Severe acute respiratory syndrome
| Severe Acute Respiratory Syndrome (SARS) | |
|---|---|
 SARS coronavirus (SARS-CoV) is causative of the syndrome. | |
| Classification and external resources | |
| Specialty | Infectious disease |
| ICD-10 | U04 |
| ICD-9-CM | 079.82 |
| DiseasesDB | 32835 |
| MedlinePlus | 007192 |
| eMedicine | med/3662 |
| Patient UK | Severe acute respiratory syndrome |
| MeSH | D045169 |
Severe acute respiratory syndrome (SARS) is a viral respiratory disease of zoonotic origin caused by the SARS coronavirus (SARS-CoV). Between November 2002 and July 2003, an outbreak of SARS in southern China caused an eventual 8,096 cases and 774 deaths reported in multiple countries with the majority of cases in Hong Kong[1] (9.6% fatality rate) according to the World Health Organization (WHO).[1] Within weeks, SARS spread from Hong Kong to infect individuals in 37 countries in early 2003.[2] It then was eradicated by January the following year.[3]
Signs and symptoms
Initial symptoms are flu-like and may include fever, myalgia, lethargy symptoms, cough, sore throat, and other nonspecific symptoms. The only symptom common to all patients appears to be a fever above 38 °C (100 °F). Shortness of breath may occur later. The patient has symptoms as with a cold in the first stage, but later on they resemble influenza. SARS may occasionally lead to pneumonia, either direct viral pneumonia or secondary bacterial pneumonia.
Diagnosis

SARS may be suspected in a patient who has:
- Any of the symptoms, including a fever of 38 °C (100 °F) or higher, and
- Either a history of:
- Contact (sexual or casual, including tattoos) with someone with a diagnosis of SARS within the last 10 days OR
- Travel to any of the regions identified by the World Health Organization (WHO) as areas with recent local transmission of SARS (affected regions as of 10 May 2003 were parts of China, Hong Kong, Singapore and the town of Geraldton, Ontario, Canada).
A probable case of SARS has the above findings plus positive chest X-ray findings of atypical pneumonia or respiratory distress syndrome.
The World Health Organization (WHO) has added the category of "laboratory confirmed SARS" for patients who would otherwise fit the above "probable" category who do not (yet) have the chest X-ray changes, but do have positive laboratory diagnosis of SARS based on one of the approved tests (ELISA, immunofluorescence or PCR).[4]
The chest X-ray (CXR) appearance of SARS is variable. There is no pathognomonic appearance of SARS, but is commonly felt to be abnormal with patchy infiltrates in any part of the lungs. The initial CXR may be clear.[5]
Treatment
Antibiotics are ineffective, as SARS is a viral disease. Treatment of SARS is largely supportive with antipyretics, supplemental oxygen and mechanical ventilation as needed.
Suspected cases of SARS must be isolated, preferably in negative pressure rooms, with complete barrier nursing precautions taken for any necessary contact with these patients.
Some of the more serious damage in SARS may be due to the body's own immune system reacting in what is known as cytokine storm.[6]
As of 2015, there is no cure or protective vaccine for SARS that is safe for use in humans.[7] The identification and development of novel vaccines and medicines to treat SARS is a priority for governments and public health agencies around the world. MassBiologics, a non-profit organization engaged in the discovery, development and manufacturing of biologic therapies, is cooperating with researchers at NIH and the CDC developed a monoclonal antibody therapy that demonstrated efficacy in animal models.[8][9][10]
Prognosis
Several consequent reports from China on some recovered SARS patients showed severe long-time sequelae exist. The most typical diseases include, among other things, pulmonary fibrosis, osteoporosis, and femoral necrosis, which have led to the complete loss of working ability or even self-care ability of these cases. As a result, some of the post-SARS patients suffer from major depressive disorder.[11]
Prevention
There is no vaccine to date. Isolation and quarantine remain the most effective means to prevent the spread of SARS. In addition, handwashing, use of universal precautions, disinfection of surfaces for fomites, and use of a surgical mask are recommended. Avoid contact with bodily fluids. Continue with precautions for at least 10 days after the person's signs and symptoms have disappeared. Keep children home from school if they develop a fever or respiratory symptoms within 10 days of being exposed to someone with SARS. Wash personal items in hot, soapy water including the eating utensils and dishes, bedding and clothing of someone with SARS.[12] Annual influenza vaccinations and 5-year pneumococcal vaccinations may be beneficial; but vaccinations only reduce or weaken the severity of SARS infection.
