Benzodiazepine withdrawal syndrome
| Benzodiazepine withdrawal syndrome | |
|---|---|
| Classification and external resources | |
| Specialty | Critical care medicine |
| ICD-10 | F13.3 |
| Benzodiazepines |
|---|
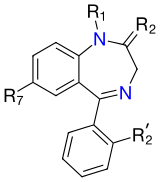 The core structure of benzodiazepines. "R" labels denote common locations of side chains, which give different benzodiazepines their unique properties. |
Benzodiazepine withdrawal syndrome—often abbreviated to benzo withdrawal—is the cluster of symptoms that emerge when a person who has taken benzodiazepines, either medically or recreationally, and has developed a physical dependence undergoes dosage reduction or discontinuation. Development of physical dependence and/or addiction and the resulting withdrawal symptoms, some of which may last for years, may result from either drug seeking behaviors or from taking the medication as prescribed. Benzodiazepine withdrawal is characterized by sleep disturbance, irritability, increased tension and anxiety, panic attacks, hand tremor, sweating, difficulty with concentration, confusion and cognitive difficulty, memory problems, dry retching and nausea, weight loss, palpitations, headache, muscular pain and stiffness, a host of perceptual changes, hallucinations, seizures, psychosis,[1] and suicide[2] (see "Signs and Symptoms" section below for full list). Further, these symptoms are notable for the manner in which they wax and wane and vary in severity from day to day or week by week instead of steadily decreasing in a straightforward monotonic manner.[3]
It is a potentially serious condition, and is complex and often protracted in time course.[4][5] Long-term use, defined as daily use for at least three months,[6] is not desirable because of the associated increased risk of dependence,[7] dose escalation, loss of efficacy, increased risk of accidents and falls, particularly for the elderly,[8] as well as cognitive,[9] neurological, and intellectual impairments.[10] Use of short-acting hypnotics, while being effective at initiating sleep, worsen the second half of sleep due to withdrawal effects.[11] Nevertheless, long-term users of benzodiazepines should not be forced to withdraw against their will.[4]
Benzodiazepine withdrawal can be severe and can provoke life-threatening withdrawal symptoms, such as seizures,[12] particularly with abrupt or overly-rapid dosage reduction from high doses or long time users.[4] A severe withdrawal response can nevertheless occur despite gradual dose reduction, or from relatively low doses in short time users,[13] even after a single large dose in animal models.[14][15] A minority of individuals will experience a protracted withdrawal syndrome whose symptoms may persist at a sub-acute level for months, or years after cessation of benzodiazepines. The likelihood of developing a protracted withdrawal syndrome can be minimized by a slow, gradual reduction in dosage.[16]
Chronic exposure to benzodiazepines causes neural adaptations that counteract the drug's effects, leading to tolerance and dependence.[17] Despite taking a constant therapeutic dose, long-term use of benzodiazepines may lead to the emergence of withdrawal-like symptoms, particularly between doses.[18] When the drug is discontinued or the dosage reduced, withdrawal symptoms may appear and remain until the body reverses the physiological adaptations.[19] These rebound symptoms may be identical to the symptoms for which the drug was initially taken, or may be part of discontinuation symptoms.[20] In severe cases, the withdrawal reaction may exacerbate or resemble serious psychiatric and medical conditions, such as mania, schizophrenia, and, especially at high doses, seizure disorders.[21] Failure to recognize discontinuation symptoms can lead to false evidence for the need to take benzodiazepines, which in turn leads to withdrawal failure and reinstatement of benzodiazepines, often to higher doses.[21]
Awareness of the withdrawal reactions, individualized taper strategies according to withdrawal severity, the addition of alternative strategies such as reassurance and referral to benzodiazepine withdrawal support groups, all increase the success rate of withdrawal.[22][23]
Signs and symptoms
Withdrawal effects caused by sedative-hypnotics discontinuation, such as benzodiazepines, barbiturates, or alcohol, can cause serious medical complications. They are cited to be more hazardous to withdraw from than opioids.[24] Users typically receive little advice and support for discontinuation.[25] Some withdrawal symptoms are identical to the symptoms for which the medication was originally prescribed,[20] and can be acute or protracted in duration. Onset of symptoms from long half-life benzodiazepines might be delayed for up to three weeks, although withdrawal symptoms from short-acting ones often present early, usually within 24–48 hours.[26] There may be no fundamental differences in symptoms from either high or low dose discontinuation, but symptoms tend to be more severe from higher doses.[27]
Daytime reemergence and rebound withdrawal symptoms, sometimes called interdose withdrawal, may occur once dependence has set in. Reemergence is the return of symptoms for which the drug was initially prescribed, in contrast, rebound symptoms are a return of the symptoms for which the benzodiazepine was initially taken for, but at a more intense level than before. Withdrawal symptoms, on the other hand, may appear for the first time during dose reduction, and include insomnia, anxiety, distress, weight loss, panic, depression, derealization, and paranoia, and are more commonly associated with short-acting benzodiazepines discontinuation, like triazolam.[21][28] Daytime symptoms can occur after a few days to a few weeks of administration of nightly benzodiazepine use[29][30] or z-drugs such as zopiclone;[31] withdrawal-related insomnia rebounds worse than baseline[32][33] even when benzodiazepines are used intermittently.[34]
The following symptoms may emerge during gradual or abrupt dosage reduction:
- Aches and pains[35]
- Agitation and restlessness[35]
- Akathisia
- Anxiety, possible terror and panic attacks[1][35]
- Blurred vision[35]
- Chest pain[35]
- Depersonalization[36]
- Depression (can be severe),[37] possible suicidal ideation
- Derealisation (feelings of unreality)[38]
- Diarrhea
- Dilated pupils[21]
- Dizziness[35]
- Double vision
- Dry mouth[35]
- Dysphoria[39][40]
- Electric shock sensations[4][41]
- Elevation in blood pressure[42]
- Fatigue and weakness[35]
- Flu-like symptoms[35]
- gastrointestinal problems [43][43][44]
- Hearing impairment[35]
- Headache[1]
- Hot and cold spells[35]
- Hyperosmia[45]
- Hypertension[46]
- Hypnagogia-hallucinations[16]
- Hypochondriasis[35]
- Increased sensitivity to touch[38]
- Increased sensitivity to sound[35]
- Increased urinary frequency[35]
- Indecision[35]
- Insomnia[47]
- Impaired concentration[1]
- Impaired memory and concentration[35]
- Loss of appetite and weight loss[48]
- Metallic taste[45]
- Mild to moderate Aphasia[45]
- Mood swings[35]
- Muscular spasms, cramps or fasciculations[49]
- Nausea and vomiting[47]
- Nightmares[47]
- Numbness and tingling[35]
- Obsessive compulsive disorder[50][51]
- Paraesthesia[38][45]
- Paranoia[45]
- Perception that stationary objects are moving[38]
- Perspiration[1]
- Photophobia[45]
- Postural hypotension[47]
- REM sleep rebound[52]
- Restless legs syndrome[23]
- Sounds louder than usual[38]
- Stiffness[35]
- Taste and smell disturbances[35]
- Tachycardia[53]
- Tinnitus[54]
- Tremor[55][56]
- Visual disturbances
Rapid discontinuation may result in a more serious syndrome
- Catatonia, which may result in death[57][58][59]
- Confusion[60]
- Convulsions, which may result in death[61][62]
- Coma[63] (rare)
- Delirium tremens[64][65][65]
- Delusions[66]
- Hallucinations
- Hyperthermia[47]
- homicidal ideations[67]
- Mania[68][69]
- Neuroleptic malignant syndrome-like event[70][71] (rare)
- Organic brain syndrome[72]
- Post-traumatic stress disorder[23]
- Psychosis[73][74]
- Suicidal ideation[75]
- Suicide[2][27][76]
- Urges to shout, throw, break things or harm someone[35]
- Violence[77]
As withdrawal progresses, patients often find their physical and mental health improves with improved mood and improved cognition.
