Sterilization (microbiology)
Sterilization (or sterilisation) is a term referring to any process that eliminates (removes) or kills (deactivates) all forms of life and other biological agents (such as prions, as well as viruses which some do not consider to be alive but are biological pathogens nonetheless), including transmissible agents (such as fungi, bacteria, viruses, prions, spore forms,unicellular eukaryotic organisms such as Plasmodium, etc.) present in a specified region, such as a surface, a volume of fluid, medication, or in a compound such as biological culture media.[1][2] Sterilization can be achieved with one or more of the following: heat, chemicals, irradiation, high pressure, and filtration. Sterilization is distinct from disinfection, sanitization, and pasteurization in that sterilization kills, deactivates, or eliminates all forms of life and other biological agents.
Applications
Foods
One of the first steps toward sterilization was made by Nicolas Appert who discovered that thorough application of heat over a suitable period slowed the decay of foods and various liquids, preserving them for safe consumption for a longer time than was typical. Canning of foods is an extension of the same principle, and has helped to reduce food borne illness ("food poisoning"). Other methods of sterilizing foods include food irradiation[3] and high pressure (pascalization).[4]
Medicine and surgery


In general, surgical instruments and medications that enter an already aseptic part of the body (such as the bloodstream, or penetrating the skin) must be sterile. Examples of such instruments include scalpels, hypodermic needles and artificial pacemakers. This is also essential in the manufacture of parenteral pharmaceuticals.
Preparation of injectable medications and intravenous solutions for fluid replacement therapy requires not only sterility but also well-designed containers to prevent entry of adventitious agents after initial product sterilization.
Spacecraft
There are strict international rules to protect the contamination of Solar System bodies from biological material from Earth. Standards vary depending on both the type of mission and its destination; the more likely a planet is considered to bear life, the stricter the requirements are.
Many components of instruments used on spacecraft cannot withstand very high temperatures, so techniques not requiring excessive temperatures are used as tolerated, including heating to at least 120 °C, chemical sterilization, oxidization, ultraviolet, and irradiation.[5]
Quantification
The aim of sterilization is the reduction of initially present microorganisms or other potential pathogens. The degree of sterilization is commonly expressed by multiples of the decimal reduction time, or D-value, denoting the time needed to reduce the initial number  to one tenth (
to one tenth ( ) of its original value.[6] Then the number of microorganisms
) of its original value.[6] Then the number of microorganisms  after sterilization time
after sterilization time  is given by:
is given by:
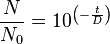 .
.
The D-value is a function of sterilization conditions and varies with the type of microorganism, temperature, water activity, pH etc.. For steam sterilization (see below) typically the temperature (in °Celsius) is given as index.
Theoretically, the likelihood of survival of an individual microorganism is never zero. To compensate for this, the overkill method is often used. Using the overkill method, sterilization is performed by sterilizing for longer than is required to kill the bioburden present on or in the item being sterilized. This provides a sterility assurance level (SAL) equal to the probability of a non-sterile unit.
For high-risk applications such as medical devices and injections, a sterility assurance level of at least 10−6 is required by the United States Food and Drug Administration (FDA)[7]
Heat
Steam
.jpg)
A widely used method for heat sterilization is the autoclave, sometimes called a converter or steam sterilizer. Autoclaves use steam heated to 121-134 °C under pressure. To achieve sterility, the article is heated in a chamber by injected steam until the article reaches a time and temperature setpoint. The article is then held at that setpoint for a period of time which varies depending on the bioburden present on the article being sterilized and its resistance (D-value) to steam sterilization. A general cycle is 20 minutes at 121 °C at 100 kPa, which is sufficient to provide a sterility assurance level of 10−4 for a product with a bioburden of 106 and a D-value of 2.0 minutes.[8] Following sterilization, liquids in a pressurized autoclave must be cooled slowly to avoid boiling over when the pressure is released. This may be achieved by gradually depressurizing the sterilization chamber and allowing liquids to evaporate under a negative pressure, while cooling the contents.
