Upper gastrointestinal series
| Upper Gastrointestinal Series | |
|---|---|
| Diagnostics | |
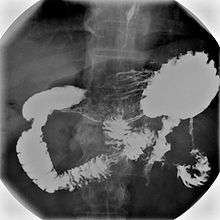
 Normal Barium swallow flouroscopic image, showing the ingested barium sulfate being induced down the oesophagus by peristalsis. | |
| ICD-10-PCS | GroupMajor.minor |
An upper gastrointestinal series, also called an upper gastrointestinal study or contrast radiography of the upper gastrointestinal tract, is a series of radiographs used to examine the gastrointestinal tract for abnormalities. A contrast medium, usually a radiocontrast agent such as barium sulfate mixed with water, is ingested or instilled into the gastrointestinal tract, and X-rays are used to create radiographs of the regions of interest. The barium enhances the visibility of the relevant parts of the gastrointestinal tract by coating the inside wall of the tract and appearing white on the film. This in combination with other plain radiographs allows for the imaging of parts of the upper gastrointestinal tract such as the pharynx, larynx, esophagus, stomach, and small intestine such that the inside wall lining, size, shape, contour, and patency are visible to the examiner. With fluoroscopy, it is also possible to visualize the functional movement of examined organs such as swallowing, peristalsis, or sphincter closure. Depending on the organs to be examined, barium radiographs can be classified into barium swallow, barium meal, barium follow-through, and enteroclysis. To further enhance the quality of images, air or gas is sometimes introduced into the gastrointestinal tract in addition to barium, and this procedure is called double-contrast imaging. In this case the gas is referred to as the negative contrast medium. Traditionally the images produced with barium contrast are made with plain-film radiography, but computed tomography is also used in combination with barium contrast, in which case the procedure is called CT enterography.[1]
Types of barium-contrast imaging


Various types of barium X-ray examinations are used to examine different parts of the gastrointestinal tract. These include barium swallow, barium meal, barium follow-through, and barium enema.[2] The barium swallow, barium meal, and barium follow-through are together also called an upper gastrointestinal series (or study), whereas the barium enema is called a lower gastrointestinal series (or study).[3] In upper gastrointestinal series examinations, the barium sulfate is mixed with water and swallowed orally, whereas in the lower gastrointestinal series (barium enema), the barium contrast agent is administered as an enema through a small tube inserted into the rectum.[2]
- Barium swallow X-ray examinations are used to study the pharynx[4] and esophagus.[2]
- Barium meal examinations are used to study the lower esophagus, stomach and duodenum.[2]
- Barium follow through examinations are used to study the small intestine.[2]
- Enteroclysis also called small bowel enema is a Barium X-ray examination used to display individual loops of the small intestine by intubating the jejunum with a small tube and administering Barium sulfate followed by methylcellulose or air.[5]
- Barium enema examinations are used to study the large intestine and rectum and are classified as lower gastrointestinal series.[2]
Medical uses
Barium X-ray examinations are a useful tools for the study of appearance and function of the parts of the gastrointestinal tract. They are used to diagnose and monitor esophageal reflux, dysphagia, hiatus hernia, strictures, diverticula, pyloric stenosis, gastritis, enteritis, volvulus, varices, ulcers, tumors, and gastrointestinal dysmotility, as well as to detect foreign bodies.[3][6] Historically barium X-ray examinations are the standard approach used to assess and diagnose diseases of the gut, but they are increasingly being replaced by more modern techniques such as computer tomography, magnetic resonance imaging, ultrasound imaging, endoscopy and capsule endoscopy.[7] However, barium contrast imaging remains a common diagnostic test, which has the advantage of lower costs and being more widely available as compared to newer techniques.[1][5] Newer techniques are also not able to assess superficial mucosal lesions in as much detail as some barium X-ray techniques such as enteroclysis.[7]
Mechanism
Barium sulfate is swallowed, which because it is a radio opaque substance does not allow the passage of X-rays. As a result, areas coated by barium sulfate will appear white on an X-ray film. The passage of barium through the gastrointestinal tract is observed by a radiologist using a fluoroscope attached to a TV monitor. The radiologist takes a series of individual X-ray images at timed intervals depending on the areas to be studied. Sometimes medication which produces gas in the gastrointestinal tract is administered together with the Barium sulfate. This gas distends the gastrointestinal lumen, providing better imaging conditions and in this case the procedure is called double-contrast imaging.[8]
Procedure
Clinical status and relevant medical history are reviewed prior to the studies.[9] Patient consent is required.[3]