Mechanism
The neuroadaptive processes involved in tolerance, dependence, and withdrawal mechanisms implicate both the GABAergic and the glutamatergic systems.[17] Gamma-Aminobutyric acid (GABA) is the major inhibitory neurotransmitter of the central nervous system; roughly one-quarter to one-third of synapses use GABA.[78] GABA mediates the influx of chloride ions through ligand-gated chloride channels called GABAA receptors. When chloride enters the nerve cell, the cell membrane potential hyperpolarizes thereby inhibiting depolarization, or reduction in the firing rate of the post-synaptic nerve cell.[79] Benzodiazepine potentiates the action of GABA,[80] by binding a site between the α and γ subunits of the 5-subunit receptor[81] thereby increasing the frequency of the GABA-gated chloride channel opening in the presence of GABA.[82]
When potentiation is sustained by long-term use, neuroadaptations occur which result in decreased GABAergic response. What is certain is that surface GABAA receptor protein levels are altered in response to benzodiazepine exposure, as is receptor turnover rate.[83] The exact reason for the reduced responsiveness has not been elucidated but down-regulation of the number of receptors has only been observed at some receptor locations including in the pars reticulata of the substantia nigra; down-regulation of the number of receptors or internalization does not appear to be the main mechanism at other locations.[84] Evidence exists for other hypotheses including changes in the receptor conformation, changes in turnover, recycling, or production rates, degree of phosphorylation and receptor gene expression, subunit composition, decreased coupling mechanisms between the GABA and benzodiazepine site, decrease in GABA production, and compensatory increased gutamatergic activity.[17][83] A unified model hypothesis involves a combination of internalization of the receptor, followed by preferential degradation of certain receptor sub-units, which provides the nuclear activation for changes in receptor gene transcription.[83]
It has been postulated that when benzodiazepines are cleared from the brain, these neuroadaptations are "unmasked", leading to unopposed excitability of the neuron.[85] Glutamate is the most abundant excitatory neurotransmitter in the vertebrate nervous system.[86] Increased glutamate excitatory activity during withdrawal may lead to sensitization or kindling of the CNS, possibly leading to worsening cognition and symptomatology and making each subsequent withdrawal period worse.[87][88][89] Those who have a prior history of withdrawing from benzodiazepines are found to be less likely to succeed the next time around.[90]
Diagnosis
In severe cases, the withdrawal reaction or protracted withdrawal may exacerbate or resemble serious psychiatric and medical conditions, such as mania, schizophrenia, agitated depression, panic disorder, generalised anxiety disorder, and complex partial seizures and, especially at high doses, seizure disorders.[21] Failure to recognize discontinuation symptoms can lead to false evidence for the need to take benzodiazepines, which in turn leads to withdrawal failure and reinstatement of benzodiazepines, often to higher doses. Pre-existing disorder or other causes typically do not improve, where as symptoms of protracted withdrawal gradually improve over the ensuing months.[21] For this reason at least six months should have elapsed after benzodiazepines cessation before re-evaluating the symptoms and updating a diagnosis.
Symptoms may lack a psychological cause and can fluctuate in intensity with periods of good and bad days until eventual recovery.[91][92]
Prevention
According to the British National Formulary, it is better to withdraw too slowly rather than too quickly from benzodiazepines.[26] The rate of dosage reduction is best carried out so as to minimize the symptoms' intensity and severity. Anecdotally, a slow rate of reduction may reduce the risk of developing a severe protracted syndrome.
Long half-life benzodiazepines like diazepam or chlordiazepoxide are preferred to minimize rebound effects, and are available in low potency dose forms. Some people may not fully stabilize between dose reductions, even when the rate of reduction is slowed. Such people sometimes simply need to persist as they may not feel better until they have been fully withdrawn from them for a period of time.[93]
Management
Psychological interventions may provide a small but significant additional benefit over gradual dose reduction alone at post-cessation and at follow-up.[94] The psychological interventions studied were relaxation training, cognitive-behavioral treatment of insomnia, and self-monitoring of consumption and symptoms, goal-setting, management of withdrawal and coping with anxiety.[94]
With sufficient motivation and the proper approach, almost anyone can successfully withdraw from benzodiazepines. However, a prolonged and severe syndrome can lead to collapsed marriages, business failures, bankruptcy, committal to a hospital, and the most serious adverse effect, suicide.[2] As such, long-term users should not be forced to discontinue against their will.[4] Over-rapid withdrawal, lack of explanation, and failure to reassure individuals that they are experiencing temporary withdrawal symptoms led some people to experience increased panic and fears they are going mad, with some people developing a condition similar to post-traumatic stress disorder as a result. A slow withdrawal regimen, coupled with reassurance from family, friends, and peers improves the outcome.[4][16]
Medications and interactions
While some substitutive pharmacotherapies may have promise, current evidence is insufficient to support their use.[94] Some studies found that the abrupt substitution of substitutive pharmacotherapy was actually less effective than gradual dose reduction alone, and only three studies found benefits of adding either melatonin,[95] paroxetine,[96] or trazodone and valproate[97] in conjunction with a gradual dose reduction.[94]
- Antipsychotics are generally ineffective for benzodiazepine withdrawal-related psychosis.[41][98] Antipsychotics should be avoided during benzodiazepine withdrawal as they tend to aggravate withdrawal symptoms, including convulsions.[26][99][100][101] Some antipsychotic agents may be more risky during withdrawal than others, especially clozapine, olanzapine or low potency phenothiazines (e.g., chlorpromazine), as they lower the seizure threshold and can worsen withdrawal effects; if used, extreme caution is required.[102]
- Barbiturates are cross tolerant to benzodiazepines and should be avoided.
- Benzodiazepines or cross tolerant drugs should be avoided after discontinuation, even occasionally. These include the nonbenzodiazepines Z-drugs, which have a similar mechanism of action. This is because tolerance to benzodiazepines has been demonstrated to be still present at four months to two years after withdrawal depending on personal biochemistry. Re-exposures to benzodiazepines typically resulted in a reactivation of the tolerance and benzodiazepine withdrawal syndrome.[103][104]
- Bupropion, which is used primarily as an antidepressant and smoking cessation aid, is contraindicated in persons experiencing abrupt withdrawal from benzodiazepines or other sedative-hypnotics (e.g. alcohol), due to an increased risk of seizures.[105]
- Buspirone augmentation was not found to increase the discontinuation success rate.[6]
- Caffeine may worsen withdrawal symptoms because of its stimulatory properties.[4] Interestingly, at least one animal study has shown some modulation of the benzodiazepine site by caffeine, which produces a lowering of seizure threshold.[106]
- Carbamazepine, an anticonvulsant, appears to have some beneficial effects in the treatment and management of benzodiazepine withdrawal, however, research is limited and thus the ability of experts to make recommendations on its use for benzodiazepine withdrawal is not possible at present.[103]
- Ethanol, the primary alcohol in alcoholic beverages, even mild to moderate use, has been found to be a significant predictor of withdrawal failure, probably because of its cross tolerance with benzodiazepines.[4][103][107]
- Flumazenil has been found to stimulate the reversal of tolerance and the normalization of receptor function. However, further research is needed in the form of randomised trials to demonstrate its role in the treatment of benzodiazepine withdrawal.[108] Flumazenil stimulates the up-regulation and reverses the uncoupling of benzodiazepine receptors to the GABAA receptor, thereby reversing tolerance and reducing withdrawal symptoms and relapse rates.[109][110] Limited research and experience and possible risks involved, the flumazenil detoxification method is controversial and can only be done as an inpatient procedure under medical supervision.
- Flumazenil was found to be more effective than placebo in reducing feelings of hostility and aggression in patients who had been free of benzodiazepines for 4-266 weeks.[111] This may suggest a role for flumazenil in treating protracted benzodiazepine withdrawal symptoms.
- A study into the effects of the benzodiazepine receptor antagonist, flumazenil, on benzodiazepine withdrawal symptoms persisting after withdrawal was carried out by Lader and Morton. Study subjects had been benzodiazepine-free for between one month and five years, but all reported persisting withdrawal effects to varying degrees. Persistent symptoms included clouded thinking, tiredness, muscular symptoms such as neck tension, depersonalisation, cramps and shaking and the characteristic perceptual symptoms of benzodiazepine withdrawal, namely, pins and needles feeling, burning skin, pain and subjective sensations of bodily distortion. Therapy with 0.2–2 mg of flumazenil intravenously was found to decrease these symptoms in a placebo-controlled study. This is of interest as benzodiazepine receptor antagonists are neutral and have no clinical effects. The author of the study suggested the most likely explanation is past benzodiazepine use and subsequent tolerance had locked the conformation of the GABA-BZD receptor complex into an inverse agonist conformation, and the antagonist flumazenil resets benzodiazepine receptors to their original sensitivity. Flumazenil was found in this study to be a successful treatment for protracted benzodiazepine withdrawal syndrome, but further research is required.[112] A study by Professor Borg in Sweden produced similar results in patients suffering from protracted withdrawal.[35] In 2007, Hoffmann–La Roche the makers of flumazenil, acknowledged the existence of protracted benzodiazepine withdrawal syndromes, but did not recommended flumazenil to treat the condition.[113]
- Fluoroquinolone antibiotics[114][115][116] have been noted by Heather Ashton and other authors as increasing the incidence of a CNS toxicity from 1 to 4% in the general population, for benzodiazepine-dependent population or in those undergoing withdrawal from them. This is probably the result of their GABA antagonistic effects as they have been found to competitively displace benzodiazepines from benzodiazepine receptor sites. This antagonism can precipitate acute withdrawal symptoms, that can persist for weeks or months before subsiding. The symptoms include depression, anxiety, psychosis, paranoia, severe insomnia, parathesia, tinnitus, hypersensitivity to light and sound, tremors, status epilepticus, suicidal thoughts and suicide attempt. Fluoroquinolone antibiotics should be contraindicated in patients who are dependent on or in benzodiazepine withdrawal.[4][117][118][119][120] NSAIDs have some mild GABA antagonistic properties and animal research indicate that some may even displace benzodiazepines from their binding site. However, NSAIDs taken in combination with fluoroquinolones cause a very significant increase in GABA antagonism, GABA toxicity, seizures, and other severe adverse effects.[121][122][123]
- Gabapentin can relieve most of the discomfort of benzodiazepine withdrawal; including anxiety, insomnia, irritability, tremor and muscle spasms. However, gabapentin may give rise to its own withdrawal syndrome upon discontinuation if taken continuously for long periods.