Proper autoclave treatment will inactivate all resistant bacterial spores in addition to fungi, bacteria, and viruses, but is not expected to eliminate all prions, which vary in their resistance. For prion elimination, various recommendations state 121-132 °C for 60 minutes or 134 °C for at least 18 minutes. The 263K scrapie prion is inactivated relatively quickly by such sterilization procedures; however, other strains of scrapie, and strains of CJD and BSE are more resistant. Using mice as test animals, one experiment showed that heating BSE positive brain tissue at 134-138 °C for 18 minutes resulted in only a 2.5 log decrease in prion infectivity.
Most autoclaves have meters and charts that record or display information, particularly temperature and pressure as a function of time. The information is checked to ensure that the conditions required for sterilization have been met. Indicator tape is often placed on packages of products prior to autoclaving, and some packaging incorporates indicators. The indicator changes color when exposed to steam, providing a visual confirmation.
Biological indicators can also be used to independently confirm autoclave performance. Simple bioindicator devices are commercially available based on microbial spores. Most contain spores of the heat resistant microbe Geobacillus stearothermophilus (formerly Bacillus stearothermophilus), which is extremely resistant to steam sterilization. Biological indicators may take the form of glass vials of spores and liquid media, or as spores on strips of paper inside glassine envelopes. These indicators are placed in locations where it is difficult for steam to reach to verify that steam is penetrating there.
For autoclaving, cleaning is critical. Extraneous biological matter or grime may shield organisms from steam penetration. Proper cleaning can be achieved through physical scrubbing, sonication, ultrasound or pulsed air. [9] Pressure cooking and canning are analogous to autoclaving, and when performed correctly renders food sterile.
Moist heat causes destruction of micro-organisms by denaturation of macromolecules, primarily proteins. This method is a faster process than dry heat sterilization.
Dry Heat
Dry heat was the first method of sterilization, and is a longer process than moist heat sterilization. The destruction of microorganisms through the use of dry heat is a gradual phenomenon. With longer exposure to lethal temperatures, the number of killed microorganisms increases. Forced ventilation of hot air can be used to increase the rate at which heat is transferred to an organism and reduce the temperature and amount of time needed to achieve sterility. At higher temperatures, shorter exposure times are required to kill organisms. This can reduce heat-induced damage to food products.[10]
The standard setting for a hot air oven is at least two hours at 160 °C. A rapid method heats air to 190 °C for 6 minutes for unwrapped objects and 12 minutes for wrapped objects.[11][12] Dry heat has the advantage that it can be used on powders and other heat-stable items that are adversely affected by steam (e.g. it does not cause rusting of steel objects).
Flaming
Flaming is done to loops and straight-wires in microbiology labs. Leaving the loop in the flame of a Bunsen burner or alcohol lamp until it glows red ensures that any infectious agent gets inactivated. This is commonly used for small metal or glass objects, but not for large objects (see Incineration below). However, during the initial heating infectious material may be "sprayed" from the wire surface before it is killed, contaminating nearby surfaces and objects. Therefore, special heaters have been developed that surround the inoculating loop with a heated cage, ensuring that such sprayed material does not further contaminate the area. Another problem is that gas flames may leave carbon or other residues on the object if the object is not heated enough. A variation on flaming is to dip the object in 70% or higher ethanol, then briefly touch the object to a Bunsen burner flame. The ethanol will ignite and burn off rapidly, leaving less residue than a gas flame.
Incineration
Incineration is a waste treatment process that involves the combustion of organic substances contained in waste materials. This method also burns any organism to ash. It is used to sterilize medical and other biohazardous waste before it is discarded with non-hazardous waste. Bacteria incinerators are mini furnaces used to incinerate and kill off any micro organisms that may be on an inoculating loop or wire.[13]
Tyndallization
Named after John Tyndall, Tyndallization[14] is an obsolete and lengthy process designed to reduce the level of activity of sporulating bacteria that are left by a simple boiling water method. The process involves boiling for a period (typically 20 minutes) at atmospheric pressure, cooling, incubating for a day, then repeating the process a total of three to four times. The incubation periods are to allow heat-resistant spores surviving the previous boiling period to germinate to form the heat-sensitive vegetative (growing) stage, which can be killed by the next boiling step. This is effective because many spores are stimulated to grow by the heat shock. The procedure only works for media that can support bacterial growth, and will not sterilize non-nutritive substrates like water. Tyndallization is also ineffective against prions.