Barium swallow
Little or no preparations are required for the study of the larynx, pharynx, and esophagus when studied alone.[10] A thick barium mixture is swallowed in supine position and fluoroscopic images of the swallowing process are made. Then several swallows of a thin barium mixture are taken and the passage is recorded by fluoroscopy and standard radiographs. The procedure is repeated several times with the examination table tilted at various angles. A total of 350-450 mL of barium is swallowed during the process.[11]
Barium meal and barium follow-through
For barium meal or barium follow-through examinations, a 6-hour period of fasting is observed prior to the studies.[9] Barium is administered orally, sometimes mixed with diatrizoic acid to reduce transit time in the bowel. Metoclopramide is sometimes also added to the mixture to enhance gastric emptying. X-ray images are then taken in a supine position at intervals of 20–30 minutes. Real-time fluoroscopy is used to assess bowel motility. The radiologist may press or palpate the abdomen during images to separate intestinal loops. The total time necessary for the test depends on the speed of bowel motility or transit time and may vary between 1 and 3 hours.[12]
Enteroclysis
For small bowel examinations, in addition to fasting for 8 hours prior to examination, a laxative may also be necessary for bowel preparation and cleansing.[10] Enteroclysis involves the continued infusion of 500 to 1000 mL of thin barium sulfate suspension into the intestine through a duodenal tube. Then methylcellulose is instilled through the tube. Barium and methylcellulose fill the intestinal loops which can be viewed continuously using fluoroscopy, or viewed as standard radiographs taken at frequent intervals. The technique is a double-contrast procedure that allows detailed imaging of the entire small intestine. However, the procedure may take 6 hours or longer to complete and is quite uncomfortable to undergo.[13]
Interpretation of results

- Enteroclysis has shown to be very accurate in diagnosing small bowel diseases, with a sensitivity of 93.1% and specificity of 96.9%. It permits detection of lesion which may not be seen with other imaging techniques.[7] There is no significant difference in terms of detection of clinically significant findings, sensitivity or specificity between enteroclysis and CT enterography.[1] Enteroclysis compares favorably with wireless capsule endoscopy and double-balloon endoscopy in the diagnosis of mucosal abnormalities of the small bowel.[14]
- The interpretation of standard barium swallow examinations for assessing dysphagia is operator and interpreter dependent. It has poor sensitivity for subtle abnormalities but is more sensitive in detecting esophageal webs and rings than gastroscopy.[4] The best initial evaluation of suspected oropharyngeal dysphagia is a barium study.[15] Barium swallow studies remain the main investigation of dysphagia.[16] Barium studies may detect pharyngeal tumors that are difficult to visualize endoscopically.[17]
- Barium follow through examinations are the most commonly used imaging technique in assessing patients with Crohn's disease, although CT and magnetic resonance imaging are widely accepted as being superior.[1] However Barium examinations remain superior in the depiction of mucosal abnormalities.[14] The features of Crohn's disease are well described by barium follow-through examinations, appearing as a typical "cobblestone pattern", but no information is obtained regarding extraluminal disease.[18] Radiographic imaging in Crohn's disease provides clinicians with objective evaluations of small bowel regions that are not accessible to standard endoscopic techniques.[19] Because of its length and complex loops, the small intestine is the most difficult part of the gastrointestinal tract to evaluate. Most endoscopic techniques are limited to the examination of proximal or distal segments, hence Barium follow through remains in most centres the test of choice for the investigation of abdominal pain, diarrhoea and in particular diseases manifesting mucosal abnormalities such as coeliac and Crohn's disease.[16]
- Barium swallow studies are better than endoscopy at demonstrating the anatomic findings in gastroesophageal reflux disease after anti-reflux surgery.[20]
- Barium fluoroscopic examinations have some advantages over computed tomography and magnetic resonance techniques, such as higher spatial resolution and the ability to examine bowel peristalsis and distension in real time.[21]
