Von Willebrand disease
| von Willebrand disease | |
|---|---|
| Classification and external resources | |
| Specialty | Hematology |
| ICD-10 | D68.0 |
| ICD-9-CM | 286.4 |
| OMIM | 193400 |
| DiseasesDB | 14007 |
| MedlinePlus | 000544 |
| eMedicine | ped/2419 |
| MeSH | D014842 |
| GeneReviews | |
Von Willebrand disease (vWD) (/ˌfʌnˈvɪlᵻbrɑːnt/) is the most common hereditary coagulation abnormality described in humans, although it can also be acquired as a result of other medical conditions. It arises from a qualitative or quantitative deficiency of von Willebrand factor (vWF), a multimeric protein that is required for platelet adhesion. It is known to affect humans and dogs (notably Doberman Pinschers), and rarely swine, cattle, horses, and cats. There are three forms of vWD: hereditary, acquired, and pseudo or platelet type. There are three types of hereditary vWD: vWD type 1, vWD type 2, and vWD type 3. Within the three inherited types of vWD there are various subtypes. Platelet type vWD is also an inherited condition.
vWD type 1 is the most common type of the disorder and those that have it are typically asymptomatic or may experience mild symptoms such as nosebleeds although there may be severe symptoms in some cases. There are various factors that affect the presentation and severity of symptoms of vWD such as blood type.
vWD is named after Erik Adolf von Willebrand, a Finnish physician who first described the disease in 1926.[1]
Signs and symptoms
The various types of vWD present with varying degrees of bleeding tendency, usually in the form of easy bruising, nosebleeds and bleeding gums. Women may experience heavy menstrual periods and blood loss during childbirth.
Severe internal or joint bleeding is uncommon (except for in vWD type 3).
Genetics

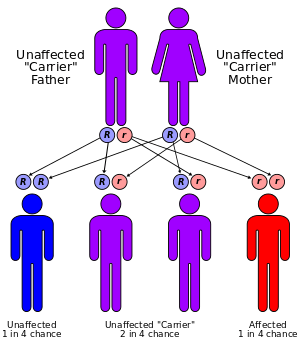
The vWF gene is located on chromosome 12 (12p13.2). It has 52 exons spanning 178kbp. Types 1 and 2 are inherited as autosomal dominant traits and type 3 is inherited as autosomal recessive. Occasionally type 2 also inherits recessively.
Pathophysiology
vWF is mainly active in conditions of high blood flow and shear stress. Deficiency of vWF therefore shows primarily in organs with extensive small vessels, such as the skin, the gastrointestinal tract and the uterus. In angiodysplasia, a form of telangiectasia of the colon, shear stress is much higher than in average capillaries, and the risk of bleeding is increased concomitantly.
In more severe cases of type 1 vWD, genetic changes are common within the vWF gene and are highly penetrant. In milder cases of type 1 vWD there may be a complex spectrum of molecular pathology in addition to polymorphisms of the vWF gene alone.[2] The individual's ABO blood group can influence presentation and pathology of vWD. Those individuals with blood group O have a lower mean level than individuals with other blood groups. Unless ABO group–specific vWF:antigen reference ranges are used, normal group O individuals can be diagnosed as type I vWD, and some individuals of blood group AB with a genetic defect of vWF may have the diagnosis overlooked because vWF levels are elevated due to blood group.[3]
Diagnosis
When vWD is suspected, blood plasma of a patient must be investigated for quantitative and qualitative deficiencies of vWF. This is achieved by measuring the amount of vWF in a vWF antigen assay and the functionality of vWF with a glycoprotein (GP)Ib binding assay, a collagen binding assay, or a ristocetin cofactor activity (RiCof) or ristocetin induced platelet agglutination (RIPA) assays. Factor VIII levels are also performed because factor VIII is bound to vWF which protects the factor VIII from rapid breakdown within the blood. Deficiency of vWF can therefore lead to a reduction in factor VIII levels, which explains the elevation in PTT time. Normal levels do not exclude all forms of vWD, particularly type 2 which may only be revealed by investigating platelet interaction with subendothelium under flow (PAF), a highly specialized coagulation study not routinely performed in most medical laboratories. A platelet aggregation assay will show an abnormal response to ristocetin with normal responses to the other agonists used. A platelet function assay (PFA) may give an abnormal collagen/adrenaline closure time and in most cases (but not all) a normal collagen/ADP time. Type 2N may be considered if factor VIII levels are disproportionately low, but confirmation requires a "factor VIII binding" assay. Detection of vWD is complicated by vWF being an acute phase reactant with levels rising in infection, pregnancy and stress.