Glass bead sterilizers
Glass bead sterilizers work by heating glass beads to 250 °C. Instruments are then quickly doused in these glass beads, which heat the object while physically scraping contaminants off their surface. Glass bead sterilizers were once a common sterilization method employed in dental offices as well as biologic laboratories,[15] but are not approved by the U.S. Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) to be used as a sterilizers since 1997.[16] They are still popular in European as well as Israeli dental practices although there are no current evidence-based guidelines for using this sterilizer.[15]
Chemical sterilization
Chemicals are also used for sterilization. Heating provides a reliable way to rid objects of all transmissible agents, but it is not always appropriate if it will damage heat-sensitive materials such as biological materials, fiber optics, electronics, and many plastics. In these situations chemicals, either as gases or in liquid form, can be used as sterilants. While the use of gas and liquid chemical sterilants avoids the problem of heat damage, users must ensure that article to be sterilized is chemically compatible with the sterilant being used. In addition, the use of chemical sterilants poses new challenges for workplace safety, as the properties that make chemicals effective sterilants usually make them harmful to humans.
Ethylene oxide
Ethylene oxide (EO or EtO) gas is commonly used to sterilize objects that are sensitive to temperatures greater than 60 °C and / or radiation such as plastics, optics and electrics. Besides moist heat and irradiation, ethylene oxide is the most common sterilization method, used for over 70% of total sterilizations, and for 50% of all disposable medical devices .
Ethylene oxide treatment is generally carried out between 30 °C and 60 °C with relative humidity above 30% and a gas concentration between 200 and 800 mg/l, and typically lasts for at least three hours. Ethylene oxide penetrates well, moving through paper, cloth, and some plastic films and is highly effective. Ethylene oxide can kill all known viruses, bacteria (including spores) and fungi, and is compatible with most materials even when repeatedly applied. However, it is highly flammable, toxic and carcinogenic with a potential to cause adverse reproductive effects. Ethylene oxide sterilizers require biological validation after sterilization installation, repairs or process failure.
A typical process consists of a preconditioning phase, an exposure phase, and a period of post-sterilization aeration to remove ethylene oxide residues and by-products such as ethylene glycol and ethylene chlorohydrine.
The two most important ethylene oxide sterilization methods are: (1) the gas chamber method and (2) the micro-dose method. To benefit from economies of scale, ethylene oxide has traditionally been delivered by flooding a large chamber with a combination of ethylene oxide and other gases used as diluents (usually CFCs or carbon dioxide). Drawbacks of this method include air contamination produced by CFC's and ethylene oxide residuals, operator exposure risks, training costs and flammability issues requiring special handling and storage.
Ethylene oxide is still widely used by medical device manufacturers for larger scale sterilization, but ethylene oxide is becoming less popular in hospitals . Since ethylene oxide is explosive at concentrations from 3% to 100% , ethylene oxide was traditionally supplied with an inert carrier gas such as a CFC or halogenated hydrocarbon. The use of CFCs as the carrier gas was banned because of concerns of ozone depletion[17] and halogenated hydrocarbons are being replaced by systems using 100% ethylene oxide because of the much greater cost of the blends. In hospitals, most ethylene oxide sterilizers use single use cartridges (e.g. 3M's Steri-Vac line,[18] or STERIS Corporation's Stericert sterilizers[19]) because of the convenience and ease of use compared to the former plumbed gas cylinders of ethylene oxide blends. Another method using 100% ethylene oxide is the micro-dose sterilization method, developed in the late 1950s, using a specially designed bag to eliminate the need to flood a larger chamber with ethylene oxide. This method is also known as gas diffusion sterilization, or bag sterilization. This method minimizes the use of gas.[20]
Other reasons for the decrease in use of ethylene oxide are the well-known health effects. In addition to being a primary irritant, ethylene oxide is now classified by the IARC as a known human carcinogen.[21] The US OSHA has set the permissible exposure limit (PEL) at 1 ppm calculated as an eight-hour time weighted average (TWA) [29 CFR 1910.1047] and 5 ppm as a 15-minute TWA. The NIOSH Immediately dangerous to life and health limit for ethylene oxide is 800 ppm.[22] The odor threshold is around 500 ppm[23] and so ethylene oxide is imperceptible until concentrations well above the OSHA PEL. Therefore, OSHA recommends that continuous gas monitoring systems be used to protect workers using ethylene oxide for sterilization.[24] Employees health records must be maintained during employment and after termination of employment for 30 years.
