Sulfonylurea
Sulfonylureas (UK: sulphonylurea) are a class of organic compounds used in medicine and agriculture. They are antidiabetic drugs widely used in the management of diabetes mellitus type 2. They act by increasing insulin release from the beta cells in the pancreas. A number of sulfonylureas are also used as herbicides ("weedkiller"), because they can interfere with plant biosynthesis of certain amino acids.
Drugs in this class
- First generation drugs include carbutamide, acetohexamide, chlorpropamide, and tolbutamide.
- Second generation drugs include glipizide (glucotrol), gliclazide, glibenclamide, glyburide (Micronase), glibornuride, gliquidone, glisoxepide, and glyclopyramide.
- Third generation drugs include glimepiride (Amaryl) (Glimiprime), Gliclazide MR (DIAMICRON MR60), although glimepiride is sometimes considered second-generation,[1] while others classify it as third-generation.[2]
- Fourth generation (light-dependent) drugs include JB253[3] and JB558.[4]
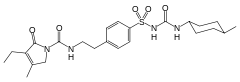
Structure
All pharmacological sulfonylureas contain a central S-arylsulfonylurea structure with a p- substituent on the phenyl ring (R) and various groups terminating the urea N′ end group (R2). Chemically, this functionality can be easily installed by reacting aryl sulfonamides (R-C6H4-SO2NH2) with isocyanates (R2-NCO).


Pharmacology

Sulfonylureas bind to an ATP-sensitive K+(KATP) channel on the cell membrane of pancreatic beta cells. This inhibits a tonic, hyperpolarizing efflux of potassium, thus causing the electric potential over the membrane to become more positive. This depolarization opens voltage-gated Ca2+ channels. The rise in intracellular calcium leads to increased fusion of insulin granulae with the cell membrane, and therefore increased secretion of (pro)insulin.
There is some evidence that sulfonylureas also sensitize β-cells to glucose, that they limit glucose production in the liver, that they decrease lipolysis (breakdown and release of fatty acids by adipose tissue) and decrease clearance of insulin by the liver.
The KATP channel is an octameric complex of the inward-rectifier potassium ion channel Kir6.x and sulfonylurea receptor SUR which associate with a stoichiometry of 4:4.
Furthermore, it has been shown that sulfonylureas interact with the nucleotide exchange factor Epac2.[5][6] Mice lacking this factor exhibited a decreased glucose-lowering effect upon sulfonylurea treatment.
Pharmacokinetics
Various sulfonylureas have different pharmacokinetics. The choice depends on the propensity of the patient to develop hypoglycemia – long-acting sulfonylureas with active metabolites can induce hypoglycemia. They can, however, help achieve glycemic control when tolerated by the patient. The shorter-acting agents may not control blood sugar levels adequately.
Due to varying half-life, some drugs have to be taken two (e.g. tolbutamide) or three times a day rather than once (e.g. glimepiride). The short-acting agents may have to be taken about 30 minutes before the meal, to ensure maximum efficacy when the food leads to increased blood glucose levels.
Some sulfonylureas are metabolised by liver metabolic enzymes (cytochrome P450) and inducers of this enzyme system (such as the antibiotic rifampicin) can therefore increase the clearance of sulfonylureas. In addition, because some sulfonylureas are bound to plasma proteins, use of drugs that also bind to plasma proteins can release the sulfonylureas from their binding places, leading to increased clearance.
Interactions
Drugs that potentiate or prolong the effects of sulfonylureas and therefore increase the risk of hypoglycemia include acetylsalicylic acid and derivatives, allopurinol, sulfonamides, and fibrates. Drugs that worsen glucose tolerance, contravening the effects of antidiabetics, include corticosteroids, isoniazide, oral contraceptives and other estrogens, sympathomimetics, and thyroid hormones. Sulfonylureas tend to interact with a wide variety of other drugs, but these interactions, as well as their clinical significance, vary from substance to substance.[7][8]
Indications
Sulfonylureas are used primarily for the treatment of diabetes mellitus type 2. Sulfonylureas are ineffective where there is absolute deficiency of insulin production such as in type 1 diabetes or post-pancreatectomy.
Sulfonylureas can be used to treat some types of neonatal diabetes. While historically patients with hyperglycemia and low blood insulin levels were diagnosed with Type I Diabetes by default, it has been found that patients who receive this diagnosis before 6 months of age are often, in fact, candidates for receiving sulfonylureas rather than insulin throughout life.[9]
Although for many years sulfonylureas were the first drugs to be used in new cases of diabetes, in the 1990s it was discovered that obese patients might benefit more from metformin.
In about 10% of patients, sulfonylureas alone are ineffective in controlling blood glucose levels. Addition of metformin or a thiazolidinedione may be necessary, or (ultimately) insulin. Triple therapy of sulfonylureas, a biguanide (metformin) and a thiazolidinedione is generally discouraged, but some doctors prefer this combination over resorting to insulin.