- Imidazenil has received some research for management of benzodiazepine withdrawal, but is not currently used in withdrawal.[124]
- Imipramine was found to statistically increase the discontinuation success rate.[6]
- Melatonin augmentation was found to statistically increase the discontinuation success rate for people with insomnia.[6]
- Phenibut may help with the anxiety, insomnia and muscle tension brought on by benzodiazepine discontinuation. However, there is a commonly known 'rebound' effect felt with Phenibut that may be exacerbated for people in withdrawal, it is also not recommended to be taken for more than 3 consecutive days to avoid developing a dependency.
- Phenobarbital, (a barbiturate), is used at "detox" or other inpatient facilities to prevent seizures during rapid withdrawal or cold turkey. The phenobarbital is followed by a one- to two-week taper, although a slow taper from phenobarbital is preferred.[21] In a comparison study, a rapid taper using benzodiazepines was found to be superior to a phenobarbital rapid taper.[125][126]
- Pregabalin may help reduce the severity of benzodiazepine withdrawal symptoms,[127] and reduce the risk of relapse.[128]
- Progesterone has been found to be ineffective for managing benzodiazepine withdrawal.[108]
- Propranolol was not found to increase the discontinuation success rate.[6]
- SSRI antidepressants have been found to have little value in the treatment of benzodiazepine withdrawal.[129]
- Tramadol has been found to lower the seizure threshold and should be avoided during benzodiazepine withdrawal.
- Trazodone was not found to increase the discontinuation success rate.[6]
Prognosis
The success rate of a minimal intervention where rapid withdrawal is first tried, followed by a systematic tapered discontinuation if the first try was unsuccessful, ranges from 25 to 100% with a median of 58%.[6] Cognitive behavioral therapy was useful to improve success rates for panic disorder, melatonin for insomnia, as was flumazenil and sodium valproate.[6] A ten-year follow-up found that more than half of those who had successfully withdrawn from long-term use were still abstinent two years later, and that if they were able to maintain this state at two years, they were likely to maintain this state at the ten-year followup.[8] One study found that after one year of abstinence from long-term use of benzodiazepines, cognitive, neurological and intellectual impairments had returned to normal.[130]
Those who had a prior psychiatric diagnosis had a similar success rate from a gradual taper at a two-year follow-up.[93][131] Withdrawal from benzodiazepines did not lead to an increased use of antidepressants.[132]
Withdrawal process
It can be too difficult to withdraw from short- or intermediate-acting benzodiazepines because of the intensity of the rebound symptoms felt between doses.[4][133][134][135] Moreover, short-acting benzodiazepines appear to produce a more intense withdrawal syndrome.[136] For this reason, discontinuation is sometimes carried out by first substituting an equivalent dose of a short-acting benzodiazepine to a longer-acting one like diazepam or chlordiazepoxide. Failure to use the correct equivalent amount can precipitate a severe withdrawal reaction.[137] Benzodiazepines with a half-life of more than 24 hours include chlordiazepoxide, diazepam, clobazam, clonazepam, chlorazepinic acid, flurazepam, ketazolam, medazepam, nordazepam, and prazepam. Benzodiazepines with a half-life of less than 24 hours include alprazolam, bromazepam, brotizolam, flunitrazepam, loprazolam, lorazepam, lormetazepam, midazolam, nitrazepam, oxazepam, and temazepam.[8] The resultant equivalent dose is then gradually reduced. The reduction rate used in the Heather Ashton protocol calls for eliminating 10% of the remaining dose every two to four weeks, depending on the severity and response to reductions with the final dose at 0.5 mg dose of diazepam or 5 mg dose of chlordiazepoxide.[4]
Duration
After the last dose has been taken, the acute phase of the withdrawal generally lasts for about two months. Withdrawal symptoms, even from low-dose use, typically persist for six to twelve months and gradually improve over that period,[27][93] however, clinically significant withdrawal symptoms may persist for years, although gradually declining.
A clinical trial of patients taking the benzodiazepine alprazolam for as short as eight weeks triggered protracted symptoms of memory deficits which were still present up to eight weeks after cessation of alprazolam.[138]
Protracted withdrawal syndrome
Protracted withdrawal syndrome refers to symptoms persisting for months or even years. A significant minority of people withdrawing from benzodiazepines, perhaps 10 to 15%, experience a protracted withdrawal syndrome which can sometimes be severe. Symptoms may include tinnitus,[54][139] psychosis, cognitive deficits, gastrointestinal complaints, insomnia, paraesthesia (tingling and numbness), pain (usually in limbs and extremities), muscle pain, weakness, tension, painful tremor, shaking attacks, jerks, and blepharospasm[16] and may occur even without a pre-existing history of these symptoms. Tinnitus occurring during dose reduction or discontinuation of benzodiazepines is alleviated by recommencement of benzodiazepines.
A study testing neuropsychological factors found psychophysiological markers differering from normals, and concluded that protracted withdrawal syndrome was a genuine iatrogenic condition caused by the long-term use.[140] The causes of persisting symptoms are a combination of pharmacological factors such as persisting drug induced receptor changes, psychological factors both caused by the drug and separate from the drug and possibly in some cases, particularly high dose users, structural brain damage or structural neuronal damage.[16][141] Symptoms continue to improve over time, often to the point where people eventually resume their normal lives, even after years of incapacity.[4]
A slow withdrawal rate significantly reduces the risk of a protracted and/or severe withdrawal state. Protracted withdrawal symptoms can be punctuated by periods of good days and bad days. When symptoms increase periodically during protracted withdrawal, physiological changes may be present, including dilated pupils as well as an increase in blood pressure and heart rate.[21] The change in symptoms has been proposed to be due to changes in receptor sensitivity for GABA during the process of tolerance reversal.[4] A meta-analysis found cognitive impairments due to benzodiazepine use show improvements after six months of withdrawal, but the remaining cognitive impairments may be permanent or may require more than six months to reverse.[142]
Protracted symptoms continue to fade over a period of many months or several years. There is no known cure for protracted benzodiazepine withdrawal syndrome except time,[16] however, the medication flumazenil was found to be more effective than placebo in reducing feelings of hostility and aggression in patients who had been free of benzodiazepines for 4–266 weeks.[111] This may suggest a role for flumazenil in treating protracted benzodiazepine withdrawal symptoms.
Epidemiology
The severity and length of the withdrawal syndrome is likely determined by various factors, including rate of tapering, length of use and dosage size, and possible genetic factors.[4][143] Those who have a prior history of withdrawing from benzodiazepines may have a sensitized or kindled central nervous system leading to worsening cognition and symptomatology, and making each subsequent withdrawal period worse.[87][88][89][144]
Special populations
Pediatrics
A neonatal withdrawal syndrome, sometimes severe, can occur when the mother had taken benzodiazepines, especially during the third trimester. Symptoms include hypotonia, apnoeic spells, cyanosis, and impaired metabolic responses to cold stress and seizures. The neonatal benzodiazepine withdrawal syndrome has been reported to persist from hours to months after birth.[145]
A withdrawal syndrome is seen in about 20% of pediatric intensive care unit children after infusions with benzodiazepines or opioids.[146] The likelihood of having the syndrome correlates with total infusion duration and dose, although duration is thought to be more important.[147] Treatment for withdrawal usually involves weaning over an 3 to 21 day period if the infusion lasted for more than a week.[148] Symptoms include tremors, agitation, sleeplessness, inconsolable crying, diarrhea and sweating. In total, over fifty withdrawal symptoms are listed in this review article.[146][149] Environmental measures aimed at easing the symptoms of neonates with severe abstinence syndrome had little impact, but providing a quiet sleep environment helped in mild cases.[146]
Pregnancy
Discontinuing benzodiazepines or antidepressants abruptly due to concerns of teratogenic effects of the medications has a high risk of causing serious complications, so is not recommended. For example, abrupt withdrawal of benzodiazepines or antidepressants has a high risk of causing extreme withdrawal symptoms, including suicidal ideation and a severe rebound effect of the return of the underlying disorder if present. This can lead to hospitalisation and potentially, suicide. One study reported one-third of mothers who suddenly discontinued or very rapidly tapered their medications became acutely suicidal due to 'unbearable symptoms'. One woman had a medical abortion, as she felt she could no longer cope, and another woman used alcohol in a bid to combat the withdrawal symptoms from benzodiazepines. Spontaneous abortions may also result from abrupt withdrawal of psychotropic medications, including benzodiazepines. The study reported physicians generally are not aware of the severe consequences of abrupt withdrawal of psychotropic medications such as benzodiazepines or antidepressants.[75]
The elderly
A study of the elderly who were benzodiazepine dependent found withdrawal could be carried out with few complications and could lead to improvements in sleep and cognitive abilities. At 52 weeks after successful withdrawal, a 22% improvement in cognitive status was found, as well as improved social functioning. Those who remained on benzodiazepines experienced a 5% decline in cognitive abilities, which seemed to be faster than that seen in normal aging, suggesting the longer the intake of benzodiazepines, the worse the cognitive effects become. Some worsening of symptoms were seen in the first few months of benzodiazepine abstinence, but at a 24-week followup, elderly subjects were clearly improved compared to those who remained on benzodiazepines. Improvements in sleep were seen at the 24- and 52-week followups. The authors concluded benzodiazepines were not effective in the long term for sleep problems except in suppressing withdrawal-related rebound insomnia. Improvements were seen between 24 and 52 weeks after withdrawal in many factors, including improved sleep and several cognitive and performance abilities. Some cognitive abilities, which are sensitive to benzodiazepines, as well as age, such as episodic memory did not improve. The authors, however, cited a study in younger patients who at a 3.5-year followup showed no memory impairments and speculated that certain memory functions take longer to recover from chronic benzodiazepine use and further improvements in elderly people's cognitive function may occur beyond 52 weeks after withdrawal. The reason it took 24 weeks for improvements to be seen after cessation of benzodiazepine use was due to the time it takes the brain to adapt to the benzodiazepine-free environment.[150]
At 24 weeks, significant improvements were found, including accuracy of information processing improved, but a decline was seen in those who remained on benzodiazepines. Further improvements were noted at the 52-week followup, indicating ongoing improvements with benzodiazepine abstinence. Younger people on benzodiazepines also experience cognitive deterioration in visual spacial memory, but are not as vulnerable as the elderly to the cognitive effects.[150]
Improved reaction times were noted at 52 weeks in elderly patients free from benzodiazepines. This is an important function in the elderly, especially if they drive a car due to the increased risk of road traffic accidents in benzodiazepine users.[150]
At the 24-week followup, 80% of people had successfully withdrawn from benzodiazepines. Part of the success was attributed to the placebo method used for part of the trial which broke the psychological dependence on benzodiazepines when the elderly patients realised they had completed their gradual reduction several weeks previously, and had only been taking placebo tablets. This helped reassure them they could sleep without their pills.[150]
The authors also warned of the similarities in pharmacology and mechanism of action of the newer nonbenzodiazepine Z drugs.[150]
The elimination half-life of diazepam and chlordiazepoxide, as well as other long half-life benzodiazepines, is twice as long in the elderly compared to younger individuals. Many doctors do not adjust benzodiazepine dosage according to age in elderly patients.[151]
Controversy
Detox facilities may be inappropriate for those who have become tolerant while taking the drug as prescribed, as opposed to recreational use. Such inpatient referrals may be traumatic for non-abusers.[21]
See also
References
- 1 2 3 4 5 Petursson, H. (1994). "The benzodiazepine withdrawal syndrome". Addiction 89 (11): 1455–9. doi:10.1111/j.1360-0443.1994.tb03743.x. PMID 7841856.