Nitrogen dioxide
Nitrogen dioxide (NO2) gas is a rapid and effective sterilant for use against a wide range of microorganisms, including common bacteria, viruses, and spores. The unique physical properties of NO2 gas allow for sterilant dispersion in an enclosed environment at room temperature and ambient pressure. The mechanism for lethality is the degradation of DNA in the spore core through nitration of the phosphate backbone, which kills the exposed organism as it absorbs NO2. This degradation occurs at even very low concentrations of the gas.[25] NO2 has a boiling point of 21 °C at sea level, which results in a relatively high saturated vapor pressure at ambient temperature. Because of this, liquid NO2 may be used as a convenient source for the sterilant gas. Liquid NO2 is often referred to by the name of its dimer, dinitrogen tetroxide (N2O4). Additionally, the low levels of concentration required, coupled with the high vapor pressure, assures that no condensation occurs on the devices being sterilized. This means that no aeration of the devices is required immediately following the sterilization cycle.[26] NO2 is also less corrosive than other sterilant gases, and is compatible with most medical materials and adhesives.[26]
The most-resistant organism (MRO) to sterilization with NO2 gas is the spore of Geobacillus stearothermophilus, which is the same MRO for both steam and hydrogen peroxide sterilization processes. The spore form of G. stearothermophilus has been well characterized over the years as a biological indicator in sterilization applications. Microbial inactivation of G. stearothermophilus with NO2 gas proceeds rapidly in a log-linear fashion, as is typical of other sterilization processes. Noxilizer, Inc. has commercialized this technology to offer contract sterilization services for medical devices at its Baltimore, MD facility.[27] This has been demonstrated in Noxilizer’s lab in multiple studies and is supported by published reports from other labs. These same properties also allow for quicker removal of the sterilant and residuals through aeration of the enclosed environment. The combination of rapid lethality and easy removal of the gas allows for shorter overall cycle times during the sterilization (or decontamination) process and a lower level of sterilant residuals than are found with other sterilization methods.[26]
Ozone
Ozone is used in industrial settings to sterilize water and air, as well as a disinfectant for surfaces. It has the benefit of being able to oxidize most organic matter. On the other hand, it is a toxic and unstable gas that must be produced on-site, so it is not practical to use in many settings.
Ozone offers many advantages as a sterilant gas; ozone is a very efficient sterilant because of its strong oxidizing properties (E = 2.076 vs SHE[28]) capable of destroying a wide range of pathogens, including prions without the need for handling hazardous chemicals since the ozone is generated within the sterilizer from medical grade oxygen. The high reactivity of ozone means that waste ozone can be destroyed by passing over a simple catalyst that reverts it to oxygen and ensures that the cycle time is relatively short. The disadvantage of using ozone is that the gas is very reactive and very hazardous. The NIOSH immediately dangerous to life and health limit for ozone is 5 ppm, 160 times smaller than the 800 ppm IDLH for ethylene oxide. Documentation for Immediately Dangerous to Life or Health Concentrations (IDLH): NIOSH Chemical Listing and Documentation of Revised IDLH Values (as of 3/1/95)[29] and OSHA has set the PEL for ozone at 0.1 ppm calculated as an 8 hour time weighted average (29 CFR 1910.1000, Table Z-1). The Canadian Center for Occupation Health and Safety provides an excellent summary of the health effects of exposure to ozone. The sterilant gas manufacturers include many safety features in their products but prudent practice is to provide continuous monitoring to below the OSHA PEL to provide a rapid warning in the event of a leak. Monitors for determining workplace exposure to ozone are commercially available.
