Scabies
| Scabies | |
|---|---|
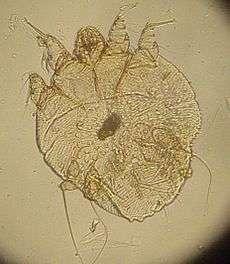 A photomicrograph of an itch mite (Sarcoptes scabiei) | |
| Classification and external resources | |
| Specialty | Infectious disease, dermatology |
| ICD-10 | B86 |
| ICD-9-CM | 133.0 |
| DiseasesDB | 11841 |
| MedlinePlus | 000830 |
| eMedicine | derm/382 emerg/517 ped/2047 |
| Patient UK | Scabies |
| MeSH | D012532 |
Scabies, known as the seven-year itch, is a contagious skin infestation by the mite Sarcoptes scabiei.[1][2] The most common symptoms are severe itchiness and a pimple-like rash. Occasionally tiny burrows may be seen in the skin. When first infected, usually two to six weeks are required before symptoms occur. If a person develops a second infection later in life, symptoms may begin within a day. These symptoms can be present across most of the body or just certain areas such as the wrists, between fingers, or along the waistline. The head may be affected, however this is typically only in young children, and not in older children or adults. The itch is often worse at night. Scratching may cause skin breakdown and an additional bacterial infection of the skin.[3]
Scabies is caused by infection with the female mite Sarcoptes scabiei.[1] The mites burrow into the skin to live and deposit eggs.[1] The symptoms of scabies are due to an allergic reaction to the mites.[3] Often only between ten and fifteen mites are involved in an infection.[3] Scabies is most often spread during a relatively long period of direct skin contact with an infected person such as that which may occur during sex.[1] Spreads of disease may occur even if the person has not developed symptoms yet.[4] Crowded living conditions such as those found in child care facilities, group homes, and prisons increase the risk of spread.[1] Areas with a lack of access to water also have higher rates of disease.[5] Crusted scabies is a more severe form of the disease. It typically only occurs in those with a poor immune system and people may have millions of mites, making them much more contagious. In these cases spread of infection may occur during brief contact or via contaminated objects. The mite is very small and usually not directly visible. Diagnosis is based on the signs and symptoms.[6]
A number of medications are available to treat those infected, including permethrin, crotamiton and lindane creams and ivermectin pills.[7] Sexual contacts within the last month and people who live in the same house should also be treated at the same time. Bedding and clothing used in the last three days should be washed in hot water and dried in a hot dryer. As the mite does not live for more than three days away from human skin more washing is not needed. Symptoms may continue for two to four weeks following treatment. If after this time there continues to be symptoms retreatment may be needed.[4]
Scabies is one of the three most common skin disorders in children, along with ringworm and bacterial skin infections.[8] As of 2010 it affects approximately 100 million people (1.5% of the world population) and is equally common in both sexes.[9] The young and the old are more commonly affected. It also occurs more commonly in the developing world and tropical climates.[6] The word scabies is from Latin: scabere, "to scratch".[10] Other animals do not spread human scabies.[1] Infections in other animals are typically caused by slightly different but related mites and is known as sarcoptic mange.[11]
Signs and symptoms
The characteristic symptoms of a scabies infection include intense itching and superficial burrows.[12] The burrow tracks are often linear, to the point that a neat "line" of four or more closely placed and equally developed mosquito-like "bites" is almost diagnostic of the disease. Because the host develops the symptoms as a reaction to the mites' presence over time, there is typically a delay of four to six weeks between the onset of infestation and the onset of itching. Similarly, symptoms often persist for one to several weeks after successful eradication of the mites. As noted, those re-exposed to scabies after successful treatment may exhibit symptoms of the new infestation in a much shorter period—as little as one to four days.[13]
Itching
In the classic scenario, the itch is made worse by warmth, and is usually experienced as being worse at night, possibly because there are fewer distractions.[12] As a symptom, it is less common in the elderly.[12]
Rash

The superficial burrows of scabies usually occur in the area of the finger webs, feet, ventral wrists, elbows, back, buttocks, and external genitals.[12] Except in infants and the immunosuppressed, infection generally does not occur in the skin of the face or scalp. The burrows are created by excavation of the adult mite in the epidermis.[12]
In most people, the trails of the burrowing mites are linear or s-shaped tracks in the skin often accompanied by rows of small, pimple-like mosquito or insect bites. These signs are often found in crevices of the body, such as on the webs of fingers and toes, around the genital area, in stomach folds of the skin, and under the breasts of women.[15]
Symptoms typically appear two to six weeks after infestation for individuals never before exposed to scabies. For those having been previously exposed, the symptoms can appear within several days after infestation. However, it is not unknown for symptoms to appear after several months or years.[16] Acropustulosis, or blisters and pustules on the palms and soles of the feet, are characteristic symptoms of scabies in infants.[15]
-

Scabies of the foot
-

Scabies of the arm
-

Scabies of the hand
-

Scabies of the finger
Crusted scabies

The elderly and people with an impaired immune system, such as HIV, cancer, or those on immunosuppressive medications, are susceptible to crusted scabies (formerly called Norwegian scabies).[12][16][17] On those with weaker immune systems, the host becomes a more fertile breeding ground for the mites, which spread over the host's body, except the face. Sufferers of crusted scabies exhibit scaly rashes, slight itching, and thick crusts of skin that contain thousands of mites.[18] Such areas make eradication of mites particularly difficult, as the crusts protect the mites from topical miticides/scabicides, necessitating prolonged treatment of these areas.