- 1 2 3 Colvin, Rod (26 August 2008). Overcoming Prescription Drug Addiction: A Guide to Coping and Understanding (3 ed.). United States of America: Addicus Books. pp. 74–76. ISBN 978-1-886039-88-9.
I have treated ten thousand patients for alcohol and drug problems and have detoxed approximately 1,500 patients for benzodiazepines – the detox for the benzodiazepines is one of the hardest detoxes we do. It can take an extremely long time, about half the length of time they have been addicted – the ongoing relentless withdrawals can be so incapacitating it can cause total destruction to one’s life – marriages break up, businesses are lost, bankruptcy, hospitalization, and of course suicide is probably the most single serious side effect.
- ↑ C. Heather Ashton DM. "Chapter III: Benzodiazepine withdrawal symptoms, acute & protracted". Institute of Neuroscience, Newcastle University. Retrieved 29 April 2013.
Benzodiazepines : How they work and how to withdraw
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Professor Heather Ashton (2002). "Benzodiazepines: How They Work and How to Withdraw".
- ↑ O'Connor, RD (1993). "Benzodiazepine dependence--a treatment perspective and an advocacy for control". NIDA research monograph 131: 266–9. PMID 8105385.
- 1 2 3 4 5 6 7 8 Voshaar, R. C. O.; Couvée, JE; Van Balkom, AJ; Mulder, PG; Zitman, FG (2006). "Strategies for discontinuing long-term benzodiazepine use: Meta-analysis". The British Journal of Psychiatry 189 (3): 213–20. doi:10.1192/bjp.189.3.213. PMID 16946355.
- ↑ Nutt, David (1986). "Benzodiazepine dependence in the clinic: Reason for anxiety?". Trends in Pharmacological Sciences 7: 457–60. doi:10.1016/0165-6147(86)90420-7.
- 1 2 3 De Gier, N.; Gorgels, W.; Lucassen, P.; Oude Voshaar, R.; Mulder, J.; Zitman, F. (2010). "Discontinuation of long-term benzodiazepine use: 10-year follow-up". Family Practice 28 (3): 253–9. doi:10.1093/fampra/cmq113. PMID 21193495.
- ↑ Authier, Nicolas; Boucher, Alexandra; Lamaison, Dominique; Llorca, Pierre-Michel; Descotes, Jacques; Eschalier, Alain (2009). "Second Meeting of the French CEIP (Centres d'Évaluation et d'Information sur la Pharmacodépendance). Part II: Benzodiazepine Withdrawal". Thérapie 64 (6): 365–70. doi:10.2515/therapie/2009051. PMID 20025839.
- ↑ Heberlein, A.; Bleich, S.; Kornhuber, J.; Hillemacher, T. (2008). "Benzodiazepin-Abhängigkeit: Ursachen und Behandlungsmöglichkeiten" [Benzodiazepine Dependence: Causalities and Treatment Options]. Fortschritte der Neurologie · Psychiatrie (in German) 77 (1): 7–15. doi:10.1055/s-0028-1100831. PMID 19101875.
- ↑ Lee-chiong, Teofilo (24 April 2008). Sleep Medicine: Essentials and Review. Oxford University Press, USA. p. 468. ISBN 0-19-530659-7.
- ↑ Evans, Katie; Sullivan, Michael J. (2001). "Withdrawal and Medical Issues". Dual Diagnosis: Counseling the Mentally Ill Substance Abuser (2nd ed.). Guilford Press. pp. 52–3. ISBN 978-1-57230-446-8.
- ↑ Lader, M (1987). "Long-term anxiolytic therapy: The issue of drug withdrawal". The Journal of Clinical Psychiatry. 48 Suppl: 12–6. PMID 2891684.
- ↑ Boisse, NR; Periana, RM; Guarino, JJ; Kruger, HS; Samoriski, GM (1986). "Pharmacologic characterization of acute chlordiazepoxide dependence in the rat". The Journal of Pharmacology and Experimental Therapeutics 239 (3): 775–83. PMID 3098961.
- ↑ Boisse, NR; Periana, RM; Guarino, JJ; Kruger, HS (1986). "Acute chlordiazepoxide dependence in the rat: Comparisons to chronic". NIDA research monograph 67: 197–201. PMID 3092067.
- 1 2 3 4 5 6 Professor Heather Ashton (2004). "Protracted Withdrawal Symptoms From Benzodiazepines". Comprehensive Handbook of Drug & Alcohol Addiction.
- 1 2 3 Allison, C; Pratt, J.A (2003). "Neuroadaptive processes in GABAergic and glutamatergic systems in benzodiazepine dependence". Pharmacology & Therapeutics 98 (2): 171–95. doi:10.1016/S0163-7258(03)00029-9. PMID 12725868.
- ↑ Herman, JB; Brotman, AW; Rosenbaum, JF (1987). "Rebound anxiety in panic disorder patients treated with shorter-acting benzodiazepines". The Journal of Clinical Psychiatry. 48 Suppl: 22–8. PMID 2889722.
- ↑ Allgulander, C; Bandelow, B; Hollander, E; Montgomery, SA; Nutt, DJ; Okasha, A; Pollack, MH; Stein, DJ; Swinson, RP; World Council Of, Anxiety (2003). "WCA recommendations for the long-term treatment of generalized anxiety disorder". CNS spectrums 8 (8 Suppl 1): 53–61. PMID 14767398.
- 1 2 Salzman, Carl (1993). "Benzodiazepine treatment of panic and agoraphobic symptoms: Use, dependence, toxicity, abuse". Journal of Psychiatric Research 27: 97–110. doi:10.1016/0022-3956(93)90021-S. PMID 7908335.
- 1 2 3 4 5 6 7 8 9 Gabbard, Glen O. (15 May 2007). Gabbard's Treatments of Psychiatric Disorders, Fourth Edition (Treatments of Psychiatric Disorders). American Psychiatric Publishing. pp. 209–211. ISBN 1-58562-216-8.
- ↑ Onyett, SR (1989). "The benzodiazepine withdrawal syndrome and its management". The Journal of the Royal College of General Practitioners 39 (321): 160–3. PMC 1711840. PMID 2576073.
- 1 2 3 Ashton, Heather (1991). "Protracted withdrawal syndromes from benzodiazepines". Journal of Substance Abuse Treatment 8 (1–2): 19–28. doi:10.1016/0740-5472(91)90023-4. PMID 1675688.
- ↑ Lindsay, S.J.E.; Powell, Graham E., eds. (28 July 1998). The Handbook of Clinical Adult Psychology (2nd ed.). Routledge. p. 363. ISBN 978-0-415-07215-1.
- ↑ Authier, N.; Balayssac, D.; Sautereau, M.; Zangarelli, A.; Courty, P.; Somogyi, A.A.; Vennat, B.; Llorca, P.-M.; Eschalier, A. (2009). "Benzodiazepine dependence: Focus on withdrawal syndrome". Annales Pharmaceutiques Françaises 67 (6): 408–13. doi:10.1016/j.pharma.2009.07.001. PMID 19900604.