Epidemiology
SARS was a relatively rare disease, with 8,273 cases as of 2003.[13]
History
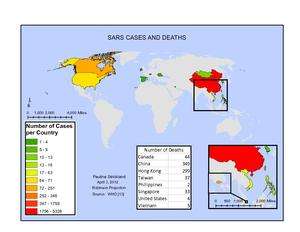
| Probable cases of SARS by country, 1 November 2002 – 31 July 2003. | ||||
| Country or Region | Cases | Deaths | SARS cases dead due to other causes | Fatality (%) |
| Canada | 251 | 44 | 0 | 18 |
| China (Mainland) * | 5,328 | 349 | 19 | 6.6 |
| China (Hong Kong) * | 1,755 | 299 | 5 | 17 |
| China (Macau) * | 1 | 0 | 0 | 0 |
| Taiwan ** | 346 | 37 | 36 | 11 |
| Singapore | 238 | 33 | 0 | 14 |
| Vietnam | 63 | 5 | 0 | 8 |
| United States | 27 | 0 | 0 | 0 |
| Philippines | 14 | 2 | 0 | 14 |
| Mongolia | 9 | 0 | 0 | 0 |
| Kuwait | 1 | 0 | 0 | 0 |
| Republic of Ireland | 1 | 0 | 0 | 0 |
| Romania | 1 | 0 | 0 | 0 |
| Russian Federation | 1 | 0 | 0 | 0 |
| Spain | 1 | 0 | 0 | 0 |
| Switzerland | 1 | 0 | 0 | 0 |
| South Korea | 4 | 0 | 0 | 0 |
| Total | 8273 | 775 | 60 | 9.6 |
| (*) Figures for the People's Republic of China exclude the Special Administrative Regions (Macau SAR, Hong Kong SAR), which are reported separately by the WHO. | ||||
| (**) Since 11 July 2003, 325 Taiwanese cases have been 'discarded'. Laboratory information was insufficient or incomplete for 135 discarded cases; 101 of these patients died. | ||||
| Source:WHO.[14] | ||||
Outbreak in South China
The epidemic of SARS appears to have started in Guangdong Province, China in November 2002. The first reported case of SARS originated in Shunde, Foshan, Guangdong in November 2002, and the patient, a farmer, was treated in the First People's Hospital of Foshan (Mckay Dennis). The patient died soon after, and no definite diagnosis was made on his cause of death. Despite taking some action to control it, Chinese government officials did not inform the World Health Organization of the outbreak until February 2003. This lack of openness caused delays in efforts to control the epidemic, resulting in criticism of the People's Republic of China from the international community. China has since officially apologized for early slowness in dealing with the SARS epidemic.[15]
The first clue of the outbreak appears to be 27 November 2002 when Canada's Global Public Health Intelligence Network (GPHIN), an electronic warning system that is part of the World Health Organization's Global Outbreak and Alert Response Network (GOARN), picked up reports of a "flu outbreak" in China through Internet media monitoring and analysis and sent them to the WHO. Importantly, while GPHIN's capability had recently been upgraded to enable Arabic, Chinese, English, French, Russian, and Spanish translation, the system was limited to English or French in presenting this information. Thus, while the first reports of an unusual outbreak were in Chinese, an English report was not generated until 21 January 2003.[16][16][17]
Subsequent to this, the WHO requested information from Chinese authorities on 5 and 11 December. Despite the successes of the network in previous outbreak of diseases, it was proven rather defective after receiving intelligence on the media reports from China several months after the outbreak of SARS. Along with the second alert, WHO released the name, definition, as well as an activation of a coordinated global outbreak response network that brought sensitive attention and containment procedures (Heymann, 2003). However, by then although the new definitions do give nations a guideline to contain SARS, over 500 deaths and an additional 2,000 cases had already occurred worldwide.[17]
In early April, after Jiang Yanyong pushed to report the danger to China,[18][19] there appeared to be a change in official policy when SARS began to receive a much greater prominence in the official media. Some have directly attributed this to the death of American James Earl Salisbury.[20] However, also in early April, accusations by Jiang Yanyong emerged regarding the undercounting of cases in Beijing military hospitals.[18][19] After intense pressure, Chinese officials allowed international officials to investigate the situation there. This revealed problems plaguing the aging mainland Chinese healthcare system, including increasing decentralization, red tape, and inadequate communication.