Cause
Scabies mite


In the 18th century, Italian biologist Diacinto Cestoni (1637–1718) described the mite now called Sarcoptes scabiei, variety hominis, as the cause of scabies. Sarcoptes is a genus of skin parasites and part of the larger family of mites collectively known as scab mites. These organisms have eight legs as adults, and are placed in the same phylogenetic class (Arachnida) as spiders and ticks.
Sarcoptes scabiei mites are under 0.5 mm in size but are sometimes visible as pinpoints of white. Pregnant females tunnel into the dead, outermost layer (stratum corneum) of a host's skin and deposit eggs in the shallow burrows. The eggs hatch into larvae in three to ten days. These young mites move about on the skin and molt into a "nymphal" stage, before maturing as adults, which live three to four weeks in the host's skin. Males roam on top of the skin, occasionally burrowing into the skin. In general, the total number of adult mites infesting a healthy hygienic person with non-crusted scabies is small; about 11 females in burrows, on average.[19]
The movement of mites within and on the skin produces an intense itch, which has the characteristics of a delayed cell-mediated inflammatory response to allergens. IgE antibodies are present in the serum and the site of infection, which react to multiple protein allergens in the body of the mite. Some of these cross-react to allergens from house-dust mites. Immediate antibody-mediated allergic reactions (wheals) have been elicited in infected persons, but not in healthy persons; immediate hypersensitivity of this type is thought to explain the observed far more rapid allergic skin response to reinfection seen in persons having been previously infected (especially having been infected within the previous year or two).[20]
Transmission
Scabies is contagious and can be contracted through prolonged (as opposed to momentary) physical contact with an infested person.[21] This includes sexual intercourse, although a majority of cases are acquired through other forms of skin-to-skin contact. Less commonly, scabies infestation can happen through the sharing of clothes, towels, and bedding, but this is not a major mode of transmission; individual mites can only survive for two to three days, at most, away from human skin.[22][23] As with lice, a latex condom is ineffective against scabies transmission during intercourse, because mites typically migrate from one individual to the next at sites other than the sex organs.[24]
Healthcare workers are at risk of contracting scabies from patients, because they may be in extended contact with them.[25]
Pathophysiology
The symptoms are caused by an allergic reaction of the host's body to mite proteins, though exactly which proteins remains a topic of study. The mite proteins are also present from the gut, in mite feces, which are deposited under the skin. The allergic reaction is both of the delayed (cell-mediated) and immediate (antibody-mediated) type, and involves IgE (antibodies, it is presumed, mediate the very rapid symptoms on reinfection).[19] The allergy-type symptoms (itching) continue for some days, and even several weeks, after all mites are killed. New lesions may appear for a few days after mites are eradicated. Nodular lesions from scabies may continue to be symptomatic for weeks after the mites have been killed.[19]
Diagnosis

Scabies may be diagnosed clinically in geographical areas where it is common when diffuse itching presents along with either lesions in two typical spots or there is itchiness of another household member.[8] The classical sign of scabies is the burrows made by the mites within the skin.[8] To detect the burrow, the suspected area is rubbed with ink from a fountain pen or a topical tetracycline solution, which glows under a special light. The skin is then wiped with an alcohol pad. If the person is infected with scabies, the characteristic zigzag or S pattern of the burrow will appear across the skin; however, interpreting this test may be difficult, as the burrows are scarce and may be obscured by scratch marks.[8] A definitive diagnosis is made by finding either the scabies mites or their eggs and fecal pellets.[8] Searches for these signs involve either scraping a suspected area, mounting the sample in potassium hydroxide and examining it under a microscope, or using dermoscopy to examine the skin directly.[12]
Differential diagnosis
Symptoms of early scabies infestation mirror other skin diseases, including dermatitis, syphilis, erythema multiforme, various urticaria-related syndromes, allergic reactions, and other ectoparasites such as lice and fleas.[26]