- 1 2 3 Committee on Safety of Medicines (2007). "Hypnotics and anxiolytics". British National Formulary. Retrieved 17 September 2007.(registration required)
- 1 2 3 Murphy, S. M.; Tyrer, P. (1991). "A double-blind comparison of the effects of gradual withdrawal of lorazepam, diazepam and bromazepam in benzodiazepine dependence". The British Journal of Psychiatry 158 (4): 511–6. doi:10.1192/bjp.158.4.511. PMID 1675901.
- ↑ Adam, Kirstine; Oswald, I. (2008). "Can a Rapidly-eliminated Hypnotic Cause Daytime Anxiety?". Pharmacopsychiatry 22 (3): 115–9. doi:10.1055/s-2007-1014592. PMID 2748714.
- ↑ Scharf, Martin B; Kales, Judith A; Bixler, EO; Jacoby, JA; Schweitzer, PK (1982). "Lorazepam—Efficacy, side effects, and rebound phenomena". Clinical Pharmacology and Therapeutics 31 (2): 175–9. doi:10.1038/clpt.1982.27. PMID 6120058.
- ↑ Walsh, James K; Schweitzer, Paula K; Parwatikar, Sadashiv (1983). "Effects of lorazepam and its withdrawal on sleep, performance, and subjective state". Clinical Pharmacology and Therapeutics 34 (4): 496–500. doi:10.1038/clpt.1983.203. PMID 6617072.
- ↑ Fontaine, Réjean; Beaudry, Paul; Le Morvan, Patrick LE; Beauclair, Linda; Chouinard, GUY (1990). "Zopiclone and Triazolam in Insomnia Associated with Generalized Anxiety Disorder". International Clinical Psychopharmacology 5 (3): 173–83. doi:10.1097/00004850-199007000-00002. PMID 2230061.
- ↑ Kales, Anthony; Bixler, Edward O.; Soldatos, Constantin R.; Jacoby, Judith A.; Kales, Joyce D. (1986). "Lorazepam: Effects on Sleep and Withdrawal Phenomena". Pharmacology 32 (3): 121–30. doi:10.1159/000138160. PMID 3960963.
- ↑ Bonnet, M H; Arand, D L (1999). "The use of lorazepam TID for chronic insomnia". International Clinical Psychopharmacology 14 (2): 81–9. doi:10.1097/00004850-199903000-00004. PMID 10220122.
- ↑ Kales, Anthony; Manfredi, Rocco L; Vgontzas, Alexandras N; Bixler, Edward O; Vela-Bueno, Antonio; Fee, Eric C (1991). "Rebound insomnia after only brief and intermittent use of rapidly eliminated benzodiazepines". Clinical Pharmacology and Therapeutics 49 (4): 468–76. doi:10.1038/clpt.1991.55. PMID 2015735.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Saxon, L.; Hjemdahl, P.; Hiltunen, A. J.; Borg, S. (1997). "Effects of flumazenil in the treatment of benzodiazepine withdrawal - a double-blind pilot study". Psychopharmacology 131 (2): 153–60. doi:10.1007/s002130050278. PMID 9201803.
- ↑ Terao, T; Yoshimura, R; Terao, M; Abe, K (1992). "Depersonalization following nitrazepam withdrawal". Biological Psychiatry 31 (2): 212–3. doi:10.1016/0006-3223(92)90209-I. PMID 1737083.
- ↑ Lader, Malcolm (1994). "Anxiety or depression during withdrawal of hypnotic treatments". Journal of Psychosomatic Research 38: 113–23; discussion 118–23. doi:10.1016/0022-3999(94)90142-2. PMID 7799243.
- 1 2 3 4 5 Mintzer, M. Z.; Stoller, K. B.; Griffiths, R. R. (1999). "A controlled study of flumazenil-precipitated withdrawal in chronic low-dose benzodiazepine users". Psychopharmacology 147 (2): 200–9. doi:10.1007/s002130051161. PMID 10591888.
- ↑ Mendelson, WB; Weingartner, H; Greenblatt, DJ; Garnett, D; Gillin, JC (1982). "A clinical study of flurazepam". Sleep 5 (4): 350–60. PMID 6761826.
- ↑ Schöpf, J. (2008). "Withdrawal Phenomena after Long-term Administration of Benzodiazepines a Review of Recent Investigations". Pharmacopsychiatry 16 (1): 1–8. doi:10.1055/s-2007-1017439. PMID 6131447.
- 1 2 Shader, RI; Greenblatt, DJ (1981). "The use of benzodiazepines in clinical practice". British Journal of Clinical Pharmacology. 11 Suppl 1 (Suppl 1): 5S–9S. doi:10.1111/j.1365-2125.1981.tb01832.x. PMC 1401641. PMID 6133535.
- ↑ Mintzer, Miriam Z.; Griffiths, Roland R. (2004). "Flumazenil-precipitated withdrawal in healthy volunteers following repeated diazepam exposure". Psychopharmacology 178 (2–3): 259–67. doi:10.1007/s00213-004-2009-1. PMID 15452683.
- 1 2 Loeb, P; Adnet, P; Boittiaux, P; Forget, AP; Mille, FX (1997). "Sevrage en benzodiazépines révélé par un syndrome douloureux abdominal pseudochirurgical" [Benzodiazepine withdrawal masquerading as surgical abdominal syndrome]. Annales Françaises d'Anesthésie et de Réanimation (in French) 16 (5): 521–2. doi:10.1016/S0750-7658(97)83345-X.
- ↑ http://www.benzo.org.uk/manual/bzcha03.htm#16[]
- 1 2 3 4 5 6 Pelissolo, A; Bisserbe, JC (1994). "Dependence on benzodiazepines. Clinical and biological aspects". L'Encephale 20 (2): 147–57. PMID 7914165.
- ↑ Biswas, AK; Feldman, BL; Davis, DH; Zintz, EA (2005). "Myocardial ischemia as a result of severe benzodiazepine and opioid withdrawal". Clinical toxicology (Philadelphia, Pa.) 43 (3): 207–9. doi:10.1081/clt-200053099. PMID 15902797.
- 1 2 3 4 5 Bismuth, C; Le Bellec, M; Dally, S; Lagier, G (1980). "Benzodiazepine physical dependence. 6 cases (author's transl)". La Nouvelle presse medicale 9 (28): 1941–5. PMID 6106922.
- ↑ Pecknold, J.C. (1993). "Discontinuation reactions to alprazolam in panic disorder". Journal of Psychiatric Research 27: 155–170. doi:10.1016/0022-3956(93)90025-W.
- ↑ Kliniska Färdigheter: Informationsutbytet Mellan Patient Och Läkare, LINDGREN, STEFAN, ISBN 91-44-37271-X (Swedish)
- ↑ Drummond, Lynne M.; Matthews, Helen P. (1988). "SINGLE CASE STUDY Obsessive-Compulsive Disorder Occurring as a Complication in Benzodiazepine Withdrawal". The Journal of Nervous and Mental Disease 176 (11): 688–91. doi:10.1097/00005053-198811000-00008. PMID 3183654.
- ↑ Matthews, HP; Drummond, LM (1987). "Obsessive-compulsive disorder--a complication of benzodiazepine withdrawal". The British Journal of Psychiatry 150: 272. PMID 3651695.
- ↑ Pagel, J. F.; Parnes, Bennett L. (2001). "Medications for the Treatment of Sleep Disorders". The Primary Care Companion to the Journal of Clinical Psychiatry 3 (3): 118–125. doi:10.4088/PCC.v03n0303. PMC 181172. PMID 15014609.
- ↑ Van Engelen, BG; Gimbrere, JS; Booy, LH (1993). "Benzodiazepine withdrawal reaction in two children following discontinuation of sedation with midazolam". The Annals of pharmacotherapy 27 (5): 579–81. PMID 8347907.
- 1 2 Beeley, L (1991). "Benzodiazepines and tinnitus". BMJ 302 (6790): 1465. doi:10.1136/bmj.302.6790.1465.
- ↑ Mellor, CS; Jain, VK (1982). "Diazepam withdrawal syndrome: Its prolonged and changing nature". Canadian Medical Association journal 127 (11): 1093–6. PMC 1862031. PMID 7139456.
- ↑ Olajide, Dele; Lader, Malcolm (2009). "Depression following withdrawal from long-term benzodiazepine use: A report of four cases". Psychological Medicine 14 (4): 937–40. doi:10.1017/S0033291700019899. PMID 6152745.
- ↑ Rosebush, Patricia I.; Mazurek, Michael F. (1996). "Catatonia After Benzodiazepine Withdrawal". Journal of Clinical Psychopharmacology 16 (4): 315–9. doi:10.1097/00004714-199608000-00007. PMID 8835707.
- ↑ Deuschle, M.F.; Lederbogen, F (2001). "Benzodiazepine Withdrawal - Induced Catatonia". Pharmacopsychiatry 34 (1): 41–2. doi:10.1055/s-2001-15188. PMID 11229621.
- ↑ Kanemoto, Kousuke; Miyamoto, Toshio; Abe, Ryuji (1999). "Ictal catatonia as a manifestation of de novo absence status epilepticus following benzodiazepine withdrawal". Seizure 8 (6): 364–6. doi:10.1053/seiz.1999.0309. PMID 10512781.