Glutaraldehyde and formaldehyde
Glutaraldehyde and formaldehyde solutions (also used as fixatives) are accepted liquid sterilizing agents, provided that the immersion time is sufficiently long. To kill all spores in a clear liquid can take up to 22 hours with glutaraldehyde and even longer with formaldehyde. The presence of solid particles may lengthen the required period or render the treatment ineffective. Sterilization of blocks of tissue can take much longer, due to the time required for the fixative to penetrate. Glutaraldehyde and formaldehyde are volatile, and toxic by both skin contact and inhalation. Glutaraldehyde has a short shelf life (<2 weeks), and is expensive. Formaldehyde is less expensive and has a much longer shelf life if some methanol is added to inhibit polymerization to paraformaldehyde, but is much more volatile. Formaldehyde is also used as a gaseous sterilizing agent; in this case, it is prepared on-site by depolymerization of solid paraformaldehyde. Many vaccines, such as the original Salk polio vaccine, are sterilized with formaldehyde.
Hydrogen peroxide
Hydrogen peroxide, in both liquid and as vaporized hydrogen peroxide (VHP), is another chemical sterilizing agent. Hydrogen peroxide is strong oxidant, which allows it to destroy a wide range of pathogens. Hydrogen peroxide is used to sterilize heat or temperature sensitive articles such as rigid endoscopes. In medical sterilization hydrogen peroxide is used at higher concentrations, ranging from around 35% up to 90%. The biggest advantage of hydrogen peroxide as a sterilant is the short cycle time. Whereas the cycle time for ethylene oxide may be 10 to 15 hours, some modern hydrogen peroxide sterilizers have a cycle time as short as 28 minutes.[30]
Drawbacks of hydrogen peroxide include material compatibility, a lower capability for penetration and operator health risks. Products containing cellulose, such as paper, cannot be sterilized using VHP and products containing nylon may become brittle.[31] The penetrating ability of hydrogen peroxide is not as good as ethylene oxide and so there are limitations on the length and diameter of lumens that can be effectively sterilized and guidance is available from the sterilizer manufacturers. Hydrogen peroxide is primary irritant and the contact of the liquid solution with skin will cause bleaching or ulceration depending on the concentration and contact time. It is relatively non-toxic when diluted to low concentrations, but is a dangerous oxidizer at high concentrations (> 10% w/w). The vapor is also hazardous, primarily affecting the eyes and respiratory system. Even short term exposures can be hazardous and NIOSH has set the Immediately Dangerous to Life and Health Level (IDLH) at 75 ppm,[22] less than one tenth the IDLH for ethylene oxide (800 ppm). Prolonged exposure to lower concentrations can cause permanent lung damage and consequently OSHA has set the permissible exposure limit to 1.0 ppm, calculated as an 8-hour time weighted average.[32] Sterilizer manufacturers go to great lengths to make their products safe through careful design and incorporation of many safety features, though there are still workplace exposures of hydrogen peroxide from gas sterilizers are documented in the FDA MAUDE database.[33] When using any type of gas sterilizer, prudent work practices will include good ventilation, a continuous gas monitor for hydrogen peroxide and good work practices and training.[34][35]
Vaporized hydrogen peroxide (VHP) is used to sterilize large enclosed and sealed areas such as entire rooms and aircraft interiors.
Peracetic acid
Peracetic acid (0.2%) is a recognized sterilant by the FDA[36] for use in sterilizing medical devices such as endoscopes.
Potential for chemical sterilization of prions
Prions are highly resistant to chemical sterilization. Treatment with aldehydes such as formaldehyde have actually been shown to increase prion resistance. Hydrogen peroxide (3%) for one hour was shown to be ineffective, providing less than 3 logs (10−3) reduction in contamination. Iodine, formaldehyde, glutaraldehyde and peracetic acid also fail this test (one hour treatment). Only chlorine, phenolic compounds, guanidinium thiocyanate, and sodium hydroxide (NaOH) reduce prion levels by more than 4 logs; chlorine (too corrosive to use on certain objects) and NaOH are the most consistent. Many studies have shown the effectiveness of sodium hydroxide.[37]
Radiation sterilization
Sterilization can be achieved using electromagnetic radiation such as electron beams, X-rays, gamma rays, or irradiation by subatomic particles.[38] Electromagnetic or particulate radiation can be energetic enough to ionize atoms or molecules (ionizing radiation), or less energetic (non-ionizing radiation).