Other tests performed in any patient with bleeding problems are a complete blood count (especially platelet counts), APTT (activated partial thromboplastin time), prothrombin time, thrombin time and fibrinogen level. Testing for factor IX may also be performed if hemophilia B is suspected. Other coagulation factor assays may be performed depending on the results of a coagulation screen. Patients with von Willebrand disease will typically display a normal prothrombin time and a variable prolongation of partial thromboplastin time.
| Condition | Prothrombin time | Partial thromboplastin time | Bleeding time | Platelet count |
|---|---|---|---|---|
| Vitamin K deficiency or warfarin | Prolonged | Normal or mildly prolonged | Unaffected | Unaffected |
| Disseminated intravascular coagulation | Prolonged | Prolonged | Prolonged | Decreased |
| Von Willebrand disease | Unaffected | Prolonged or unaffected | Prolonged | Unaffected |
| Haemophilia | Unaffected | Prolonged | Unaffected | Unaffected |
| Aspirin | Unaffected | Unaffected | Prolonged | Unaffected |
| Thrombocytopenia | Unaffected | Unaffected | Prolonged | Decreased |
| Liver failure, early | Prolonged | Unaffected | Unaffected | Unaffected |
| Liver failure, end-stage | Prolonged | Prolonged | Prolonged | Decreased |
| Uremia | Unaffected | Unaffected | Prolonged | Unaffected |
| Congenital afibrinogenemia | Prolonged | Prolonged | Prolonged | Unaffected |
| Factor V deficiency | Prolonged | Prolonged | Unaffected | Unaffected |
| Factor X deficiency as seen in amyloid purpura | Prolonged | Prolonged | Unaffected | Unaffected |
| Glanzmann's thrombasthenia | Unaffected | Unaffected | Prolonged | Unaffected |
| Bernard-Soulier syndrome | Unaffected | Unaffected | Prolonged | Decreased or unaffected |
| Factor XII deficiency | Unaffected | Prolonged | Unaffected | Unaffected |
| C1INH deficiency | Unaffected | Shortened | Unaffected | Unaffected |
The testing for vWD can be influenced by laboratory procedures. There are numerous variables in the testing procedure that may affect the validity of the test results and may result in a missed or erroneous diagnosis. The chance of procedural errors are typically greatest during the preanalytical phase (during collecting storage and transportation of the specimen) especially when the testing is contracted out to an outside facility and the specimen is frozen and transported long distances.[4] Diagnostic errors are not uncommon, and there is a varying rate of testing proficiency amongst laboratories with error rates ranging from 7% to 22% in some studies to as high as 60% in cases of misclassification of vWD sub-type. To increase the probability of a proper diagnosis testing should be done at a facility with immediate on-site processing in their own specialized coagulation laboratory.[5][6]
Types
The four hereditary types of vWD described are type 1, type 2, type 3, and pseudo or platelet-type. Most cases are hereditary, but acquired forms of vWD have been described. The International Society on Thrombosis and Haemostasis's (ISTH) classification depends on the definition of qualitative and quantitative defects.[7]
Type 1
Type 1 vWD (60-80% of all vWD cases) is a quantitative defect which is heterozygous for the defective gene. It can arise from failure to secrete vWF into the circulation or from vWF being cleared more quickly than normal. Decreased levels of vWF are detected at 10-45% of normal, i.e. 10-45 IU.
Many patients are asymptomatic or may have mild symptoms and not have clearly impaired clotting which might suggest a bleeding disorder. Often the discovery of vWD occurs incidentally to other medical procedures requiring a blood work-up. Most cases of type 1 vWD are never diagnosed due to the asymptomatic or mild presentation of type I and most people usually end up leading a normal life free of complications with many being unaware that they have the disorder.
Trouble may however arise in some patients in the form of bleeding following surgery (including dental procedures), noticeable easy bruising, or menorrhagia (heavy menstrual periods). There are also a minority of cases of Type 1 which may present with severe hemorrhagic symptoms.
Type 2
Type 2 vWD (20-30% of cases) is a qualitative defect and the bleeding tendency can vary between individuals. Four subtypes exist: 2A, 2B, 2M and 2N.