- ↑ Uhlenhuth EH; Starcevic V; Qualls C; Antal EJ; Matuzas W; Javaid JI; Barnhill J (October 2006). "Abrupt discontinuation of alprazolam and cognitive style in patients with panic disorder: early effects on mood, performance, and vital signs". J Clin Psychopharmacol 26 (5): 519–523. doi:10.1097/01.jcp.0000236653.85791.60. PMID 16974197.
- ↑ Metten, Pamela; Crabbe, John C (1999). "Genetic Determinants of Severity of Acute Withdrawal from Diazepam in Mice". Pharmacology Biochemistry and Behavior 63 (3): 473–9. doi:10.1016/S0091-3057(99)00017-9. PMID 10418790.
- ↑ Haque, W; Watson, DJ; Bryant, SG (1990). "Death following suspected alprazolam withdrawal seizures: A case report". Texas medicine 86 (1): 44–7. PMID 2300914.
- ↑ De Bard, ML (1979). "Diazepam withdrawal syndrome: A case with psychosis, seizure, and coma". The American Journal of Psychiatry 136 (1): 104–5. PMID 103443.
- ↑ Provini, F.; Cortelli, P.; Montagna, P.; Gambetti, P.; Lugaresi, E. (2008). "Fatal insomnia and agrypnia excitata: Sleep and the limbic system". Revue Neurologique 164 (8–9): 692–700. doi:10.1016/j.neurol.2007.11.003. PMID 18805303.
- 1 2 Berezak, A.; Weber, M.; Hansmann, J.; Tulasne, P.A.; Laporte, B.; Ould Ouali, A. (1984). "Dépendance physique aux benzodiazépines dans un contexte traumatologique" [Benzodiazepine physical dependence in traumatology]. Annales Françaises d'Anesthésie et de Réanimation (in French) 3 (5): 383–4. doi:10.1016/S0750-7658(84)80078-7.
- ↑ Keshavan, MS; Moodley, P; Eales, M; Joyce, E; Yeragani, VK (1988). "Delusional depression following benzodiazepine withdrawal". Canadian Journal of Psychiatry 33 (7): 626–7. PMID 3197017.
- ↑ Risse, SC; Whitters, A; Burke, J; Chen, S; Scurfield, RM; Raskind, MA (1990). "Severe withdrawal symptoms after discontinuation of alprazolam in eight patients with combat-induced posttraumatic stress disorder". The Journal of Clinical Psychiatry 51 (5): 206–9. PMID 2335496.
- ↑ Turkington, Douglas; Gill, Paul (1989). "Mania induced by lorazepam withdrawal: A report of two cases". Journal of Affective Disorders 17 (1): 93–5. doi:10.1016/0165-0327(89)90028-1. PMID 2525581.
- ↑ Lapierre, YD; Labelle, A (1987). "Manic-like reaction induced by lorazepam withdrawal". Canadian Journal of Psychiatry 32 (8): 697–8. PMID 3690487.
- ↑ Kawajiri, M; Ohyagi, Y; Furuya, H; Araki, T; Inoue, N; Esaki, S; Yamada, T; Kira, J (2002). "A patient with Parkinson's disease complicated by hypothyroidism who developed malignant syndrome after discontinuation of etizolam". Rinsho shinkeigaku 42 (2): 136–9. PMID 12424963.
- ↑ Strawn, Jeffrey; Keck Jr, PE; Caroff, SN (2007). "Neuroleptic Malignant Syndrome". American Journal of Psychiatry 164 (6): 870–6. doi:10.1176/appi.ajp.164.6.870. PMID 17541044.
- ↑ Khan, A; Joyce, P; Jones, AV (1980). "Benzodiazepine withdrawal syndromes". The New Zealand medical journal 92 (665): 94–6. PMID 6107888.
- ↑ Peh, LH; Mahendran, R (1989). "Psychiatric complications of Erimin abuse". Singapore medical journal 30 (1): 72–3. PMID 2595393.
- ↑ Fruensgaard, K. (1976). "Withdrawal Psychosis: A Study of 30 Consecutive Cases". Acta Psychiatrica Scandinavica 53 (2): 105–18. doi:10.1111/j.1600-0447.1976.tb00065.x. PMID 3091.
- 1 2 Einarson, A; Selby, P; Koren, G (2001). "Abrupt discontinuation of psychotropic drugs during pregnancy: Fear of teratogenic risk and impact of counselling". Journal of Psychiatry & Neuroscience 26 (1): 44–8. PMC 1408034. PMID 11212593.
- ↑ Joughin, N.; Tata, P.; Collins, M.; Hooper, C.; Falkowski, J. (1991). "In-patient withdrawal from long-term benzodiazepine use". Addiction 86 (4): 449–55. doi:10.1111/j.1360-0443.1991.tb03422.x. PMID 1675899.
- ↑ Citrome, Leslie; Volavka, Jan (1999). "Violent Patients in the Emergency Setting". Psychiatric Clinics of North America 22 (4): 789–801. doi:10.1016/S0193-953X(05)70126-X. PMID 10623971.
- ↑ Dubuc, Bruno. "Neurotransmitters". The Brain from Top to Bottom. Retrieved 29 April 2013.
- ↑ Tallman, J F; Gallager, D W (1985). "The Gaba-Ergic System: A Locus of Benzodiazepine Action". Annual Review of Neuroscience 8: 21–44. doi:10.1146/annurev.ne.08.030185.000321. PMID 2858999.
- ↑ Schoch, P.; Richards, J. G.; Häring, P.; Takacs, B.; Stähli, C.; Staehelin, T.; Haefely, W.; Möhler, H. (1985). "Co-localization of GABAA receptors and benzodiazepine receptors in the brain shown by monoclonal antibodies". Nature 314 (6007): 168–71. Bibcode:1985Natur.314..168S. doi:10.1038/314168a0. PMID 2983231.
- ↑ Vinkers, Christiaan H.; Olivier, Berend (2012). "Mechanisms Underlying Tolerance after Long-Term Benzodiazepine Use: A Future for Subtype-Selective GABAA Receptor Modulators?". Advances in Pharmacological Sciences 2012: 1–19. doi:10.1155/2012/416864. PMC 3321276. PMID 22536226.
- ↑ Study, R. E.; Barker, JL (1981). "Diazepam and (–)-pentobarbital: fluctuation analysis reveals different mechanisms for potentiation of γ-aminobutyric acid responses in cultured central neurons". Proceedings of the National Academy of Sciences 78 (11): 7180–4. Bibcode:1981PNAS...78.7180S. doi:10.1073/pnas.78.11.7180. JSTOR 11434. PMC 349220. PMID 6273918.
- 1 2 3 Bateson, A. (2002). "Basic Pharmacologic Mechanisms Involved in Benzodiazepine Tolerance and Withdrawal". Current Pharmaceutical Design 8 (1): 5–21. doi:10.2174/1381612023396681. PMID 11812247.
- ↑ Tietz, EI; Rosenberg, HC; Chiu, TH (1986). "Autoradiographic localization of benzodiazepine receptor downregulation". The Journal of Pharmacology and Experimental Therapeutics 236 (1): 284–92. PMID 3001290.
- ↑ Koob, G.; Bloom, F. (1988). "Cellular and molecular mechanisms of drug dependence". Science 242 (4879): 715–23. Bibcode:1988Sci...242..715K. doi:10.1126/science.2903550. PMID 2903550.
- ↑ Meldrum, Brian S. (2000). "Glutamate as a Neurotransmitter in the Brain: Review of Physiology and Pathology". The Journal of Nutrition 130 (4): 1007S–15S. PMID 10736372.
- 1 2 Stephens, D. N. (1995). "A glutamatergic hypothesis of drug dependence: extrapolations from benzodiazepine receptor ligands". Behavioural Pharmacology 6 (5): 425–46. doi:10.1097/00008877-199508000-00004. PMID 11224351.
- 1 2 Dunworth, Sarah J.; Mead, Andy N.; Stephens, David N. (2000). "Previous experience of withdrawal from chronic diazepam ameliorates the aversiveness of precipitated withdrawal and reduces withdrawal-induced c-fos expression in nucleus accumbens". European Journal of Neuroscience 12 (4): 1501–8. doi:10.1046/j.1460-9568.2000.00036.x. PMID 10762378.
- 1 2 Rickels, Karl; Schweizer, E; Csanalosi, I; Case, WG; Chung, H (1988). "Long-term Treatment of Anxiety and Risk of Withdrawal: Prospective Comparison of Clorazepate and Buspirone". Archives of General Psychiatry 45 (5): 444–50. doi:10.1001/archpsyc.1988.01800290060008. PMID 2895993.
- ↑ Vorma, Helena; Naukkarinen, Hannu H.; Sarna, Seppo J.; Kuoppasalmi, Kimmo I. (2005). "Predictors of Benzodiazepine Discontinuation in Subjects Manifesting Complicated Dependence". Substance Use & Misuse 40 (4): 499–510. doi:10.1081/JA-200052433. PMID 15830732.
- ↑ Smith, David E.; Wesson, Donald R. (1983). "Benzodiazepine Dependency Syndromes". Journal of Psychoactive Drugs 15 (1–2): 85–95. doi:10.1080/02791072.1983.10472127. PMID 6136575.