Prevention
Mass treatment programs that use topical permethrin or oral ivermectin have been effective in reducing the prevalence of scabies in a number of populations.[8] No vaccine is available for scabies. The simultaneous treatment of all close contacts is recommended, even if they show no symptoms of infection (asymptomatic), to reduce rates of recurrence.[8][8] Since mites can survive for only two to three days without a host, other objects in the environment pose little risk of transmission except in the case of crusted scabies, thus cleaning is of little importance.[8] Rooms used by those with crusted scabies require thorough cleaning.[27]
Management
A number of medications are effective in treating scabies. Treatment should involve the entire household, and any others who have had recent, prolonged contact with the infested individual.[8] Options to control itchiness include antihistamines and prescription anti-inflammatory agents.[28] Bedding, clothing and towels used during the previous three days should be washed in hot water and dried in a hot dryer.[29]
Permethrin
Permethrin is the most effective treatment for scabies,[30] and remains the treatment of choice.[8][31] It is applied from the neck down, usually before bedtime, and left on for about eight to 14 hours, then washed off in the morning.[8] Care should be taken to coat the entire skin surface, not just symptomatic areas; any patch of skin left untreated can provide a "safe haven" for one or more mites to survive. One application is normally sufficient, as permethrin kills eggs and hatchlings as well as adult mites, though many physicians recommend a second application three to seven days later as a precaution. Crusted scabies may require multiple applications, or supplemental treatment with oral ivermectin (below).[8][31][32] Permethrin may cause slight irritation of the skin that is usually tolerable.[12]
Ivermectin
Oral Ivermectin is effective in eradicating scabies, often in a single dose.[5][8] It is the treatment of choice for crusted scabies, and is sometimes prescribed in combination with a topical agent.[8][12] It has not been tested on infants, and is not recommended for children under six years of age.[12]
Topical ivermectin preparations have been shown to be effective for scabies in adults, though only one such formulation is available in the United States at present, and it is not FDA approved as a scabies treatment.[33] It has also been useful for sarcoptic mange (the veterinary analog of human scabies).[34]
Others
Other treatments include lindane, benzyl benzoate, crotamiton, malathion, and sulfur preparations.[8][12] Lindane is effective, but concerns over potential neurotoxicity has limited its availability in many countries.[12] It is banned in California,[35] but may be used in other states as a second-line treatment.[36] Sulfur ointments or benzyl benzoate are often used in the developing world due to their low cost;[12] 10% sulfur solutions have been shown to be effective,[37] and sulfur ointments are typically used for at least a week, though many people find the odor of sulfur products unpleasant.[12] Crotamiton has been found to be less effective than permethrin in limited studies.[12] Crotamiton or sulfur preparations are sometimes recommended instead of permethrin for children, due to concerns over dermal absorption of permethrin.[8]
-

Day 4
-
Day 8 (treatment begins)
-
Day 12 (under treatment)
-
Healed
Communities
Anne Frank was infected with scabies at Auschwitz concentration camp,[38] and scabies is endemic in many developing countries,[39] where it tends to be particularly problematic in rural and remote areas. In such settings community wide control strategies are required to reduce the rate of disease, as treatment of only individuals is ineffective due to the high rate of reinfection. Large-scale mass drug administration strategies may be required where coordinated interventions aim to treat whole communities in one concerted effort.[40] Although such strategies have shown to be able to reduce the burden of scabies in these kinds of communities, debate remains about the best strategy to adopt, including the choice of drug.[40][41]
The resources required to implement such large-scale interventions in a cost-effective and sustainable way are significant. Furthermore, since endemic scabies is largely restricted to poor and remote areas, it is a public health issue that has not attracted much attention from policy makers and international donors.[40][41]