- Many infections and parasitic infestations produce patterns of the luminal surface, which are best seen on Barium examinations. Certain parasites are seen as filling defects outlined by Barium and Barium examinations play an important role in the diagnosis of intestinal infections and infestations as compared to other techniques.[22] Barium studies show tapeworms and roundworms as thin, linear filling defects of the bowel.[23] Because roundworms have a developed alimentary tract, barium may outline the parasites’ intestinal tracts on delayed images. In Strongyloidiasis barium studies show intestinal wall oedema, thickening of intestinal folds with flattening, and atrophy of the overlying mucosa.[23] Schistosomiasis caused by infection with flatworms have an appearance resembling colitis ulcerosa, with inflammatory polyps, ulcers, fibrosis, wall thickening, loss of haustration, and stenosis in Barium X-rays.[23] Anisakiasis is demonstrated by Barium X-rays as bowel wall oedema, thickening, ulceration, or stricture due to inflammation. Sometimes worms are seen as long, thread-like, linear filling defects up to 30 cm long.[23] In Typhlitis Barium studies show oedema, ulceration, and inflammation of bowel wall resulting in wall thickening.[23] In pseudomembranous colitis, barium studies show pancolitis with thumb printing and shaggy margins as well as plaque-like eccentric, nodular or polypoid appearance.[23]
- Barium studies and computer tomography are the most common tools used to diagnose gastrointestinal lymphoma. Barium contrast is more sensitive in the demonstration of subtle mucosa and sub-mucosa abnormalities but computer tomography is the method of choice for determining the extent of disease and staging as well as related complications such as fistulation and perforation. Submucosal nodules or masses form a bull’s-eye or target appearance on barium studies.[24]
Adverse effects
Radiographic examinations entail the exposure to radiation in form of X-rays.[18] Although barium ions are toxic, their use is generally regarded as safe because the small amounts of barium ions available in solution and absorbed by the gastrointestinal tract are deemed to be of no practical importance. However isolated cases of barium encephalopathy have been described following absorption of barium from the intestinal tract.[25] Constipation and abdominal pain may occur after Barium meals.[25] The formation of baroliths, which may need to be removed surgically, is a complication of the use of barium sulfate.[25] Barium sulfate may cause serious peritoneal irritation. Leakage of Barium sulfate into the abdominal cavity may occur in people with duodenal ulcers or other perforations and may lead to peritonitis, adhesion, and granulomas; it is associated with a high mortality rate.[10] Leakage of barium into the mediastinum or peritoneal cavity may lead to endotoxic shock which is often fatal. As a result, the use of barium as a contrast agent is contraindicated when there is a suspicion or possibility of compromise of bowel wall integrity.[25] Aspiration or inhalation of Barium sulfate into the lungs during oral application can lead to serious respiratory complications leading to fatal aspiration pneumonia or asphyxiation.[25] Hypersensitivity and allergic reactions are rare but some additives contained in Barium preparations may induce immune reactions.[25] Complete gastrointestinal obstruction is also a contraindication for barium studies.[12]
History
Barium sulfate as a contrast medium was evolved from the prior use of bismuth preparation which were too toxic. The use of bismuth preparations had been described as early as 1898. Barium sulfate as a contrast medium in medical practice was introduced largely as a result of the works of Krause a director of the Bonn Polyclinic, now the medical faculty of the University of Bonn and his colleagues Bachem and Gunther. In a paper read in 1910 at the radiological congress they advocated for the use of barium sulfate as an opaque contrast medium in medicine.[26]
References
- 1 2 3 4 Murphy, KP; McLaughlin, PD; O'Connor, OJ; Maher, MM (Mar 2014). "Imaging the small bowel.". Current opinion in gastroenterology 30 (2): 134–40. doi:10.1097/mog.0000000000000038. PMID 24419291.
- 1 2 3 4 5 6 British Medical Association (2013). BMA Illustrated Medical Dictionary. Dorling Kindersley Ltd. ISBN 1409349667.
- 1 2 3 Daniels, Rick (2010). Delmar's guide to laboratory and diagnostic tests (2nd ed.). Clifton Park, NY: Delmar/Cengage Learning. ISBN 9781418020675.
- 1 2 Kuo, P; Holloway, RH; Nguyen, NQ (May 2012). "Current and future techniques in the evaluation of dysphagia.". Journal of Gastroenterology and Hepatology 27 (5): 873–81. doi:10.1111/j.1440-1746.2012.07097.x. PMID 22369033.
- 1 2 Levine, MS; Rubesin, SE; Laufer, I (Nov 2008). "Pattern approach for diseases of mesenteric small bowel on barium studies.". Radiology 249 (2): 445–60. doi:10.1148/radiol.2491071336. PMID 18812557.
- ↑ Boland, Giles W (2013). Gastrointestinal imaging: the requisites (4th ed.). Philadelphia: Elsevier/Saunders. ISBN 9780323101998.
- 1 2 3 Markova, I; Kluchova, K; Zboril, R; Mashlan, M; Herman, M (Jun 2010). "Small bowel imaging - still a radiologic approach?". Biomedical papers of the Medical Faculty of the University Palacky, Olomouc, Czechoslovakia 154 (2): 123–32. doi:10.5507/bp.2010.019. PMID 20668493.
- ↑ M.D, Steven R. Peikin, (2014). Gastrointestinal health third edition. [S.l.]: HarperCollins e-Books. p. 29. ISBN 9780061863653.
- 1 2 al.], editors, C.J. Hawkey ... [et (2012). Textbook of Clinical Gastroenterology and Hepatology (2nd ed.). Hoboken: John Wiley & Sons. p. 1001. ISBN 9781118321409.
