Hair follicle
| Hair follicle | |
|---|---|
 Hair follicle | |
 A photograph of hair on a human arm emerging from follicles | |
| Details | |
| System | Integumentary system |
| Artery | [relicollies artery |
| Vein | superficial temporal, posterior auricular, occipital |
| Nerve | supratrochlear, supraorbital, greater occipital, lesser occipital |
| Lymph | occipital, mastoid |
| Identifiers | |
| Latin | folliculus pili |
| Code | TH H3.12.00.3.980643 |
| TA | A16.0.00.023 |
| FMA | 70660 |
A hair follicle is a mammalian skin organ that produces hair. Hair production occurs in phases, including growth (anagen), cessation (catagen), and rest (telogen) phases. Stem cells are responsible for hair production. The shape of the hair follicle has an effect on the hair shape and texture of the individual's hair.
Structure

Papilla
The papilla is a large structure at the base of the hair follicle.[1] The papilla is made up mainly of connective tissue and a capillary loop. Cell division in the papilla is either rare or non-existent.
Matrix
Around the papilla is the hair matrix.
Root sheath
The root sheath is composed of an external and internal root sheath. The external root sheath appears empty with cuboid cells when stained with H&E stain. The internal root sheath is composed of three layers, Henle's layer, Huxley's layer, and an internal cuticle that is continuous with the outermost layer of the hair fiber.
Bulge
The bulge is located in the outer root sheath at the insertion point of the arrector pili muscle. It houses several types of stem cells, which supply the entire hair follicle with new cells, and take part in healing the epidermis after a wound.[2][3] Stem cells express the marker LGR5+ in vivo.[4]
Other structures
Other structures associated with the hair follicle include the cup in which the follicle grows known as the infundibulum,[5] the arrector pili muscles, the sebaceous glands, and the apocrine sweat glands. Hair follicle receptors sense the position of the hair.
Attached to the follicle is a tiny bundle of muscle fiber called the arrector pili. This muscle is responsible for causing the follicle lissis to become more perpendicular to the surface of the skin, and causing the follicle to protrude slightly above the surrounding skin (piloerection) and a pore encased with skin oil. This process results in goose bumps (or goose flesh).
Also attached to the follicle is a sebaceous gland, which produces the oily or waxy substance sebum. The higher the density of the hair, the more sebaceous glands that are found.
Morphogenesis
In utero, the epithelium and underlying mesenchyme interact to form hair follicles.[6]
Hair-follicle cycling
Hair grows in cycles of various phases:[7] anagen is the growth phase; catagen is the involuting or regressing phase; and telogen, the resting or quiescent phase (names derived using the greek prefixes ana-, kata-, and telos- meaning up, down, and end respectively). Each phase has several morphologically and histologically distinguishable sub-phases. Prior to the start of cycling is a phase of follicular morphogenesis (formation of the follicle). There is also a shedding phase, or exogen, that is independent of anagen and telogen in which one of several hair that might arise from a single follicle exits. Normally up to 90% of the hair follicles are in anagen phase while, 10–14% are in telogen and 1–2% in catagen. The cycle's length varies on different parts of the body. For eyebrows, the cycle is completed in around 4 months, while it takes the scalp 3–4 years to finish; this is the reason eyebrow hair have a much shorter length limit compared to hair on the head. Growth cycles are controlled by a chemical signal like epidermal growth factor. DLX3 is a crucial regulator of hair follicle differentiation and cycling. Specifically, colocalization of phosphorylated Smad1/5/8 complex and DLX3 regulate role for BMP signaling to Dlx3 during hair morphogenesis in animal models.[8][9]