Type 2A
The vWF is quantitatively normal but qualitatively defective. The ability of the defective von Willebrand factors to coalesce and form large vWF multimers is impaired, resulting in decreased quantity of large vWF multimers and low ristocetin co-factor (RCoF) activity. Only small multimer units are detected in the circulation. Von Willebrand factor antigen (vWF:Ag) assay is low or normal.
Type 2B
This is a "gain of function" defect. The ability of the qualitatively defective von Willebrand factor to bind to glycoprotein Ib (GPIb) receptor on the platelet membrane is abnormally enhanced, leading to its spontaneous binding to platelets and subsequent rapid clearance of the bound platelets and of the large vWF multimers. Thrombocytopenia may occur. Large vWF multimers are reduced or absent from the circulation.
The ristocetin cofactor activity is low when the patient's platelet-poor plasma is assayed against formalin-fixed, normal donor platelets. However, when the assay is performed with the patient's own platelets (platelet-rich plasma), a lower-than-normal amount of ristocetin causes aggregation to occur. This is due to the large vWF multimers remaining bound to the patient's platelets. Patients with this sub-type are unable to use desmopressin as a treatment for bleeding, because it can lead to unwanted platelet aggregation and aggravation of thrombocytopenia.
Type 2M
Type 2M von Willebrand disease is a qualitative defect of von Willebrand factor characterized by its decreased ability to bind to glycoprotein Ib (GPIb) receptor on the platelet membrane and normal capability at multimerization. The vWF antigen levels are normal. The ristocetin cofactor activity is decreased and high molecular weight large vWF multimers are present in the circulation.[8]
Type 2N (Normandy)
This is a deficiency of the binding of vWF to coagulation factor VIII. The vWF antigen test is normal indicating normal quantity of vWF. The ristocetin cofactor assay is normal. Assay for coagulation factor VIII revealed marked quantitative decrease equivalent to levels seen in hemophilia A. This has led to some vWD type 2N patients being misdiagnosed as having hemophilia A.
Type 3
Type 3 is the most severe form of von Willebrand disease (homozygous for the defective gene) and is characterized by complete absence of production of vWF. The von Willebrand factor is undetectable in the vWF antigen assay. Since the von Willebrand factor protects coagulation Factor VIII from proteolytic degradation, total absence of vWF leads to extremely low Factor VIII level, equivalent to that seen in severe hemophilia A with its clinical manifestations of life-threatening external and internal hemorrhages. The inheritance pattern of vWD type 3 is autosomal recessive while the inheritance pattern of hemophilia A is x-linked recessive.
Platelet-type
Platelet-type vWD (also known as pseudo-vWD) is an autosomal dominant genetic defect of the platelets. The von Willebrand factor is qualitatively normal and genetic testing of the von Willebrand gene and vWF protein reveals no mutational alteration. The defect lies in the qualitatively altered glycoprotein Ib (GPIb) receptor on the platelet membrane which increases its affinity to bind to the von Willebrand factor. Large platelet aggregates and high molecular weight vWF multimers are removed from the circulation resulting in thrombocytopenia and diminished or absent large vWF multimers. The ristocetin cofactor activity and loss of large vWF multimers are similar to vWD type 2B.
Acquired
Acquired vWD can occur in patients with autoantibodies. In this case the function of vWF is not inhibited but the vWF-antibody complex is rapidly cleared from the circulation.
A form of vWD occurs in patients with aortic valve stenosis, leading to gastrointestinal bleeding (Heyde's syndrome). This form of acquired vWD may be more prevalent than is presently thought. In 2003 Vincentelli et al. noted that patients with acquired vWD and aortic stenosis who underwent valve replacement experienced a correction of their hemostatic abnormalities but that the hemostatic abnormalities can recur after 6 months when the prosthetic valve is a poor match with the patient.[9] Similarly, acquired vWD contributes to the bleeding tendency in people with an implant of a Left Ventricular Assist Device (LVAD), a pump that pumps blood from the left ventricle of the heart into the aorta.[10] Large multimers of vWF are destroyed by mechanical stress in both conditions.
Thrombocythemia is another cause of acquired von Willebrand disease, due to sequestration of von Willebrand factor via the adhesion of vast numbers of platelets.
Acquired vWD has also been described in the following disorders: Wilms' tumour, hypothyroidism and mesenchymal dysplasias.
Treatment
For patients with vWD type 1 and vWD type 2A, desmopressin (DDAVP) is recommended for use in cases of minor trauma, or in preparation for dental or minor surgical procedures. DDAVP stimulates the release of von Willebrand factor (vWF) from the Weibel Palade bodies of endothelial cells, thereby increasing the levels of vWF (as well as coagulant factor VIII) 3 to 5-fold. DDAVP is available as a preparation for intranasal administration (Stimate) and as a preparation for intravenous administration.