More recently, a pharmaceutical startup, Remedy Pharmaceuticals, Inc. has begun developing intravenous glyburide[10] as a treatment for acute stroke, traumatic brain injury and spinal cord injury based on the identification of a non-selective ATP-gated cation channel which is upregulated in neurovascular tissue during these conditions and closed by sulfonylurea agents.[11][12]
Some diabetes experts feel that sulfonylureas accelerate the loss of beta cells from the pancreas, and should be avoided.[13]
Adverse effects and cautions
Sulfonylureas, as opposed to metformin, the thiazolidinediones, exenatide, symlin and other newer treatment agents may induce hypoglycemia as a result of excesses in insulin production and release. This typically occurs if the dose is too high, and the patient is fasting. Some people attempt to change eating habits to prevent this, however it can be counter productive.
Like insulin, sulfonylureas can induce weight gain, mainly as a result of their effect to increase insulin levels and thus utilization of glucose and other metabolic fuels. Other side-effects are: abdominal upset, headache and hypersensitivity reactions.
The safety of sulfonylurea therapy in pregnancy is unestablished. Prolonged hypoglycemia (4 to 10 days) has been reported in children borne to mothers taking sulfonylureas at the time of delivery.[14] Impairment of liver or kidney function increase the risk of hypoglycemia, and are contraindications. As other anti-diabetic drugs cannot be used either under these circumstances, insulin therapy is typically recommended during pregnancy and in hepatic and renal failure, although some of the newer agents offer potentially better options.
A 2014 Cochrane review found tentative evidence that people treated with sulfonylureas have fewer non-fatal cardiovascular events than those treated with metformin (RR 0.67, 95% CI 0.48 to 0.93) but a higher risk of severe hypoglycemia (RR 5.64, 95% CI 1.22 to 26.00). There was not enough data available to determine the relative risk of mortality or of cardiovascular mortality.[15] An earlier review by the same group found a statistically significant increase in the risk of cardiovascular death for first generation sulfonylureas relative to placebo (RR 2.63, 95% CI 1.32 to 5.22; P = 0.006) but there was not enough data to determine the relative risk of first generation sulfonylureas relative to insulin (RR 1.36, 95% CI 0.68 to 2.71; P = 0.39). Likewise it was not possible to determine the relative mortality risk of second generation sulfonylureas relative to metformin (RR 0.98, 95% CI 0.61 to 1.58; P = 0.68), insulin (RR 0.96, 95% CI 0.79 to 1.18; P = 0.72), or placebo.[16] The FDA requires sulfonylureas to carry a label warning regarding increased risk of cardiovascular death.[14]
Second-generation sulfonylureas have increased potency by weight, compared to first-generation sulfonylureas. Similarly, ACCORD (Action to Control Cardiovascular Risk in Diabetes)[17] and the VADT (Veterans Affairs Diabetes Trial)[18] studies showed no reduction in heart attack or death in patients assigned to tight glucose control with various drugs.
History
Sulfonylureas were discovered in 1942 by the chemist Marcel Janbon and co-workers,[19] who were studying sulfonamide antibiotics and discovered that the compound sulfonylurea induced hypoglycemia in animals.[20]
Sulfonylureas used as herbicides
A large number of sulfonylureas are used as herbicides. They function by interfering with biosynthesis of the amino acids valine, isoleucine, and leucine. Some of the brand names of these compounds are amidosulfuron, azimsulfuron, bensulfuron-methyl, chlorimuron-ethyl, chlorsulfuron, ethametsulfuron-methyl, cinosulfuron, ethoxysulfuron, flazasulfuron, flupyrsulfuron-methyl-sodium, imazosulfuron, metsulfuron-methyl, nicosulfuron, oxasulfuron, primisulfuron-methyl, prosulfuron, pyrazosulfuron-ethyl, rimsulfuron, sulfometuron-methyl, sulfosulfuron, thifensulfuron-methyl, triasulfuron, tribenuron-methyl, and triflusulfuron-methyl.[21]
References
- ↑ Triplitt CL, Reasner CA (2011). "Chapter 83: diabetes mellitus". In DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM. Pharmacotherapy: a pathophysiologic approach (8th ed.). New York, NY: McGraw-Hill. p. 1274. ISBN 0-07-170354-3.
- ↑ Davidson J (2000). Clinical diabetes mellitus: a problem-oriented approach. Stuttgart: Thieme. p. 422. ISBN 0-86577-840-X.
- ↑ Broichhagen J, Schönberger M, Cork SC, Frank JA, Marchetti P, Bugliani M, Shapiro AM, Trapp S, Rutter GA, Hodson DJ, Trauner D (2014). "Optical control of insulin release using a photoswitchable sulfonylurea". Nature Communications 5: 5116. doi:10.1038/ncomms6116. PMID 25311795.
- ↑ Broichhagen J, Frank JA, Johnston NR, Mitchell RK, Šmid K, Marchetti P, Bugliani M, Rutter GA, Trauner D, Hodson DJ (Apr 2015). "A red-shifted photochromic sulfonylurea for the remote control of pancreatic beta cell function". Chemical Communications 51 (27): 6018–21. doi:10.1039/C5CC01224D. PMID 25744824.