Anagen phase
Anagen is the active growth phase of hair follicles[10] during which the root of the hair is dividing rapidly, adding to the hair shaft. During this phase the hair grows about 1 cm every 28 days. Scalp hair stays in this active phase of growth for 2–7 years and is genetically determined. At the end of the anagen phase an unknown signal causes the follicle to go into the catagen phase.
Catagen phase
The catagen phase is a short transition stage that occurs at the end of the anagen phase.[11] It signals the end of the active growth of a hair. This phase lasts for about 2–3 weeks while the hair converts to a club hair. A club hair is formed during the catagen phase when the part of the hair follicle in contact with the lower portion of the hair becomes attached to the hair shaft. This process cuts the hair off from its blood supply and from the cells that produce new hair. When a club hair is completely formed, about a 2-week process, the hair follicle enters the telogen phase.
Telogen phase
The telogen phase is the resting phase of the hair follicle.[12] When the body is subjected to extreme stress, as much as 70 percent of hair can prematurely enter a phase of rest, called the telogen phase. This hair begins to fall, causing a noticeable loss of hair. This condition is called telogen effluvium.[13] The club hair is the final product of a hair follicle in the telogen stage, and is a dead, fully keratinized hair.[6] Fifty to one-hundred club hair are shed daily from a normal scalp.[6]
Hair growth cycle times
- Scalp: The time these phases last varies from person to person. Different hair color and follicle shape affects the timings of these phases.
- anagen phase, 2–8 years (occasionally much longer)
- catagen phase, 2–3 weeks
- telogen phase, around 3 months
- Eyebrows etc.:
- anagen phase, 4–7 months
- catagen phase, 3–4 weeks
- telogen phase, about 9 months
Hair follicles in hair restoration
Hair follicles form the basis of the two primary methods of hair transplantation in hair restoration, Follicular Unit Transplantation (FUT) and Follicular Unit Extraction (FUE). In each of these methods, naturally-occurring groupings of one to four hairs, called follicular units, are extracted from the hair restoration patient and then surgically implanted in the balding area of the patient's scalp, known as the recipient area. These follicles are extracted from donor areas of the scalp, or other parts of the body, which are typically resistant to the miniaturization effects of the hormone DHT. It is this miniaturization of the hair shaft that is the primary predictive indicator of androgenetic alopecia,[14] commonly referred to as male pattern baldness or male hair loss. When these DHT-resistant follicles are transplanted to the recipient area, they continue to grow hair in the normal hair cycle, thus providing the hair restoration patient with permanent, naturally-growing hair.
While hair transplantation dates back to the 1950s,[15] and plucked human hair follicle cell culture in vitro to the early 1980s,[16] it was not until 1995 when hair transplantation using individual follicular units was introduced into medical literature.[17]
Additional images
-