Non-ionizing radiation sterilization
Ultraviolet light irradiation (UV, from a germicidal lamp) is useful for sterilization of surfaces and some transparent objects. Many objects that are transparent to visible light absorb UV. UV irradiation is routinely used to sterilize the interiors of biological safety cabinets between uses, but is ineffective in shaded areas, including areas under dirt (which may become polymerized after prolonged irradiation, so that it is very difficult to remove). It also damages some plastics, such as polystyrene foam if exposed for prolonged periods of time.
Ionizing radiation sterilization

The safety of irradiation facilities is regulated by the United Nations International Atomic Energy Agency and monitored by the different national Nuclear Regulatory Commissions. The incidents that have occurred in the past are documented by the agency and thoroughly analyzed to determine root cause and improvement potential. Such improvements are then mandated to retrofit existing facilities and future design.
Gamma radiation is very penetrating, and is commonly used for sterilization of disposable medical equipment, such as syringes, needles, cannulas and IV sets, and food. It is emitted by a radioisotope, usually Cobalt-60(60Co) or caesium-137 (137Cs).
Use of a radioisotope requires shielding for the safety of the operators while in use and in storage. With most designs the radioisotope is lowered into a water-filled source storage pool, which absorbs radiation and allows maintenance personnel to enter the radiation shield. One variant keeps the radioisotope under water at all times and lowers the product to be irradiated into the water towards the source in hermetic bells; no further shielding is required for such designs. Other uncommonly used designs use dry storage, providing movable shields that reduce radiation levels in areas of the irradiation chamber. An incident in Decatur Georgia, US, where water-soluble caesium-137 leaked into the source storage pool, requiring NRC intervention[39] has led to use of this radioisotope being almost entirely discontinued in favour of the more costly, non-water-soluble cobalt-60. Cobalt-60 gamma photons have about twice the energy, and hence greater penetrating range, of Caesium-137 radiation.
Electron beam processing is also commonly used for sterilization. Electron beams use an on-off technology and provide a much higher dosing rate than gamma or x-rays. Due to the higher dose rate, less exposure time is needed and thereby any potential degradation to polymers is reduced. A limitation is that electron beams are less penetrating than either gamma or x-rays. Facilities rely on substantial concrete shields to protect workers and the environment from radiation exposure.
X-rays: high-energy X-rays (produced by bremsstrahlung) allow irradiation of large packages and pallet loads of medical devices. They are sufficiently penetrating to treat multiple pallet loads of low-density packages with very good dose uniformity ratios. X-ray sterilization does not require chemical or radioactive material: high-energy X-rays are generated at high intensity by an X-ray generator that does not require shielding when not in use. X-rays are generated by bombarding a dense material (target) such as tantalum or tungsten with high-energy electrons in a process known as bremsstrahlung conversion. These systems are energy-inefficient, requiring much more electrical energy than other systems for the same result.
Irradiation with X-rays or gamma rays, electromagnetic radiation rather than particles, does not make materials radioactive. Irradiation with particles may make materials radioactive, depending upon the type of particles and their energy, and the type of target material: neutrons and very high-energy particles can make materials radioactive, but have good penetration, whereas lower energy particles (other than neutrons) cannot make materials radioactive, but have poorer penetration.
Sterilization by irradiation with gamma rays may however in some cases affect material properties.[40]
Irradiation is used by the United States Postal Service to sterilize mail in the Washington, D.C. area. Some foods (e.g. spices, ground meats) are sterilized by irradiation.
Subatomic particles may be more or less penetrating, and may be generated by a radioisotope or a device, depending upon the type of particle.
Sterile filtration
Fluids that would be damaged by heat, irradiation or chemical sterilization, such as drug products, can be sterilized by microfiltration using membrane filters. This method is commonly used for heat labile pharmaceuticals and protein solutions in medicinal drug processing. A microfilter with pore size 0.2 µm will usually effectively remove microorganisms.[41] In the processing of biologics, viruses must be removed or inactivated, requiring the use of nanofilters with a smaller pore size (20 -50 nm) are used. Smaller pore sizes lower the flow rate, so in order to achieve higher total throughput or to avoid premature blockage, pre-filters might be used to protect small pore membrane filters.