DDAVP is contraindicated in vWD type 2b because of the risk of aggravated thrombocytopenia and thrombotic complications.
DDAVP is probably not effective in vWD type 2M and is rarely effective in vWD type 2N. It is totally ineffective in vWD type 3.
For women with heavy menstrual bleeding, estrogen-containing oral contraceptive medications are effective in reducing the frequency and duration of the menstrual periods. Estrogen compounds available for use in the correction of menorrhagia are Ethinyl Estradiol and Levonorgestel (levona, Nordette, Lutera, Trivora). Administration of Ethinyl Estradiol diminishes the secretion of luteinizing hormone and follicle stimulating hormone from the pituitary, leading to stabilization of the endometrial surface of the uterus.
Desmopressin (DDAVP) is a synthetic analog of the natural antidiuretic hormone vasopressin. Overuse of Desmopressin (DDAVP) can lead to water retention and dilutional hyponatremia with consequent convulsion.
For patients with vWD scheduled for surgery and cases of vWD disease complicated by clinically significant hemorrhage, human derived medium purity Factor VIII concentrates, which also contain von Willebrand factors, are available for prophylaxis and treatment. Humate P, Alphanate and Koate HP are commercially available for prophylaxis and treatment of von Willebrand disease. Monoclonally purified Factor VIII concentrates and recombinant Factor VIII concentrates contain insignificant quantity of VWF and are therefore not clinically useful.
Development of alloantibodies occur in 10-15% of patients receiving human derived medium purity Factor VIII concentrates and the risk of allergic reactions including anaphylaxis must be considered when administering these preparations. Administration of the latters is also associated with increased risk of venous thromboembolic complications.
Blood transfusions are given as needed to correct anemia and hypotension secondary to hypovolemia.
Infusion of platelet concentrates is recommended for correction of hemorrhage associated with platelet-type von Willebrand disease.
The antifibrinolytic agents Epsilon amino caproic acid and Tranexamic acid are useful adjuncts in the management of vWD complicated by clinical hemorrhage.
The use Topical thrombin JMI and Topical Tisseel VH are effective adjuncts for correction of hemorrhage from wounds.
Epidemiology
The prevalence of vWD is about 1 in 100 individuals.[11] However the majority of these people do not have symptoms. The prevalence of clinically significant cases is 1 per 10,000.[11] Because most forms are rather mild, they are detected more often in women, whose bleeding tendency shows during menstruation. It may be more severe or apparent in people with blood type O.
History
In 1924, a 5-year-old girl who lived on the Åland Islands was brought to Deaconess Hospital in Helsinki, Finland, where she was seen by Dr. Erik von Willebrand. He ultimately assessed 66 members of her family and reported in 1926 that this was a previously undescribed bleeding disorder that differed from hemophilia. Dr von Willebrand recognized the autosomal inheritance pattern, and noted that the bleeding symptoms were greater in children and in women of childbearing age. Thus, he stated that patients with this syndrome had (1) mucocutaneous bleeding, (2) normal clotting time, (3) autosomal inheritance rather than being linked to the X chromosome, and (4) prolonged bleeding times by the Duke method (ear lobe bleeding time). He subsequently found that blood transfusions were useful not only to correct the anemia but also to control bleeding.[12]
In the 1950s, it became clear that a "plasma factor," antihemophilic factor (FVIII), was decreased in these persons and that Cohn fraction I-0 could correct both the plasma deficiency of FVIII and the prolonged bleeding time. Since this time, the factor causing the long bleeding time was called "von Willebrand factor" in honor of Dr. Erick von Willebrand.
Variant forms of vWF were recognized in the 1970s, and we now recognize that these variations are the result of synthesis of an abnormal protein.
During the 1980s, molecular and cellular studies distinguished hemophilia A and vWD more precisely. Persons who had vWD had a normal FVIII gene on the X chromosome, and some had an abnormal vWF gene on chromosome 12. Gene sequencing identified many of these persons as having a vWF gene mutation. The genetic causes of milder forms of low vWF are still under investigation, and these forms may not always be caused by an abnormal vWF gene.
See also
- Bernard-Soulier syndrome, caused by a deficiency in the vWF receptor, GPIb
- Blood diseases
- Purpura secondary to clotting disorders
References
- ↑ doctor/2690 at Who Named It?