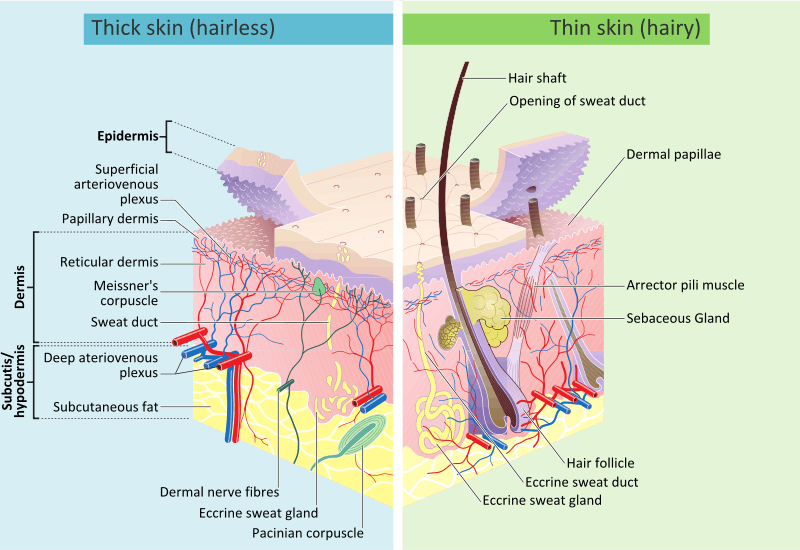
Cross-section of all skin layers
-

Diagram of a hair follicle, from Gray's Anatomy.
-

Hair Follicle
-

Pili multigemini is a malformation characterized by the presence of bifurcated or multiple divided hair matrices and papillae, giving rise to the formation of multiple hair shafts within the individual follicles.
Skin overview
References
- ↑ Pawlina, Wojciech; Ross, Michael W.; Kaye, Gordon I. (2003). Histology: a text and atlas: with cell and molecular biology. Hagerstown, Maryland: Lippincott Williams & Wilkins. ISBN 0-683-30242-6.
- ↑ Ma DR; Yang EN; Lee ST (2004). "A review: the location, molecular characterisation and multipotency of hair follicle epidermal stem cells". Ann. Acad. Med. Singap. 33 (6): 784–8. PMID 15608839.
- ↑ Cotsarelis G (2006). "Epithelial stem cells: a folliculocentric view". J. Invest. Dermatol. 126 (7): 1459–68. doi:10.1038/sj.jid.5700376. PMID 16778814.
- ↑ Lin, K. K.; Andersen, B. (2008). "Have Hair Follicle Stem Cells Shed Their Tranquil Image?". Cell Stem Cell 3 (6): 581–582. doi:10.1016/j.stem.2008.11.005. PMID 19041772.
- ↑ "Histologic Diagnosis of Inflammatory Skin Diseases". Derm101.com.
|chapter=ignored (help) - 1 2 3 Paus R; Cotsarelis G (August 1999). "The biology of hair follicles". N. Engl. J. Med. 341 (7): 491–7. doi:10.1056/NEJM199908123410706. PMID 10441606.
- ↑ K. S. Stenn & R. Paus (1 January 2001). "Controls of Hair Follicle Cycling". Physiological Reviews 81 (1): 449–494. PMID 11152763. (comprehensive topic review, successor to landmark review of 1954 by HB Chase)
- ↑ Hwang, J.; Mehrani, T.; Millar, S. E.; Morasso, M. I. (2008). "Dlx3 is a crucial regulator of hair follicle differentiation and cycling". Development 135 (18): 3149–3159. doi:10.1242/dev.022202. PMC 2707782. PMID 18684741.
- ↑ Park, G. T.; Morasso, M. I. (2002). "Bone morphogenetic protein-2 (BMP-2) transactivates Dlx3 through Smad1 and Smad4: Alternative mode for Dlx3 induction in mouse keratinocytes". Nucleic Acids Research 30 (2): 515–522. doi:10.1093/nar/30.2.515. PMC 99823. PMID 11788714.
- ↑ Brannon, Maryland, Heather. "Anagen Phase". The New York Times. Retrieved 2007-11-14.
- ↑ Brannon, Maryland, Heather. "Categen Phase". The New York Times. Retrieved 2007-11-14.
- ↑ Brannon, Maryland, Heather. "Telogen Phase". The New York Times. Retrieved 2007-11-14.
- ↑
- ↑ Bernstein RM; Rassman WR (September 1997). "Follicular transplantation. Patient evaluation and surgical planning". Dermatol Surg 23 (9): 771–84; discussion 801–5. doi:10.1111/j.1524-4725.1997.tb00417.x. PMID 9311372.
- ↑ Orentreich N (November 1959). "Autografts in alopecias and other selected dermatological conditions". Ann. N. Y. Acad. Sci. 83: 463–79. doi:10.1111/j.1749-6632.1960.tb40920.x. PMID 14429008.
- ↑ Wells J; Sieber VK (December 1985). "Morphological characteristics of cells derived from plucked human hair in vitro". Br. J. Dermatol. 113 (6): 669–75. doi:10.1111/j.1365-2133.1985.tb02402.x. PMID 2420350.
- ↑ Bernstein RM; Rassman WR; Szaniawski W; Halperin A: (1995). "Follicular Transplantation". Intl J Aesthetic Restorative Surgery 3: 119–32. ISSN 1069-5249. OCLC 28084113.
External links
![]() Media related to Hair follicle at Wikimedia Commons
Media related to Hair follicle at Wikimedia Commons
| ||||||||||||||||||||||||||||||||||||||||||||||||