Epidemiology
Scabies is one of the three most common skin disorders in children, along with tinea and pyoderma.[8] As of 2010 it affects approximately 100 million people (1.5% of the population) and is equally common in both genders.[9] The mites are distributed around the world and equally infect all ages, races, and socioeconomic classes in different climates.[18] Scabies is more often seen in crowded areas with unhygienic living conditions.[42] Globally as of 2009, an estimated 300 million cases of scabies occur each year, although various parties claim the figure is either over- or underestimated.[16][43] About 1–10% of the global population is estimated to be infected with scabies, but in certain populations, the infection rate may be as high as 50–80%.[8]
History

Scabies has been observed in humans since ancient times. Archeological evidence from Egypt and the Middle East suggests scabies was present as early as 494 BC.[13][44] The first recorded reference to scabies is believed to be from the Bible – it may be a type of "leprosy" mentioned in Leviticus circa 1200 BC[45] or be mentioned among the curses of Deuteronomy 28.[46] In the fourth century BC, Aristotle reported on "lice" that "escape from little pimples if they are pricked" — a description consistent with scabies.[47]
The Greek encyclopedist and medical writer Aulus Cornelius Celsus (c. 25 BC – c. 50 AD) is credited with naming the disease "scabies" and describing its characteristic features.[47] The parasitic etiology of scabies was documented by the Italian physician Giovanni Cosimo Bonomo (1663–1696) in his 1687 letter, "Observations concerning the fleshworms of the human body".[47] Bonomo's description established scabies as one of the first human diseases with a well-understood cause.[13][44]
Society and culture
The International Alliance for the Control of Scabies (IACS) was started in 2012,[41][48][49] and brings together over 70 researchers, clinicians and public health experts from more than 15 different countries. It has managed to bring the global health implications of scabies to the attention of the World Health Organization.[41] Consequently, the WHO has included scabies on its official list of neglected tropical diseases and other neglected conditions.[50]
Other animals
Scabies may occur in a number of domestic and wild animals; the mites that cause these infestations are of different subspecies from the one typically causing the human form.[12] These subspecies can infest animals that are not their usual hosts, but such infections do not last long.[12] Scabies-infected animals suffer severe itching and secondary skin infections. They often lose weight and become frail.[19]
The most frequently diagnosed form of scabies in domestic animals is sarcoptic mange, caused by the subspecies Sarcoptes scabiei canid, most commonly in dogs and cats. Sarcoptic mange is transmissible to humans who come into prolonged contact with infested animals,[51] and is distinguished from human scabies by its distribution on skin surfaces covered by clothing. Scabies-infected domestic fowl suffer what is known as "scaly leg". Domestic animals that have gone feral and have no veterinary care are frequently afflicted with scabies and a host of other ailments.[52] Nondomestic animals have also been observed to suffer from scabies. Gorillas, for instance, are known to be susceptible to infection via contact with items used by humans.[53]
References
- 1 2 3 4 5 6 "Epidemiology & Risk Factors". Centers for Disease Control and Prevention. November 2, 2010. Retrieved 18 May 2015.
- ↑ Gates, Robert H. (2003). Infectious disease secrets (2. ed.). Philadelphia: Elsevier, Hanley Belfus. p. 355. ISBN 978-1-56053-543-0.
- 1 2 3 "Parasites - Scabies Disease". Center for Disease Control and Prevention. November 2, 2010. Retrieved 18 May 2015.
- 1 2 "Parasites - Scabies Treatment". Center for Disease Control and Prevention. November 2, 2010. Retrieved 18 May 2015.
- 1 2 "WHO -Water-related Disease". World Health Organization. Retrieved 2010-10-10.
- 1 2 "Scabies". World Health Organization. Retrieved 18 May 2015.
- ↑ "Parasites - Scabies Medications". Center for Disease Control and Prevention. November 2, 2010. Retrieved 18 May 2015.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Andrews RM, McCarthy J, Carapetis JR, Currie BJ (December 2009). "Skin disorders, including pyoderma, scabies, and tinea infections". Pediatr. Clin. North Am. 56 (6): 1421–40. doi:10.1016/j.pcl.2009.09.002. PMID 19962029.