Many doctors and other medical staff in many nations heroically risked their lives treating patients and containing the infection before ways to prevent infection were known. Not all survived.[21]
Spread to other countries and regions
The epidemic reached the public spotlight in February 2003, when an American businessman traveling from China became afflicted with pneumonia-like symptoms while on a flight to Singapore. The plane stopped at Hanoi, Vietnam, where the victim died in The French Hospital of Hanoi. Several of the medical staff who treated him soon developed the same disease despite basic hospital procedures. Italian doctor Carlo Urbani identified the threat and communicated it to WHO and the Vietnamese government; he later succumbed to the disease.
The severity of the symptoms and the infection of hospital staff alarmed global health authorities fearful of another emergent pneumonia epidemic. On 12 March 2003, the WHO issued a global alert, followed by a health alert by the United States Centers for Disease Control and Prevention (CDC). Local transmission of SARS took place in Toronto, Ottawa, San Francisco, Ulaanbaatar, Manila, Singapore, Taiwan, Hanoi and Hong Kong whereas within China it spread to Guangdong, Jilin, Hebei, Hubei, Shaanxi, Jiangsu, Shanxi, Tianjin, and Inner Mongolia.

In Hong Kong, the first cohort of affected people were discharged from the hospital on 29 March 2003. The disease spread in Hong Kong from a mainland doctor who arrived in February and stayed at the ninth floor of the Metropole Hotel in Kowloon, infecting 16 of the hotel visitors. Those visitors traveled to Canada, Singapore, Taiwan, and Vietnam, spreading SARS to those locations.[22]
Another larger cluster of cases in Hong Kong centred on the Amoy Gardens housing estate. Its spread is suspected to have been facilitated by defects in its drainage system. Concerned citizens in Hong Kong worried that information was not reaching people quickly enough and created a website called sosick.org, which eventually forced the Hong Kong government to provide information related to SARS in a timely manner.
Identification of virus
The CDC and Canada's National Microbiology Laboratory identified the SARS genome in April, 2003.[23][24] Scientists at Erasmus University in Rotterdam, the Netherlands demonstrated that the SARS coronavirus fulfilled Koch's postulates thereby confirming it as the causative agent. In the experiments, macaques infected with the virus developed the same symptoms as human SARS victims.[25]
In late May 2003, studies from samples of wild animals sold as food in the local market in Guangdong, China, found the SARS coronavirus could be isolated from masked palm civets (Paguma sp.), but the animals did not always show clinical signs. The preliminary conclusion was the SARS virus crossed the xenographic barrier from palm civet to humans, and more than 10,000 masked palm civets were killed in Guangdong Province. Virus was also later found in raccoon dogs (Nyctereuteus sp.), ferret badgers (Melogale spp.), and domestic cats. In 2005, two studies identified a number of SARS-like coronaviruses in Chinese bats.[26][27] Phylogenetic analysis of these viruses indicated a high probability that SARS coronavirus originated in bats and spread to humans either directly or through animals held in Chinese markets. The bats did not show any visible signs of disease, but are the likely natural reservoirs of SARS-like coronaviruses. In late 2006, scientists from the Chinese Centre for Disease Control and Prevention of Hong Kong University and the Guangzhou Centre for Disease Control and Prevention established a genetic link between the SARS coronavirus appearing in civets and humans, bearing out claims that the disease had jumped across species.[28]
Containment
The World Health Organization declared severe acute respiratory syndrome contained on 9 July 2003. In the year after, SARS made the occasional appearance. There were four cases spotted in China in December 2003 and January 2004. As well, three separate laboratory accidents resulted in infections; in one case, an ill lab worker spread the virus to several other people.[3][29] The precise coronavirus that caused SARS is gone or mostly contained within different BSL-4 laboratories for research much like Smallpox, but different coronaviruses remain circulating in the wild, like MERS, the Common Cold and gastroenteritis.
See also
- 2009 flu pandemic
- Bird flu
- MERS-CoV – Coronavirus discovered in June 2012 in Saudi Arabia
- Health crisis
- Jiang Yanyong
- Public health in the People's Republic of China
- SARS conspiracy theory
- Super-spreader
- Progress of the SARS outbreak
- Bat-borne virus
References
- 1 2 "Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003". World Health Organization (WHO). Retrieved 2008-10-31.
