Lateral medullary syndrome
| Lateral medullary syndrome | |
|---|---|
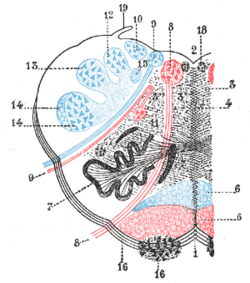 Medulla oblongata, shown by a transverse section passing through the middle of the olive. (Lateral medullary syndrome can affect structures in upper left: #9, #10, #11, #12, #13, and #14.) | |
| Classification and external resources | |
| Specialty | neurology |
| ICD-10 | G46.4 |
| DiseasesDB | 10449 |
| eMedicine | emerg/834 |
| MeSH | D014854 |
Lateral medullary syndrome (also called Wallenberg syndrome and posterior inferior cerebellar artery syndrome) is a disorder in which the patient has a constellation of neurologic symptoms due to injury to the lateral part of the medulla in the brain, resulting in tissue ischemia and necrosis.
Signs and symptoms
This syndrome is characterized by sensory deficits affecting the trunk (torso) and extremities on the opposite side of the infarction and sensory deficits affecting the face and cranial nerves on the same side with the infarct. Specifically, there is a loss of pain and temperature sensation on the contralateral (opposite) side of the body and ipsilateral (same) side of the face. This crossed finding is diagnostic for the syndrome.
Clinical symptoms include swallowing difficulty, or dysphagia,[1] slurred speech, ataxia, facial pain, vertigo, nystagmus, Horner's syndrome, diplopia, and possibly palatal myoclonus.
Affected persons have difficulty in swallowing (dysphagia) resulting from involvement of the nucleus ambiguus, as well as slurred speech (dysarthria) and disordered vocal quality (dysphonia) . Damage to the spinal trigeminal nucleus causes absence of pain on the ipsilateral side of the face, as well as an absent corneal reflex.
The spinothalamic tract is damaged, resulting in loss of pain and temperature sensation on the opposite side of the body. The damage to the cerebellum or the inferior cerebellar peduncle can cause ataxia. Damage to the hypothalamospinal fibers disrupts sympathetic nervous system relay and gives symptoms analogous to Horner syndrome.
Nystagmus and vertigo may result in falling, caused from involvement of the region of Deiters' nucleus and other vestibular nuclei. Onset is usually acute with severe vertigo.
Palatal myoclonus may be observed due to disruption of the central tegmental tract.

Features
| Dysfunction | Effects |
| vestibular nuclei | vestibular system: vomiting, vertigo, nystagmus, |
| inferior cerebellar peduncle | Ipsilateral cerebellar signs including ataxia, dysmetria (past pointing), dysdiadokokinesia |
| central tegmental tract | palatal myoclonus |
| lateral spinothalamic tract | contralateral deficits in pain and temperature sensation from body (limbs and torso) |
| spinal trigeminal nucleus & tract | ipsilateral loss of pain, and temperature sensation from face |
| nucleus ambiguus - (which affects vagus nerve and glossopharyngeal nerve) - localizing lesion (all other deficits are present in lateral pontine syndrome as well) | ipsilateral laryngeal, pharyngeal, and palatal hemiparalysis: dysphagia, hoarseness, diminished gag reflex (efferent limb - CN.X) |
| descending sympathetic fibers | ipsilateral Horner's syndrome (ptosis, miosis, & anhydrosis) |
Cause

It is the clinical manifestation resulting from occlusion of the posterior inferior cerebellar artery (PICA) or one of its branches or of the vertebral artery, in which the lateral part of the medulla oblongata infarcts, resulting in a typical pattern. The most commonly affected artery is the vertebral artery, followed by the PICA, superior middle and inferior medullary arteries.
Treatment
Treatment for lateral medullary syndrome involves focusing on relief of symptoms and active rehabilitation to help those suffering from the stroke syndrome recover their activities of daily living and cope with neurologic loss that can be psychologically devastating. Depressed mood and withdrawal from society can be seen in patients following the initial neurologic insult.
A feeding tube inserted through the mouth or gastrostomy may be necessary if swallowing is impaired. Speech therapy may be beneficial in diet recommendations and helping to understand if there is risk for aspiration pneumonia. In some cases, medication may be used to reduce or eliminate pain. Some studies have reported success in mitigating the chronic neuropathic pain associated with the syndrome with anti-epileptics such as gabapentin. The small caliber of the affected PICA does not typically lend itself to reliable surgical recanalization, although a cerebral angiogram is typically required by a neuroradiologist to make this distinction.[2]
One of the most unique and difficult to treat symptoms that occur due to Wallenberg syndrome are interminable, violent hiccups. The hiccups can be so severe that patients often struggle to eat, sleep and carry on conversations. Depending on the severity of the blockage caused by the stroke, the hiccups can last for weeks. Unfortunately there are very few successful medications available to mediate the inconvenience of constant hiccups.
Long term treatment generally involves the use of antiplatelets like aspirin or clopidogrel and statin regimen for the rest of their lives in order to minimize the risk of another stroke. Warfarin is used if atrial fibrillation is present. Other medications may be necessary in order to suppress high blood pressure and risk factors associated with strokes.
Treatment for this disorder can be disconcerting because some individuals will always have residual symptoms due to the severity of the blockage. Two patients may present with the same initial symptoms right after the stroke has occurred, but after several months one patient may fully recover while the other is still severely handicapped. [3]
Prognosis
The outlook for someone with lateral medullary syndrome depends upon the size and location of the area of the brain stem damaged by the stroke. Some individuals may see a decrease in their symptoms within weeks or months. Others may be left with significant neurological disabilities for years after the initial symptoms appeared.[2]
History
This syndrome was first described in 1808 by Gaspard Vieusseux.[4] First descriptions by Adolf Wallenberg were in 1895 (clinical) and 1901 (autopsy findings).
See also
- Alternating hemiplegia of childhood
- Benedikt syndrome
- Stroke Recovery
- Lateral pontine syndrome
- Medial medullary syndrome
- Weber's syndrome
References
- ↑ Khedr E, Abo-Elfetoh N (October 2009). "Therapeutic role of rTMS on recovery of dysphagia in patients with lateral medullary syndrome and brain stem infarction". J. Neurol. Neurosurg. Psychiatr. 81 (5): 495–499. doi:10.1136/jnnp.2009.188482. PMID 19828479.
- 1 2 wallenbergs at NINDS
- ↑ http://www.healthline.com/galecontent/wallenberg-syndrome
- ↑ synd/1778 at Who Named It?
External links
- -831848439 at GPnotebook
- Department of Biomedical Engineering at Johns Hopkins University
- MRI of Lateral Medullary Infarction (Wallenberg) MedPix Images
| ||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||