Membrane filters used in production processes are commonly made from materials such as mixed cellulose ester or polyethersulfone (PES). The filtration equipment and the filters themselves may be purchased as pre-sterilized disposable units in sealed packaging, or must be sterilized by the user, generally by autoclaving at a temperature that does not damage the fragile filter membranes. To ensure proper functioning of the filter, the membrane filters are integrity tested post-use and sometimes before use. The non-destructive integrity test assures the filter is undamaged, and is a regulatory requirement.[42] Typically, terminal pharmaceutical sterile filtration is performed inside of a cleanroom to prevent contamination.
Preservation of sterility

Instruments that have undergone sterilization can be maintained in such condition by containment in sealed packaging until use.
Aseptic technique is the act of maintaining sterility during procedures.
See also
- Antibacterial soap
- Asepsis
- Aseptic processing
- Contamination control
- Electron irradiation
- Food and Bioprocess Technology
- Food chemistry
- Food engineering
- Food microbiology
- Food packaging
- Food preservation
- Food rheology
- Food safety
- Food storage
- Food technology
References
- ↑ WHO Glossary
- ↑ UCLA Dept. Epidemiology: Definitions
- ↑ Molins, Ricardo A. (2001). Food irradiation: principles and applications. Wiley-IEEE. p. 23. ISBN 978-0-471-35634-9.
- ↑ Brown, Amy Christian (2007). Understanding Food: Principles and Preparation (3 ed.). Cengage Learning. p. 546. ISBN 978-0-495-10745-3.
- ↑ "No bugs please, this is a clean planet!". European Space Agency. 30 July 2002. Retrieved 7 August 2014.
- ↑ "Guidance for Industry: Biological Indicators". United States Food and Drug Administration. 4 October 2007.
- ↑ "Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing" (PDF). United States Food and Drug Administration. September 2004.
- ↑ "Steam Sterilization Principles". STERIS Life Sciences. November 2013.
- ↑ "Decontamination and Sterilization". NIH.
- ↑ Casolari, A. "FOOD STERILIZATION BY HEAT". Liberty Knowledge Reason.
- ↑ "– Alberta Health and Wellness" (PDF). Health.gov.ab.ca. Retrieved 2010-06-25.
- ↑ Dental Volume 1 - Dentist training manual for military dentists
- ↑ Incineration
- ↑ Thiel, Theresa (1999). "Sterilization of Broth Media by Tyndallization" (PDF). Science in the Real World. Retrieved 2007-03-06.
- 1 2 Zadik Y, Peretz A (Apr 2008). "The effectiveness of glass bead sterilizer in the dental practice". J Isr Dent Assoc 25 (2): 36–9. PMID 18780544.
- ↑ http://www.CDC.gov/OralHealth/InfectionControl/faq/bead.htm 2008-09-11
- ↑ "Substitute Sterilants under SNAP as of September 28, 2006" (PDF). Retrieved 2010-06-25.
- ↑ "Sterilization/Aeration Equipment". Solutions.3m.com. Retrieved 2010-06-25.
- ↑ "Unique solutions for infection control, sterile processing, SPD, and sterilization: EtO Sterilization Solutions". SteriCert. Retrieved 2010-06-25.
- ↑ Micro-dose sterilization method
- ↑ "IARC Vol 60" (PDF). Retrieved 2010-06-25.
- 1 2 "NIOSH: Documentation for Immediately Dangerous to Life or Health Concentrations (IDLH) / NIOSH Chemical Listing and Documentation of Revised IDLH Values (as of 3/1/95) - intridl4". Cdc.gov. Retrieved 2010-06-25.
- ↑ "ATSDR - MMG: Ethylene Oxide". Atsdr.cdc.gov. 2007-09-24. Retrieved 2010-06-25.
- ↑ "Hospital eTool: Central Supply Module". Osha.gov. Retrieved 2010-06-25.