- 1 2 Vos, T (Dec 15, 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010.". Lancet 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ↑ Mosby's Medical, Nursing & Allied Health Dictionary (4 ed.). Mosby-Year Book Inc. 1994. p. 1395. ISBN 9780801672255.
- ↑ Georgis' Parasitology for Veterinarians (10 ed.). Elsevier Health Sciences. 2014. p. 68. ISBN 9781455739882.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Hay RJ (2009). "Scabies and pyodermas—diagnosis and treatment". Dermatol Ther 22 (6): 466–74. doi:10.1111/j.1529-8019.2009.01270.x. PMID 19889132.
- 1 2 3 Markell, Edward K.; John, David C.; Petri, William H. (2006). Markell and Voge's medical parasitology (9th ed.). St. Louis, Mo: Elsevier Saunders. ISBN 0-7216-4793-6.
- 1 2 CDC web site > DPDx - Laboratory Identification of Parasites of Public Health Concern > Scabies
- 1 2 "Scabies" (PDF). DermNet NZ. New Zealand Dermatological Society Incorporated.
- 1 2 3 Bouvresse, S.; Chosidow, O. (Apr 2010). "Scabies in healthcare settings". Curr Opin Infect Dis 23 (2): 111–8. doi:10.1097/QCO.0b013e328336821b. PMID 20075729.
- ↑ Hicks MI, Elston DM (2009). "Scabies". Dermatol Ther 22 (4): 279–92. doi:10.1111/j.1529-8019.2009.01243.x. PMID 19580575.
- 1 2 "DPDx—Scabies". Laboratory Identification of Parasites of Public Health Concern. CDC.
- 1 2 3 4 Walton, SF; Currie, BJ (April 2007). "Problems in Diagnosing Scabies, a Global Disease in Human and Animal Populations". Clinical Microbiology Reviews 20 (2): 268–79. doi:10.1128/CMR.00042-06. PMC 1865595. PMID 17428886.
- ↑ "Problems in Diagnosing Scabies, a Global Disease in Human and Animal Populations". Clinical Microbiology Reviews 20 (2): 268–279. 2007. doi:10.1128/CMR.00042-06. PMC 1865595. PMID 17428886.
- ↑ Carol Turkington and Jeffrey S. Dover, M.D. (2006). The Encyclopedia of Skin and Skin Disorders. New York: Facts on File inc. ISBN 978-0-8160-6403-8.
- ↑ "Scabies Causes". WebMD. October 2010. Retrieved 2010-10-09.
- ↑ Chosidow O (April 2006). "Clinical practices. Scabies". N. Engl. J. Med. 354 (16): 1718–27. doi:10.1056/NEJMcp052784. PMID 16625010.
- ↑ "Scabies—Fast Facts". American Social Health Association. Retrieved 2010-10-09.
- ↑ FitzGerald, Deirdre; Grainger, Rachel J.; Reid, Alex (2014). "Interventions for preventing the spread of infestation in close contacts of people with scabies". The Cochrane Database of Systematic Reviews 2: CD009943. doi:10.1002/14651858.CD009943.pub2. ISSN 1469-493X. PMID 24566946.
- ↑ Arlian, LG (1989). "Biology, host relations, and epidemiology of Sarcoptes scabiei". Annual review of entomology 34 (1): 139–61. doi:10.1146/annurev.en.34.010189.001035. PMID 2494934.
- ↑ "CDC—Prevention and Control—Scabies". Center for Disease Control and Prevention. Retrieved 2010-10-09.
- ↑ Vañó-Galván, S; Moreno-Martin, P (2008). "Generalized pruritus after a beach vacation. Diagnosis: scabies". Cleveland Clinic journal of medicine 75 (7): 474, 478. doi:10.3949/ccjm.75.7.474. PMID 18646583.
- ↑ "Parasites - Scabies". cdc.gov. November 2, 2010. Retrieved 11 December 2014.
- ↑ Strong M, Johnstone PW (2007). Strong, Mark, ed. "Interventions for treating scabies". Cochrane Database Syst Rev (3): CD000320. doi:10.1002/14651858.CD000320.pub2. PMID 17636630.
- 1 2 "Scabies". Illinois Department of Public Health. January 2008. Retrieved 2010-10-07.
- ↑ The Pill Book. Bantam Books. 2010. pp. 867–869. ISBN 978-0-553-59340-2.