- 1 2 3 Nightingale, Julie; Law, Robert (2012). Gastrointestinal Tract Imaging: An Evidence-Based Practice Guide. Elsevier Health Sciences. ISBN 9780702045493.
- ↑ Chernecky, Cynthia; Berger, Barbara (2012). Laboratory Tests and Diagnostic Procedures. Elsevier Health Sciences. ISBN 9781455745029.
- 1 2 Thomas, James; Monaghan, Tanya (2014). Oxford Handbook of Clinical Examination and Practical Skills. Oxford University Press. p. 712. ISBN 9780191044540.
- ↑ al.], Rene A. Day ... [et (2009). Brunner & Suddarth's textbook of Canadian medical-surgical nursing. (2nd Canadian ed.). Philadelphia: Lippincott Williams & Wilkins. ISBN 9780781799898.
- 1 2 Maglinte, DD; Kohli, MD; Romano, S; Lappas, JC (Sep 2009). "Air (CO2) double-contrast barium enteroclysis.". Radiology 252 (3): 633–41. doi:10.1148/radiol.2523081972. PMID 19717748.
- ↑ Grant, PD; Morgan, DE; Scholz, FJ; Canon, CL (Jan–Feb 2009). "Pharyngeal dysphagia: what the radiologist needs to know.". Current problems in diagnostic radiology 38 (1): 17–32. doi:10.1067/j.cpradiol.2007.08.009. PMID 19041038.
- 1 2 Robinson, C; Punwani, S; Taylor, S (Dec 2009). "Imaging the gastrointestinal tract in 2008.". Clinical Medicine (London) 9 (6): 609–12. doi:10.7861/clinmedicine.9-6-609. PMID 20095312.
- ↑ Brant, [edited by] William E.; Helms, Clyde A. (2007). Fundamentals of diagnostic radiology (3rd ed.). Philadelphia: Lippincott, Williams & Wilkins. p. 811. ISBN 9780781761352.
- 1 2 Dambha, F; Tanner, J; Carroll, N (Jun 2014). "Diagnostic imaging in Crohn's disease: what is the new gold standard?". Best practice & research. Clinical gastroenterology 28 (3): 421–36. doi:10.1016/j.bpg.2014.04.010. PMID 24913382.
- ↑ Deepak, P; Bruining, DH (Aug 2014). "Radiographical evaluation of ulcerative colitis.". Gastroenterology report 2 (3): 169–77. doi:10.1093/gastro/gou026. PMID 24843072.
- ↑ Baker, ME; Einstein, DM (Mar 2014). "Barium esophagram: does it have a role in gastroesophageal reflux disease?". Gastroenterology clinics of North America 43 (1): 47–68. doi:10.1016/j.gtc.2013.11.008. PMID 24503359.
- ↑ Fidler, JL; Fletcher, JG; Bruining, DH; Trenkner, SW (Jul 2013). "Current status of CT, magnetic resonance, and barium in inflammatory bowel disease.". Seminars in roentgenology 48 (3): 234–44. doi:10.1053/j.ro.2013.03.004. PMID 23796374.
- ↑ Sinha, R; Rajesh, A; Rawat, S; Rajiah, P; Ramachandran, I (May 2012). "Infections and infestations of the gastrointestinal tract. Part 1: bacterial, viral and fungal infections.". Clinical radiology 67 (5): 484–94. doi:10.1016/j.crad.2011.10.021. PMID 22257535.
- 1 2 3 4 5 6 Sinha, R; Rajesh, A; Rawat, S; Rajiah, P; Ramachandran, I (May 2012). "Infections and infestations of the gastrointestinal tract. Part 2: parasitic and other infections.". Clinical radiology 67 (5): 495–504. doi:10.1016/j.crad.2011.10.022. PMID 22169349.
- ↑ Engin, G; Korman, U (Sep 2011). "Gastrointestinal lymphoma: a spectrum of fluoroscopic and CT findings.". Diagnostic and interventional radiology (Ankara, Turkey) 17 (3): 255–65. doi:10.4261/1305-3825.dir.3332-10.3. PMID 20725903.
- 1 2 3 4 5 6 Baert, Henrik S. Thomsen ; Judith A.W. Webb (ed.). With contributions by P. Aspelin ... Foreword by A.L. (2009). Contrast media : safety issues and ESUR guidelines ; with 24 tables (2., rev. ed.). Berlin: Springer. ISBN 9783540727835.
- ↑ Schott, G. D. (16 August 2012). "SOME OBSERVATIONS ON THE HISTORY OF THE USE OF BARIUM SALTS IN MEDICINE". Medical History 18 (1): 9–21. doi:10.1017/S0025727300019190. PMC 1081520. PMID 4618587.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||