Transdermal patch

A transdermal patch is a medicated adhesive patch that is placed on the skin to deliver a specific dose of medication through the skin and into the bloodstream. Often, this promotes healing to an injured area of the body. An advantage of a transdermal drug delivery route over other types of medication delivery such as oral, topical, intravenous, intramuscular, etc. is that the patch provides a controlled release of the medication into the patient, usually through either a porous membrane covering a reservoir of medication or through body heat melting thin layers of medication embedded in the adhesive. The main disadvantage to transdermal delivery systems stems from the fact that the skin is a very effective barrier; as a result, only medications whose molecules are small enough to penetrate the skin can be delivered by this method. A wide variety of pharmaceuticals are now available in transdermal patch form.
The first commercially available prescription patch was approved by the U.S. Food and Drug Administration in December 1979. These patches administered scopolamine for motion sickness.[1][2]
Development
Before these patches go into the market, they have to be carefully studied. One way to study these patches is through the use of Franz Diffusion Cell systems. This system is used to study the effects of temperature on the permeated amount of a specific drug on a certain type of membrane, which in this case would be the membrane that is used in the patches. A Franz Diffusion Cell system is composed of a receptor and a donor cell. In many of these research studies the following procedure is used. The donor cell is set at a specific temperature (the temperature of the environment ), while the receptor cell is set at different one (temperature of the body).
Different runs are performed using different temperatures to study the impact of temperature on the release of a certain medicament through a certain type of membrane. Although different concentrations of the medicament are used in this study, they do not affect the amount permeated through the membrane (the process is constant). From Chemical kinetics it is concluded that these studies are zero order, since the concentration plays no role in the permeated amount through the membrane.
Some pharmaceuticals must be combined with substances, such as alcohol, within the patch to increase their ability to penetrate the skin in order to be used in a trans dermal patch. Others can overwhelm the body if applied in only one place, and are often cut into sections and applied to different parts of the body to avoid this, such as nitroglycerin. Many molecules, however, such as insulin, are too large to pass through the skin without it being modified in some way. Several new technologies are being investigated to allow larger molecules to be delivered transdermally.[3]
Popular uses
- The highest selling transdermal patch in the United States is the nicotine patch, which releases nicotine in controlled doses to help with cessation of tobacco smoking. The first commercially available vapour patch to reduce smoking was approved in Europe in 2007.
- Two opioid medications used to provide round-the-clock relief for severe pain are often prescribed in patch form, fentanyl CII (marketed as Duragesic) and buprenorphine CIII (marketed as BuTrans).
- Hormonal patches
- estrogen patches are sometimes prescribed to treat menopausal symptoms (as well as post-menopausal osteoporosis) and to transgender women as a type of hormone replacement therapy.
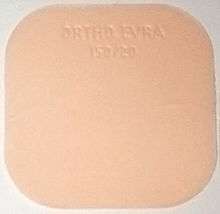
- contraceptive patch (marketed as Ortho Evra or Evra) and
- testosterone CIII patches for both men (Androde) and women (Intrinsa).
- Nitroglycerin patches are sometimes prescribed for the treatment of angina in lieu of sublingual pills.
- Transdermal scopolamine is commonly used as a treatment for motion sickness.[4]
- The anti-hypertensive drug clonidine is available in transdermal patch form[5] under the brand name Catapres-TTS.[6]
- Emsam, a transdermal form of the MAOI selegiline, became the first transdermal delivery agent for an antidepressant approved for use in the U.S. in March 2006.[7]
- Daytrana, the first methylphenidate transdermal delivery system for the treatment of Attention Deficit Hyperactivity Disorder (ADHD), was approved by the FDA in April 2006.[8]
- Vitamin B12 may also be administered through a transdermal patch. Cyanocobalamin, a highly stable form of vitamin B12, is compatible with transdermal patching.