- ↑ Smith, R. D. (2006). "Responding to global infectious disease outbreaks, Lessons from SARS on the role of risk perception, communication and management". Social Science and Medicine 63 (12): 3113–3123. doi:10.1016/j.socscimed.2006.08.004. PMID 16978751.
- 1 2 http://www.huffingtonpost.ca/2013/03/11/sars-2013_n_2854568.html
- ↑ "Laboratory Diagnosis of SARS". Emerging Infectious Disease Journal (Centers for Disease Control and Prevention) 10 (5). May 2004. Retrieved 2013-07-14.
- ↑ Lu P, Zhou B, Chen X, Yuan M, Gong X, Yang G, Liu J, Yuan B, Zheng G, Yang G, Wang H. (July 2003). "Chest X-ray imaging of patients with SARS". Chinese Medical Journal 116 (7): 972–5. PMID 12890364.
- ↑ Dandekar, A; Perlman, S (2005). "Immunopathogenesis of coronavirus infections: implications for SARS". Nat Rev Immunol 5 (12): 917–927. doi:10.1038/nri1732. PMID 16322745.
- ↑ Shibo Jiang, Lu Lu & Lanying Du (2013). "Development of SARS vaccines and therapeutics is still needed". Future Virology 8 (1): 1–2. doi:10.2217/fvl.12.126.
- ↑ Greenough TC, Babcock GJ, Roberts A, Hernandez HJ, Thomas WD Jr, Coccia JA, Graziano RF, Srinivasan M, Lowy I, Finberg RW, Subbarao K, Vogel L, Somasundaran M, Luzuriaga K, Sullivan JL, Ambrosino DM (15 February 2005). "Development and characterization of a severe acute respiratory syndrome-associated coronavirus-neutralizing human monoclonal antibody that provides effective immunoprophylaxis in mice". The Journal of Infectious Diseases 191 (4): 507–14. doi:10.1086/427242. PMID 15655773.
- ↑ Tripp RA, Haynes LM, Moore D, Anderson B, Tamin A, Harcourt BH, Jones LP, Yilla M, Babcock GJ, Greenough T, Ambrosino DM, Alvarez R, Callaway J, Cavitt S, Kamrud K, Alterson H, Smith J, Harcourt JL, Miao C, Razdan R, Comer JA, Rollin PE, Ksiazek TG, Sanchez A, Rota PA, Bellini WJ, Anderson LJ (September 2005). "Monoclonal antibodies to SARS-associated coronavirus (SARS-CoV): identification of neutralizing and antibodies reactive to S, N, M and E viral proteins". J Virol Methods 128 (1–2): 21–8. doi:10.1016/j.jviromet.2005.03.021. PMID 15885812.
- ↑ Roberts A, Thomas WD, Guarner J, Lamirande EW, Babcock GJ, Greenough TC, Vogel L, Hayes N, Sullivan JL, Zaki S, Subbarao K, Ambrosino DM (1 March 2006). "Therapy with a severe acute respiratory syndrome-associated coronavirus-neutralizing human monoclonal antibody reduces disease severity and viral burden in golden Syrian hamsters". J Infect Dis 193 (5): 685–92. doi:10.1086/500143. PMID 16453264.
- ↑ Ma Jinyu (2009-07-15). "(Silence of the Post-SARS Patients)" (in Chinese). Southern People Weekly. Retrieved 2013-08-03.
- ↑ "SARS: Prevention". MayoClinic.com. 2011-01-06. Retrieved 2013-07-14.
- ↑ Oehler, Richard L. "Severe Acute Respiratory Syndrome (SARS)". Retrieved 2008-05-11.
- ↑ "Epidemic and Pandemic Alert and Response (EPR)". World Health Organization.
- ↑ "WHO targets SARS 'super spreaders'". CNN. 6 April 2003. Retrieved 5 July 2006.
- 1 2 Mawudeku, Abla; Blench, Michael (2005). "Global Public Health Intelligence Network" (PDF). Public Health Agency of Canada.
- 1 2 Rodier, G (10 February 2004). "Global Surveillance, National Surveillance, and SARS". Emerging Infectious Diseases 10: 173–5. doi:10.3201/eid1002.031038. PMID 15040346.