- ↑ Görsdorf S, Appel KE, Engeholm C, Obe G.; Nitrogen dioxide induces DNA single-strand breaks in cultured Chinese hamster cells: Carcinogenesis. 1990.
- 1 2 3 "Mechanism Overview, June 2012" (PDF). noxilizer.com. Noxilizer, Inc. Retrieved 2 July 2013.
- ↑ "Noxilizer Contract Sterilization Services". noxilizer.com. Noxilizer, Inc. Retrieved 2 July 2013.
- ↑ CRC Handbook of Chemistry and Physics, 76th Ed. 1995.
- ↑ http://www.cdc.gov/niosh/idlh/intridl4.html
- ↑ "Sterrad NX". Retrieved 25 March 2015.
- ↑ "Guidelines for Disinfection" (PDF). Center for Disease Control. 2008.
- ↑ "29 CFR 1910.1000 Table Z-1". Occupational Safety and Health Administration. Retrieved 25 March 2015.
- ↑ "MAUDE - Manufacturer and User Facility Device Experience". Accessdata.fda.gov. Retrieved 2010-06-25.
- ↑ "Occupational Safety and Health Guideline for Hydrogen Peroxide". Osha.gov. Retrieved 2010-06-25.
- ↑ "ATSDR - MMG: Hydrogen Peroxide". Atsdr.cdc.gov. 2007-09-24. Retrieved 2010-06-25.
- ↑ "Cleared Sterilants and High Level Disinfectants with General Claims for Processing Reusable Medical and Dental Devices". United States Food and Drug Administration. March 2015.
- ↑ Bauman, PA; Lawrence LA; Biesert L; Dichtelmüller H; Fabbrizzi F; Gajardo R; Gröner A; Jorquera JI; Kempf C; Kreil TR; von Hoegen I; Pifat DY; Petteway SR Jr; MCai K (July 2006). "Critical factors influencing prion inactivation by sodium hydroxide.". Vox Sang 91 (1): 34–40. doi:10.1111/j.1423-0410.2006.00790.x. PMID 16756599.
- ↑ Trends in Radiation Sterilization of Health Care Products, IAEA, Vienna,24 September 2008
- ↑ Information Notice No. 89-82: RECENT SAFETY-RELATED INCIDENTS AT LARGE IRRADIATORS
- ↑ Bharati, S; Soundrapandian C; Basu D; Datta S (2009). "Studies on a novel bioactive glass and composite coating with hydroxyapatite on titanium based alloys: Effect of γ-sterilization on coating". J Eur. Ceram. Soc. 29 (12): 2527–35. doi:10.1016/j.jeurceramsoc.2009.02.013.
- ↑ "Guidance for Industry, Sterile Drug Products Produced by Aseptic Processing — Current Good Manufacturing Practice" (PDF). U.S. Department of Health and Human Services. 2004
- ↑ "Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing" (PDF). United States Food and Drug Administration. September 2004.
Other references
- WHO - Infection Control Guidelines for Transmissible Spongiform Encephalopathies. Retrieved Jul 10, 2010
- Ninemeier J. Central Service Technical Manual (6th ed.). International Association of Healthcare Central Service Materiel Management.
- Control of microbes
- Raju GK, Cooney CL (1993). "Media and air sterilization". In Stephanopoulos G. Biotechnology, 2E, Vol. 3, Bioprocessing. Weinheim: Wiley-VCH. pp. 157–84. ISBN 3-527-28313-7.
- Innovative Technologies for the Biofunctionalisation and Terminal Sterilisation of Medical Devices
- Pharmaceutical Filtration - The Management of Organism Removal, Meltzer TH, Jornitz MW, PDA/DHI 1998
- "Association for Advancement of Medical Instrumentation ANSI/AAMI ST41-Ehylene Oxyde Sterilization in Healthcare facilities: Safety and Effectiveness. Arlington, VA: Association for Advancement of Medical Instrumentation; 2000." ISBN 1-57020-420-9
- “US Department of Labor, Occupational Safety and Health Administration.29 CFR 1910.1020. Access to Employee Medical Records.". October 26, 2007.
- Perioperative Standards and Recommended Practices, AORN 2013, ISBN 978-1-888460-77-3
|