- 5-Hydroxytryptophan (5-HTP) can also be administered through a transdermal patch, which was launched in the United Kingdom in early 2014.[9]
- Rivastigmine, an Alzheimer's treatment medication, was released in patch form in 2007, under the brand name Exelon[10]
- Health Supplements such as Thrive by Le-Vel make use of a DFT or derma fusion technology patch. Slow releases natural ingredients such as Garcinia Cambogia, White Will bark, CoQ10, Green Coffee Bean Extract and Saffron. The newer Black Label version contains some natural Mood enhancers 5-HTP, L-Theanine, and Yerba Mate.
Adverse events
- In 2005, the FDA announced that they were investigating reports of death and other serious adverse events related to narcotic overdose in patients using Duragesic, the fentanyl transdermal patch for pain control. The Duragesic product label was subsequently updated to add safety information in June 2005.[11]
- In 2007, Shire and Noven Pharmaceuticals, manufacturers of the Daytrana ADHD patch, announced a voluntary recall of several lots of the patch due to problems with separating the patch from its protective release liner.[12] Since then, no further problems with either the patch or its protective packaging have been reported.
- In 2008, two manufacturers of the Fentanyl patch, ALZA Pharmaceuticals (a division of major medical manufacturer Johnson & Johnson) and Sandoz, subsequently issued a recall of their versions of the patch due to a manufacturing defect that allowed the gel containing the medication to leak out of its pouch too quickly, which could result in overdose and death.[13] As of March 2009, Sandoz—now manufactured by ALZA—no longer uses gel in its transdermal fentanyl patch; instead, Sandoz-branded fentanyl patches use a matrix/adhesive suspension (where the medication is blended with the adhesive instead of held in a separate pouch with a porous membrane), similar to other fentanyl patch manufacturers such as Mylan and Janssen.[14]
- In 2009, the FDA announced a public health advisory warning of the risk of burns during MRI scans from transdermal drug patches with metallic backings. Patients should be advised to remove any medicated patch prior to an MRI scan and replace it with a new patch after the scan is complete.[15]
- In 2009, an article in Europace journal detailed stories of skin burns that occurred with transdermal patches that contain metal (usually as a backing material) caused by shock therapy from external as well as internal cardioverter defibrillators (ICD).[16]
Components
The main components to a transdermal patch are:
- Liner - Protects the patch during storage. The liner is removed prior to use.
- Drug - Drug solution in direct contact with release liner
- Adhesive - Serves to adhere the components of the patch together along with adhering the patch to the skin
- Membrane - Controls the release of the drug from the reservoir and multi-layer patches
- Backing - Protects the patch from the outer environment
- Permeation Enhancer - These are permeation promoter for drugs, which increases delivery of drug.
- Matrix Filler - It provides bulk to matrix as well as some of fillers acts as matrix stiffening agent.
Other components includes: Stabilizer (anti oxidants), Preservatives etc.
Types

There are five main types of transdermal patches.
Single-layer Drug-in-Adhesive
The adhesive layer of this system also contains the drug. In this type of patch the adhesive layer not only serves to adhere the various layers together, along with the entire system to the skin, but is also responsible for the releasing of the drug. The adhesive layer is surrounded by a temporary liner and a backing.
Multi-layer Drug-in-Adhesive
The multi-layer drug-in-adhesive patch is similar to the single-layer system; the multi-layer system is different, however, in that it adds another layer of drug-in-adhesive, usually separated by a membrane (but not in all cases). One of the layers is for immediate release of the drug and other layer is for control release of drug from the reservoir. This patch also has a temporary liner-layer and a permanent backing. The drug release from this depends on membrane permeability and diffusion of drug molecules.
Reservoir
Unlike the single-layer and multi-layer drug-in-adhesive systems, the reservoir transdermal system has a separate drug layer. The drug layer is a liquid compartment containing a drug solution or suspension separated by the adhesive layer. The drug reservoir is totally encapsulated in a shallow compartment molded from a drug-impermeable metallic plastic laminate, with a rate-controlling membrane made of a polymer like vinyl acetate on one surface. This patch is also backed by the backing layer. In this type of system the rate of release is zero order.