- ↑ Landry, MJ; Smith, DE; McDuff, DR; Baughman, OL (1992). "Benzodiazepine dependence and withdrawal: Identification and medical management". The Journal of the American Board of Family Practice 5 (2): 167–75. PMID 1575069.
- 1 2 3 Higgitt, A C; Lader, M H; Fonagy, P (1985). "Clinical management of benzodiazepine dependence". BMJ 291 (6497): 688–90. doi:10.1136/bmj.291.6497.688. PMC 1416639. PMID 2864096.
- 1 2 3 4 Parr, Jannette M.; Kavanagh, David J.; Cahill, Lareina; Mitchell, Geoffrey; Mcd Young, Ross McD. (2009). "Effectiveness of current treatment approaches for benzodiazepine discontinuation: A meta-analysis". Addiction 104 (1): 13–24. doi:10.1111/j.1360-0443.2008.02364.x. PMID 18983627.
- ↑ Garfinkel, Doron; Zisapel, N; Wainstein, J; Laudon, M (1999). "Facilitation of Benzodiazepine Discontinuation by Melatonin: A New Clinical Approach". Archives of Internal Medicine 159 (20): 2456–60. doi:10.1001/archinte.159.20.2456. PMID 10665894.
- ↑ Nakao, Mutsuhiro; Takeuchi, Takeaki; Nomura, Kyoko; Teramoto, Tamio; Yano, Eiji (2006). "Clinical application of paroxetine for tapering benzodiazepine use in non-major-depressive outpatients visiting an internal medicine clinic". Psychiatry and Clinical Neurosciences 60 (5): 605–10. doi:10.1111/j.1440-1819.2006.01565.x. PMID 16958945.
- ↑ Rickels, K.; Schweizer, E.; Garcia España, F.; Case, G.; Demartinis, N.; Greenblatt, D. (1999). "Trazodone and valproate in patients discontinuing long-term benzodiazepine therapy: Effects on withdrawal symptoms and taper outcome". Psychopharmacology 141 (1): 1–5. doi:10.1007/s002130050798. PMID 9952057.
- ↑ Fruensgaard, K (1977). "Withdrawal psychosis after drugs. Report of a consecutive material". Ugeskrift for laeger 139 (29): 1719–22. PMID 898354.
- ↑ Tagashira, Eijiro; Hiramori, Tameo; Urano, Tomoko; Nakao, Kenzo; Yanaura, Saizo (1981). "Enhancement of drug withdrawal convulsion by combinations of phenobarbital and antipsychotic agents". The Japanese Journal of Pharmacology 31 (5): 689–99. doi:10.1254/jjp.31.689. PMID 6118452.
- ↑ Bobolakis, Ioannis (2000). "Neuroleptic Malignant Syndrome After Antipsychotic Drug Administration During Benzodiazepine Withdrawal". Journal of Clinical Psychopharmacology 20 (2): 281–3. doi:10.1097/00004714-200004000-00033. PMID 10770479.
- ↑ Randall, Michael D; Neil, Karen E (February 2004). "5". Disease management (1 ed.). Pharmaceutical Press. p. 62. ISBN 978-0-85369-523-3. Retrieved 1 June 2009.
- ↑ Ebadi, Manuchair (23 October 2007). "Alphabetical presentation of drugs". Desk Reference for Clinical Pharmacology (2nd ed.). USA: CRC Press. p. 512. ISBN 978-1-4200-4743-1.
- 1 2 3 Lader, Malcolm; Tylee, Andre; Donoghue, John (2009). "Withdrawing Benzodiazepines in Primary Care". CNS Drugs 23 (1): 19–34. doi:10.2165/0023210-200923010-00002. PMID 19062773.
- ↑ Higgitt, A.; Fonagy, P.; Lader, M. (2009). "The natural history of tolerance to the benzodiazepines". Psychological Medicine. Monograph Supplement 13: 1–55. doi:10.1017/S0264180100000412. PMID 2908516.
- ↑ "Wellbutrin XL Prescribing Information" (PDF). GlaxoSmithKline. December 2008. Archived from the original (PDF) on 2009-03-26. Retrieved 2010-01-16.
- ↑ Seale, Thomas W.; Carney, John M.; Rennert, Owen M.; Flux, Marinus; Skolnick, Phil (1987). "Coincidence of seizure susceptibility to caffeine and to the benzodiazepine inverse agonist, DMCM, in SWR and CBA inbred mice". Pharmacology Biochemistry and Behavior 26 (2): 381–7. doi:10.1016/0091-3057(87)90133-X. PMID 3575358.
- ↑ Schweizer, Edward; Rickels, K; Case, WG; Greenblatt, DJ (1990). "Long-term Therapeutic Use of Benzodiazepines: II. Effects of Gradual Taper". Archives of General Psychiatry 47 (10): 908–15. doi:10.1001/archpsyc.1990.01810220024003. PMID 2222130.
- 1 2 Denis, Cecile; Fatseas, Melina; Lavie, Estelle; Auriacombe, Marc (2006). Denis, Cecile, ed. "Pharmacological interventions for benzodiazepine mono-dependence management in outpatient settings". Cochrane Database Syst Rev (3): CD005194. doi:10.1002/14651858.CD005194.pub2. PMID 16856084.
- ↑ Gerra, G.; Zaimovic, A.; Giusti, F.; Moi, G.; Brewer, C. (2002). "Intravenous flumazenil versus oxazepam tapering in the treatment of benzodiazepine withdrawal: A randomized, placebo-controlled study". Addiction Biology 7 (4): 385–95. doi:10.1080/1355621021000005973. PMID 14578014.
- ↑ Little, H.J. (1991). "The benzodiazepines: Anxiolytic and withdrawal effects". Neuropeptides 19: 11–4. doi:10.1016/0143-4179(91)90077-V. PMID 1679209.
- 1 2 L. Saxon, S. Borg & A. J. Hiltunen (August 2010). "Reduction of aggression during benzodiazepine withdrawal: effects of flumazenil". Pharmacology, biochemistry, and behavior 96 (2): 148–151. doi:10.1016/j.pbb.2010.04.023. PMID 20451546.
- ↑ Lader, M. H.; Morton, S. V. (1992). "A pilot study of the effects of flumazenil on symptoms persisting after benzodiazepine withdrawal". Journal of Psychopharmacology 6 (3): 357–63. doi:10.1177/026988119200600303. PMID 22291380.
- ↑ Roche USA (October 2007). "Romazicon" (PDF). Roche Pharmaceuticals USA.
- ↑ Unseld, E; G Ziegler; A Gemeinhardt; U Janssen; U Klotz (July 1990). "Possible interaction of fluoroquinolones with the benzodiazepine-GABAA-receptor complex (summary)". Br J Clin Pharmacol 30 (1): 63–70. doi:10.1111/j.1365-2125.1990.tb03744.x. PMC 1368276. PMID 2167717.
- ↑ Ashton, Heather (April 2011). "THE ASHTON MANUAL SUPPLEMENT". BENZODIAZEPINES: HOW THEY WORK AND HOW TO WITHDRAW. benzo.org.uk.
- ↑ Kamath, Ashwin (2013). "Floroquinolone induced neurotoxicity: A review" (PDF). J. Adv. Pharm. Edu. & Res. 3 (1): 16–19. Retrieved October 17, 2015.
- ↑ McConnell, John Girvan (2008). "Benzodiazepine tolerance, dependency, and withdrawal syndromes and interactions with fluoroquinolone antimicrobials". British Journal of General Practice 58 (550): 365–6. doi:10.3399/bjgp08X280317. PMC 2435654. PMID 18482496.
- ↑ Unseld, E; Ziegler, G; Gemeinhardt, A; Janssen, U; Klotz, U (1990). "Possible interaction of fluoroquinolones with the benzodiazepine-GABAA- receptor complex". British Journal of Clinical Pharmacology 30 (1): 63–70. doi:10.1111/j.1365-2125.1990.tb03744.x. PMC 1368276. PMID 2167717.
- ↑ Sternbach, Harvey; State, Rosanne (1997). "Antibiotics: Neuropsychiatric Effects and Psychotropic Interactions". Harvard Review of Psychiatry 5 (4): 214–26. doi:10.3109/10673229709000304. PMID 9427014.
- ↑ Committee on Safety of Medicines; Medicines and Healthcare products Regulatory Agency (2008). "Quinolones". United Kingdom: British National Formulary. Retrieved 16 February 2009. (registration required (help)).
- ↑ Wong, PT (1993). "Interactions of indomethacin with central GABA systems". Archives internationales de pharmacodynamie et de therapie 324: 5–16. PMID 8297186.
- ↑ Delanty, Norman (November 2001). "Medication associated seizures". Seizures: Medical Causes and Management. Humana Press. pp. 152–153. ISBN 0-89603-827-0.
- ↑ Green, M. A.; Halliwell, R. F. (1997). "Selective antagonism of the GABAAreceptor by ciprofloxacin and biphenylacetic acid". British Journal of Pharmacology 122 (3): 584–90. doi:10.1038/sj.bjp.0701411. PMC 1564969. PMID 9351519.
- ↑ Auta, J; Costa, E; Davis, J; Guidotti, A (2005). "Imidazenil: An antagonist of the sedative but not the anticonvulsant action of diazepam". Neuropharmacology 49 (3): 425–9. doi:10.1016/j.neuropharm.2005.04.005. PMID 15964602.