- 1 2 Joseph Kahn (12 July 2007). "China bars U.S. trip for doctor who exposed SARS cover-up". The New York Times. Retrieved 2013-08-03.
- 1 2 "The 2004 Ramon Magsaysay Awardee for Public Service". Ramon Magsaysay Foundation. 31 August 2004. Retrieved 2013-05-03.
- ↑ "SARS death leads to China dispute". CNN. 10 April 2003. Retrieved 3 April 2007.
- ↑ Sars: The people who risked their lives to stop the virus
- ↑ "Sr. Irene Martineau". Oxford Medical School Gazette. Retrieved 2008-11-10.
- ↑ "Remembering SARS: A Deadly Puzzle and the Efforts to Solve It". Centers for Disease Control and Prevention. 11 April 2013. Retrieved 3 August 2013.
- ↑ "Coronavirus never before seen in humans is the cause of SARS". United Nations World Health Organization. 16 April 2006. Retrieved 5 July 2006.
- ↑ Fouchier RA, Kuiken T, Schutten M, et al. (2003). "Aetiology: Koch's postulates fulfilled for SARS virus". Nature 423 (6937): 240. doi:10.1038/423240a. PMID 12748632.
- ↑ Li W, Shi Z, Yu M, et al. (2005). "Bats are natural reservoirs of SARS-like coronaviruses". Science 310 (5748): 676–9. doi:10.1126/science.1118391. PMID 16195424.
- ↑ Lau SK, Woo PC, Li KS, et al. (2005). "Severe acute respiratory syndrome coronavirus-like virus in Chinese horseshoe bats". Proc. Natl. Acad. Sci. U.S.A. 102 (39): 14040–5. doi:10.1073/pnas.0506735102. PMC 1236580. PMID 16169905.
- ↑ "Scientists prove SARS-civet cat link". China Daily. 23 November 2006.
- ↑ "WHO | SARS outbreak contained worldwide". www.who.int. Retrieved 2015-10-16.
Further reading
- Alan DL Sihoe; Randolph HL Wong; Alex TH Lee; Lee Sung Lau; Natalie Y. Y. Leung; Kin Ip Law; Anthony P. C. Yim (June 2004). "Severe acute respiratory syndrome complicated by spontaneous pneumothorax". Chest 125 (6): 2345–51. doi:10.1378/chest.125.6.2345. PMID 15189961.
- War Stories, Martin Enserink, Science 15 March 2013: 1264–1268. In 2003, the world successfully fought off a new disease that could have become a global catastrophe. A decade after the SARS outbreak, how much safer are we?
- SARS: Chronology of the Epidemic Martin Enserink, Science 15 March 2013: 1266–1271. In 2003, the world successfully fought off a new disease that could have become a global catastrophe. Here's what happened from the first case to the end of the epidemic.
- Understanding the Enemy, Dennis Normile, Science 15 March 2013: 1269–1273. Research sparked by the SARS outbreak increased the understanding of emerging diseases, though much remains to be learned.
External links
| Library resources about Severe acute respiratory syndrome |
| Wikimedia Commons has media related to SARS. |
- Vaccine Research Center Information regarding preventative vaccine research studies
- MedlinePlus: Severe Acute Respiratory Syndrome News, links and information from The United States National Library of Medicine.
- Severe Acute Respiratory Syndrome (SARS) Symptoms and treatment guidelines, travel advisory, and daily outbreak updates. From the World Health Organization (WHO).
- Severe Acute Respiratory Syndrome (SARS) Information on the international outbreak of the illness known as severe acute respiratory syndrome (SARS). Provided by the US Centers for Disease Control
- Severe Acute Respiratory Syndrome (SARS) Information on Severe Acute Respiratory Syndrome (SARS) – For Health Professionals from the Public Health Agency of Canada.
- Life in Hong Kong during SARS – a gallery of images reflecting daily life in Hong Kong during the 2003 SARS outbreak.
- What we can learn from SARS Severe Acute Respiratory Syndrome (SARS)—Lessons for Future Pandemics
- Virus Pathogen Database and Analysis Resource (ViPR): Coronaviridae
- Other
- NIOSH Topic Area: Severe Acute Respiratory Syndrome (SARS)
- NIOSH Publication: Understanding Respiratory Protection Against SARS
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||
|