Matrix
The matrix system has a drug layer of a semisolid matrix containing a drug solution or suspension. The adhesive layer in this patch surrounds the drug layer, partially overlaying it. Also known as a monolithic device.
Vapour Patch
In a vapour patch, the adhesive layer not only serves to adhere the various layers together but also to release vapour. Vapour patches release essential oils for up to 6 hours and are mainly used for decongestion. Other vapour patches on the market improve quality of sleep or aid in smoking cessation.
Regulatory aspects
A transdermal patch is classified by the U.S. Food and Drug Administration as a combination product, consisting of a medical device combined with a drug or biological product that the device is designed to deliver. Prior to sale in the United States, any transdermal patch product must apply for and receive approval from the Food and Drug Administration, demonstrating safety and efficacy for its intended use.[17]
References
- ↑ Segal, Marian. "Patches, Pumps and Timed Release: New Ways to Deliver Drugs". Food and Drug Administration. Archived from the original on 2007-02-10. Retrieved 2007-02-24.
- ↑ "FDA approves scopolamine patch to prevent peri-operative nausea". Food and Drug Administration. 1997-11-10. Archived from the original on 2006-12-19. Retrieved 2007-02-12.
- ↑ Prausnitz M, Langer R. Trans dermal drug delivery. Nature Biotechnology. Volume 26, Number 11, Pages 1261-1268, November 2008
- ↑ Nachum Z, Shupak A, Gordon CR (2006). "Transdermal scopolamine for prevention of motion sickness : clinical pharmacokinetics and therapeutic applications". Clinical Pharmacokinetics 45 (6): 543–66. doi:10.2165/00003088-200645060-00001. PMID 16719539.
- ↑ Berner B, John VA (February 1994). "Pharmacokinetic characterisation of transdermal delivery systems". Clinical pharmacokinetics 26 (2): 121–34. doi:10.2165/00003088-199426020-00005. PMID 8162656.
- ↑ First Databank Inc. "Clonidine - Transdermal (Catapres-TTS) side effects, medical uses, and drug interactions". Retrieved 2010-09-28.
- ↑ Peck, Peggy (2006-03-01). "FDA Approves First Antidepressant Transdermal Patch". Retrieved 2010-09-28.
- ↑ Cabray, Matthew (2006-04-12). "Transdermal Patch Approved For Treatment Of ADHD". Retrieved 2010-09-28.
- ↑ "'Revolutionary' 24-hour slow release 5-HTP transdermal patch, launched in early 2014 in the United Kingdom". 5htppatch.co.uk. Retrieved 2014-06-18.
- ↑
- PatchBrothers, lifestyle, party patches, body boosts and transdermal pick me ups
- ↑ "FDA ALERT (07/2005): Narcotic Overdose and Death". Food and Drug Administration. 2005-07-15. Archived from the original on 2007-02-20. Retrieved 2007-02-24.
- ↑ Megget, Katrina (2007-09-05). "ADHD Transdermal Patches Withdrawn". Retrieved 2010-09-28.
- ↑ Silverman, Ed (2008-02-12). "J&J and Sandoz Recall Fentanyl Patches". Retrieved 2010-09-28.
- ↑ As stated on the packaging and labels of Sandoz-branded Fentanyl Transdermal System products, revised March 2009.
- ↑ "FDA Public Health Advisory: Risk of Burns during MRI Scans from Transdermal Drug Patches with Metallic Backings". Archived from the original on March 7, 2009. Retrieved March 9, 2009.
- ↑ Brown, MR: "Analgesic patches and defibrillators: a cautionary tale", Europace,2009 Nov;11(11):1552-3
- ↑ "Combination Products; FAQ". Retrieved April 10, 2012.
Further reading
- "Transderm Scōp" (PDF). Food and Drug Administration. 1998. Archived from the original (PDF) on 2007-08-10. Retrieved 2007-02-12.
External links
| Wikimedia Commons has media related to Transdermal patches. |
- ProSolus Pharmaceuticals - Transdermal development and manufacturing
- Step-by-Step Instruction: How to Use Transdermal Patches
-solution.jpg)