- ↑ Sullivan, Mark; Toshima, Michelle; Lynn, Pamela; Roy-Byrne, Peter (1993). "Phenobarbital Versus Clonazepam for Sedative-Hypnotic Taper in Chronic Pain Patients: A Pilot Study". Annals of Clinical Psychiatry 5 (2): 123–8. doi:10.3109/10401239309148974. PMID 8348204.
- ↑ Dr Ray Baker. "Dr Ray Baker's Article on Addiction: Benzodiazepines in Particular". Retrieved 14 February 2009.
- ↑ Oulis, P.; Konstantakopoulos, G. (2010). "Pregabalin in the treatment of alcohol and benzodiazepines dependence.". CNS Neurosci Ther 16 (1): 45–50. doi:10.1111/j.1755-5949.2009.00120.x. PMID 20070788.
- ↑ Oulis, P.; Konstantakopoulos, G. (Jul 2012). "Efficacy and safety of pregabalin in the treatment of alcohol and benzodiazepine dependence.". Expert Opin Investig Drugs 21 (7): 1019–29. doi:10.1517/13543784.2012.685651. PMID 22568872.
- ↑ Zitman, F. G.; Couvée, JE (2001). "Chronic benzodiazepine use in general practice patients with depression: An evaluation of controlled treatment and taper-off: Report on behalf of the Dutch Chronic Benzodiazepine Working Group". The British Journal of Psychiatry 178 (4): 317–24. doi:10.1192/bjp.178.4.317. PMID 11282810.
- ↑ Tönne, U.; Hiltunen, A. J.; Vikander, B.; Engelbrektsson, K.; Bergman, H.; Bergman, I.; Leifman, H.; Borg, S. (1995). "Neuropsychological changes during steady-state drug use, withdrawal and abstinence in primary benzodiazepine-dependent patients". Acta Psychiatrica Scandinavica 91 (5): 299–304. doi:10.1111/j.1600-0447.1995.tb09786.x. PMID 7639085.
- ↑ Kan, CC; Mickers, FC; Barnhoorn, D (2006). "Short- and long-term results of a systematic benzodiazepine discontinuation programme for psychiatric patients". Tijdschrift voor psychiatrie 48 (9): 683–93. PMID 17007474.
- ↑ Jørgensen, VR (2009). "Benzodiazepine reduction does not imply an increased consumption of antidepressants. A survey of two medical practices". Ugeskrift for laeger 171 (41): 2999–3003. PMID 19814928.
- ↑ Lal R, Gupta S, Rao R, Kattimani S (2007). "Emergency management of substance overdose and withdrawal" (PDF). Substance Use Disorder (PDF). World Health Organisation. p. 82. Archived from the original (PDF) on 2010-06-13. Retrieved 2009-06-06.
Generally, a longer-acting benzodiazepine such as chlordiazepoxide or diazepam is used and the initial dose titrated downward
- ↑ Noyes, Russell; Perry, Paul J.; Crowe, Raymond R.; Coryell, William H.; Clancy, John; Yamada, Thoru; Gabel, Janelle (1986). "Seizures Following the Withdrawal of Alprazolam". The Journal of Nervous and Mental Disease 174 (1): 50–2. doi:10.1097/00005053-198601000-00009. PMID 2867122.
- ↑ Noyes Jr, R; Clancy, J; Coryell, WH; Crowe, RR; Chaudhry, DR; Domingo, DV (1985). "A withdrawal syndrome after abrupt discontinuation of alprazolam". The American Journal of Psychiatry 142 (1): 114–6. PMID 2857066.
- ↑ Rickels, Karl; Schweizer, E; Case, WG; Greenblatt, DJ (1990). "Long-term Therapeutic Use of Benzodiazepines: I. Effects of Abrupt Discontinuation". Archives of General Psychiatry 47 (10): 899–907. doi:10.1001/archpsyc.1990.01810220015002. PMID 2222129.
- ↑ Neale, G; Smith, AJ (2007). "Self-harm and suicide associated with benzodiazepine usage". The British journal of general practice 57 (538): 407–8. PMC 2047018. PMID 17504594.
- ↑ Curran, H. V.; Bond, A.; O'Sullivan, G.; Bruce, M.; Marks, I.; Lelliot, P.; Shine, P.; Lader, M. (2009). "Memory functions, alprazolam and exposure therapy: A controlled longitudinal study of agoraphobia with panic disorder". Psychological Medicine 24 (4): 969–76. doi:10.1017/S0033291700029056. PMID 7892364.
- ↑ Busto, Usoa; Fornazzari, Luis; Naranjo, Claudio A. (1988). "Protracted Tinnitus after Discontinuation of Long-Term Therapeutic Use of Benzodiazepines". Journal of Clinical Psychopharmacology 8 (5): 359–362. doi:10.1097/00004714-198810000-00010. PMID 2903182.
- ↑ Higgitt, A.; Fonagy, P.; Toone, B.; Shine, P. (1990). "The prolonged benzodiazepine withdrawal syndrome: Anxiety or hysteria?". Acta Psychiatrica Scandinavica 82 (2): 165–8. doi:10.1111/j.1600-0447.1990.tb01375.x. PMID 1978465.
- ↑ Ashton CH (March 1995). "Protracted Withdrawal From Benzodiazepines: The Post-Withdrawal Syndrome". Psychiatric Annals (benzo.org.uk) 25 (3): 174–179.
- ↑ Barker, M; Greenwood, KM; Jackson, M; Crowe, SF (2004). "Persistence of cognitive effects after withdrawal from long-term benzodiazepine use: A meta-analysis". Archives of Clinical Neuropsychology 19 (3): 437–54. doi:10.1016/S0887-6177(03)00096-9. PMID 15033227.
- ↑ Hood HM, Metten P, Crabbe JC, Buck KJ (February 2006). "Fine mapping of a sedative-hypnotic drug withdrawal locus on mouse chromosome 11". Genes, Brain and Behavior 5 (1): 1–10. doi:10.1111/j.1601-183X.2005.00122.x. PMID 16436183.
- ↑ Vorma, H; Naukkarinen, Hh; Sarna, Sj; Kuoppasalmi, Ki (2005). "Predictors of benzodiazepine discontinuation in subjects manifesting complicated dependence". Substance Use & Misuse 40 (4): 499–510. doi:10.1081/JA-200052433. PMID 15830732.
- ↑ McElhatton, Patricia R. (1994). "The effects of benzodiazepine use during pregnancy and lactation". Reproductive Toxicology 8 (6): 461–75. doi:10.1016/0890-6238(94)90029-9. PMID 7881198.
- 1 2 3 Birchley, Giles (2009). "Opioid and benzodiazepine withdrawal syndromes in the paediatric intensive care unit: A review of recent literature". Nursing in Critical Care 14 (1): 26–37. doi:10.1111/j.1478-5153.2008.00311.x. PMID 19154308.
- ↑ Fontela, Patrícia Scolari; Fontela, Aline; Moraes, Fabrício; Da Silva, Ricardo Bernardi; Sober, Roberta B.; Noer, Francisco; Bruno, Paulo; Einloft, Ana; Garcia, Pedro Celiny Ramos; Piva, Jefferson P. (2003). "Sedation and analgesia in children submitted to mechanical ventilation could be overestimated?". Jornal de Pediatria 79 (4): 343–8. doi:10.2223/JPED.1046. PMID 14513134.
- ↑ Playfor, Stephen; Jenkins, Ian; Boyles, Carolyne; Choonara, Imti; Davies, Gerald; Haywood, Tim; Hinson, Gillian; Mayer, Anton; Morton, Neil; Ralph, Tanya; Wolf, Andrew; United Kingdom Paediatric Intensive Care Society Sedation; Analgesia Neuromuscular Blockade Working Group (2006). "Consensus guidelines on sedation and analgesia in critically ill children". Intensive Care Medicine 32 (8): 1125–36. doi:10.1007/s00134-006-0190-x. PMID 16699772.
- ↑ Ista, Erwin; Van Dijk, Monique; Gamel, Claudia; Tibboel, Dick; De Hoog, Matthijs (2007). "Withdrawal symptoms in children after long-term administration of sedatives and/or analgesics: A literature review. 'Assessment remains troublesome'". Intensive Care Medicine 33 (8): 1396–406. doi:10.1007/s00134-007-0696-x. PMID 17541548.
- 1 2 3 4 5 Baillargeon, L; Landreville, P; Verreault, R; Beauchemin, JP; Grégoire, JP; Morin, CM (2003). "Discontinuation of benzodiazepines among older insomniac adults treated with cognitive-behavioural therapy combined with gradual tapering: A randomized trial". Canadian Medical Association Journal 169 (10): 1015–20. PMC 236226. PMID 14609970.
- ↑ Salzman, Carl (15 May 2004). Clinical geriatric psychopharmacology (4th ed.). USA: Lippincott Williams & Wilkins. pp. 450–3. ISBN 978-0-7817-4380-8.
External links
- Benzodiazepine Withdrawal Symptom Relief
- Benzodiazepines: How they work and how to withdraw by Professor Heather Ashton
- The Minor Tranquilliser Project, For support, Camden, UK
- Benzodiazepine withdrawal syndrome at DMOZ
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||