- ↑ James P, Notley C, Hegadorn C, Leggo J, Tuttle A, Tinlin S, Brown C, Andrews C, Labelle A, Chirinian Y, O'Brien L, Othman M, Rivard G, Rapson D, Hough C, Lillicrap D (2007). "The mutational spectrum of type 1 von Willebrand disease: Results from a Canadian cohort study". Blood 109 (1): 145–54. doi:10.1182/blood-2006-05-021105. PMID 17190853.
- ↑ Gill, JC; Endres-Brooks J; Bauer PJ; Marks WJ; Montgomery RR (1987). "The effect of ABO blood group on the diagnosis of von Willebrand disease". Blood 69 (6): 1691–5. PMID 3495304.
- ↑ Christine A. Lee, Rezan A. Kadir, Peter A. Kouides: Inherited Bleeding Disorders in Women P.,ISBN 1-4051-6915-X
- ↑ Favaloro EJ, Bonar R, Kershaw G, et al. (July 2006). "Reducing errors in identification of von Willebrand disease: the experience of the Royal College of Pathologists of Australasia quality assurance program". Semin. Thromb. Hemost. 32 (5): 505–13. doi:10.1055/s-2006-947865. PMID 16862524.
- ↑ Chandler WL, Peerschke EI, Castellone DD, Meijer P (June 2011). "Von Willebrand factor assay proficiency testing. The North American Specialized Coagulation Laboratory Association experience". Am. J. Clin. Pathol. 135 (6): 862–9. doi:10.1309/AJCPH5JK4ONENPAE. PMID 21571959.
- ↑ Sadler JE (1994). "A revised classification of von Willebrand disease. For the Subcommittee on von Willebrand Factor of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis". Thromb. Haemost. 71 (4): 520–5. PMID 8052974.
- ↑ Oxford Handbook of Clinical Haematology, Chapter 11
- ↑ Vincentelli A, Susen S, Le Tourneau T, et al. (July 2003). "Acquired von Willebrand syndrome in aortic stenosis". N. Engl. J. Med. 349 (4): 343–9. doi:10.1056/NEJMoa022831. PMID 12878741.
- ↑ Uriel, N; Pak SW; Jorde UP; Jude B; Susen S; Vincentelli A; Ennezat PV; Cappleman S; Naka Y; Mancini D (5 Oct 2010). "Acquired von Willebrand syndrome after continuous-flow mechanical device support contributes to a high prevalence of bleeding during long-term support and at the time of transplantation". J Am Coll Cardiol. 56(15) (15): 1207–13. doi:10.1016/j.jacc.2010.05.016. PMID 20598466.
- 1 2 "Molecular basis of von Willebrand disease and its clinical implications". Haematologica 89 (9): 1036. 1 September 2004. PMID 15377463.
- ↑ Von Willebrand, EA (May 1999). "Hereditary pseudohaemophilia". Haemophilia : the official journal of the World Federation of Hemophilia 5 (3): 223–31; discussion 222. doi:10.1046/j.1365-2516.1999.00302.x. PMID 10444294.
- Notes
- Harrison's textbook of Internal Medicine, Chapter 177.
- Sadler JE (1998). "Biochemistry and genetics of von Willebrand factor". Annu. Rev. Biochem. 67: 395–424. doi:10.1146/annurev.biochem.67.1.395. PMID 9759493.
- Mannucci PM; Mannucci, Pier Mannuccio (2004). "Treatment of von Willebrand's Disease". N. Engl. J. Med. 351 (7): 683–94. doi:10.1056/NEJMra040403. PMID 15306670.
- Laffan M, Brown SA, Collins PW, et al. (2004). "The diagnosis of von Willebrand disease: a guideline from the UK Haemophilia Centre Doctors' Organization". Haemophilia 10 (3): 199–217. doi:10.1111/j.1365-2516.2004.00894.x. PMID 15086318.
- Williams Hematology, 7th edition, Grune and Stratton, chapters112 (p. 1806) and118 (p. 1937)
External links
- GeneReviews/NCBI/NIH/UW entry on von Willebrand Disease
- Sheffield.ac.uk, International repository on vWF mutations (University of Sheffield)
- Hemophilia.org
- Haemophilia.org.uk
- WFH.org, World Federation of Hemophilia
- Ukhcdo.org UK Haemophilia Centre Directors Organisation
- NIH.gov, Clinical Practice Guidelines by the U.S. National Heart, Lung, and Blood Institute