- ↑ Victoria J, Trujillo R (2001). "Topical ivermectin: a new successful treatment for scabies". Pediatr Dermatol 18 (1): 63–5. doi:10.1046/j.1525-1470.2001.018001063.x. PMID 11207977.
- ↑ "Parasitology Research, Volume 78, Number 2". SpringerLink. Retrieved 2010-11-14.
- ↑ Humphreys, EH; Janssen, S; Heil, A; Hiatt, P; Solomon, G; Miller, MD (March 2008). "Outcomes of the California ban on pharmaceutical lindane: clinical and ecologic impacts.". Environmental health perspectives 116 (3): 297–302. doi:10.1289/ehp.10668. PMC 2265033. PMID 18335094.
- ↑ "FDA Public Health Advisory: Safety of Topical Lindane Products for the Treatment of Scabies and Lice". Fda.gov. 2009-04-30. Retrieved 2010-11-14.
- ↑ Jin-Gang A, Sheng-Xiang X, Sheng-Bin X, et al. (March 2010). "Quality of life of patients with scabies". J Eur Acad Dermatol Venereol 24 (10): 1187–91. doi:10.1111/j.1468-3083.2010.03618.x. PMID 20236379.
- ↑ Müller, Melissa (1999) [1998]. Das Mädchen Anne Frank [Anne Frank: The Biography] (in German). Kimber, Rita and Robert (translators). New York: Henry Holt and Company. ISBN 978-0-7475-4523-1. OCLC 42369449.; With a note from Miep Gies. Pp. 246-247.
- ↑ Andrews, RM; McCarthy, J; Carapetis, JR; Currie, BJ (Dec 2009). "Skin disorders, including pyoderma, scabies, and tinea infections.". Pediatric clinics of North America 56 (6): 1421–40. doi:10.1016/j.pcl.2009.09.002. PMID 19962029.
- 1 2 3 Hay, RJ; Steer, AC; Chosidow, O; Currie, BJ (Apr 2013). "Scabies: a suitable case for a global control initiative.". Current opinion in infectious diseases 26 (2): 107–9. doi:10.1097/QCO.0b013e32835e085b. PMID 23302759.
- 1 2 3 4 Engelman, D; Kiang, K; Chosidow, O; McCarthy, J; Fuller, C; Lammie, P; Hay, R; Steer, A; Members Of The International Alliance For The Control Of, Scabies (2013). "Toward the global control of human scabies: introducing the International Alliance for the Control of Scabies.". PLoS neglected tropical diseases 7 (8): e2167. doi:10.1371/journal.pntd.0002167. PMID 23951369.
- ↑ Green MS (1989). "Epidemiology of scabies". Epidemiol Rev 11 (1): 126–50. PMID 2509232.
- ↑ Hicks, MI; Elston, DM (Jul–Aug 2009). "Scabies". Dermatologic therapy 22 (4): 279–92. doi:10.1111/j.1529-8019.2009.01243.x. PMID 19580575.
- 1 2 "Scabies homepage". Stanford University. Retrieved 2010-10-09.
- ↑ Leviticus 13:29-13:37
- ↑ See translations
- 1 2 3 Roncalli RA (July 1987). "The history of scabies in veterinary and human medicine from biblical to modern times". Vet. Parasitol. 25 (2): 193–8. doi:10.1016/0304-4017(87)90104-X. PMID 3307123.
- ↑ "Scabies". Neglected tropical diseases. World Health Organization. Retrieved 1 February 2014.
- ↑ "International Alliance for the Control of Scabies". International Alliance for the Control of Scabies. Retrieved 1 February 2014.
- ↑ "The 17 neglected tropical diseases". Neglected tropical diseases. World Health Organization. Retrieved 1 February 2014.
- ↑ Borgman W (June 30, 2006). Dog mange called scabies can transfer to humans. Orlando Sentinel archive. Retrieved February 16, 2015.
- ↑ "Bali Animal Welfare Association". Retrieved 2009-07-28.
- ↑ "Uganda: Out of the Wild". Frontlinehttp://www.pbs.org/wgbh/pages/frontline/tehranbureau/deathintehran/etc/script.html
|transcripturl=missing title (help). PBS. Retrieved Nov 4, 2013.
External links
| Wikimedia Commons has media related to Scabies. |
- American Academy of Dermatology pamphlet on Scabies
- Scabies FAQ from the National Pediculosis Association
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||