- ↑ Zhang CL, Katoh M, Shibasaki T, Minami K, Sunaga Y, Takahashi H, Yokoi N, Iwasaki M, Miki T, Seino S (Jul 2009). "The cAMP sensor Epac2 is a direct target of antidiabetic sulfonylurea drugs". Science 325 (5940): 607–10. doi:10.1126/science.1172256. PMID 19644119.
- ↑ Takahashi T, Shibasaki T, Takahashi H, Sugawara K, Ono A, Inoue N, Furuya T, Seino S (Oct 2013). "Antidiabetic sulfonylureas and cAMP cooperatively activate Epac2A". Science Signaling 6 (298): ra94. doi:10.1126/scisignal.2004581. PMID 24150255.
- ↑ Haberfeld, H, ed. (2009). Austria-Codex (in German) (2009/2010 ed.). Vienna: Österreichischer Apothekerverlag. ISBN 3-85200-196-X.
- ↑ Dinnendahl V, Fricke U, eds. (2010). Arzneistoff-Profile (in German) 4 (23 ed.). Eschborn, Germany: Govi Pharmazeutischer Verlag. ISBN 978-3-7741-9846-3.
- ↑ Greeley SA, Tucker SE, Naylor RN, Bell GI, Philipson LH (Aug 2010). "Neonatal diabetes mellitus: a model for personalized medicine". Trends in Endocrinology and Metabolism 21 (8): 464–72. doi:10.1016/j.tem.2010.03.004. PMID 20434356.
- ↑ "Breakthrough Discovery Offers Hope to Stroke Victims". Carrot Capital. Retrieved 2008-01-06.
- ↑ Kunte H, Schmidt S, Eliasziw M, del Zoppo GJ, Simard JM, Masuhr F, Weih M, Dirnagl U (Sep 2007). "Sulfonylureas improve outcome in patients with type 2 diabetes and acute ischemic stroke". Stroke; A Journal of Cerebral Circulation 38 (9): 2526–30. doi:10.1161/STROKEAHA.107.482216. PMC 2742413. PMID 17673715.
- ↑ Simard JM, Woo SK, Bhatta S, Gerzanich V (Feb 2008). "Drugs acting on SUR1 to treat CNS ischemia and trauma". Current Opinion in Pharmacology 8 (1): 42–9. doi:10.1016/j.coph.2007.10.004. PMC 2265539. PMID 18032110.
- ↑ (Maedler K, Carr RD, Bosco D, Zuellig RA, Berney T, Donath MY (2005). Sulfonylurea induced beta-cell apoptosis in cultured human islets" J Clin Endocrinol Metab 90:501–506).
- 1 2 "www.accessdata.fda.gov" (PDF).
- ↑ Hemmingsen B, Schroll JB, Wetterslev J, Gluud C, Vaag A, Sonne DP, Lundstrøm LH, Almdal T (Jul 2014). "Sulfonylurea versus metformin monotherapy in patients with type 2 diabetes: a Cochrane systematic review and meta-analysis of randomized clinical trials and trial sequential analysis". CMAJ Open 2 (3): E162–75. doi:10.9778/cmajo.20130073. PMC 4185978. PMID 25295236.
- ↑ Hemmingsen B, Schroll JB, Lund SS, Wetterslev J, Gluud C, Vaag A, Sonne DP, Lundstrøm LH, Almdal T (2013). "Sulphonylurea monotherapy for patients with type 2 diabetes mellitus". The Cochrane Database of Systematic Reviews 4: CD009008. doi:10.1002/14651858.CD009008.pub2. PMID 23633364.
- ↑ Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH, Probstfield JL, Simons-Morton DG, Friedewald WT (Jun 2008). "Effects of intensive glucose lowering in type 2 diabetes". The New England Journal of Medicine 358 (24): 2545–59. doi:10.1056/NEJMoa0802743. PMID 18539917.
- ↑ Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD (Jan 2009). "Glucose control and vascular complications in veterans with type 2 diabetes". The New England Journal of Medicine 360 (2): 129–39. doi:10.1056/NEJMoa0808431. PMID 19092145.
- ↑ Janbon M, Chaptal J, Vedel A, Schaap J (1942). "Accidents hypoglycémiques graves par un sulfamidothiodiazol (le VK 57 ou 2254 RP)". Montpellier Med. 441: 21–22.
- ↑ Patlak M (Dec 2002). "New weapons to combat an ancient disease: treating diabetes". FASEB Journal 16 (14): 1853. doi:10.1096/fj.02-0974bkt. PMID 12468446.
- ↑ Arnold P. Appleby, Franz Müller, Serge Carpy "Weed Control" in Ullmann's Encyclopedia of Industrial Chemistry 2002, Wiley-VCH, Weinheim. doi:10.1002/14356007.a28_165
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||