Raynaud's phenomenon
| Raynaud's phenomenon | |
|---|---|
 Hands with Raynaud's phenomenon | |
| Classification and external resources | |
| Specialty | Rheumatology |
| ICD-10 | I73.0 |
| ICD-9-CM | 443.0 |
| OMIM | 179600 |
| DiseasesDB | 25933 |
| MedlinePlus | 000412 |
| eMedicine | med/1993 |
| Patient UK | Raynaud's phenomenon |
| MeSH | D011928 |
In medicine, Raynaud's disease or Raynaud's phenomenon (pronunciation: /reɪˈnoʊz/ ray-NOHZ) is excessively reduced blood flow in response to cold or emotional stress, causing discoloration of the fingers, toes, and occasionally other areas. This condition may also cause nails to become brittle with longitudinal ridges. Named after French physician Maurice Raynaud (1834–1881), the phenomenon is believed to be the result of vasospasms that decrease blood supply to the respective regions.
When the disorder's cause is idiopathic, it is referred to as Raynaud's disease (also called primary Raynaud's); if the syndrome is secondary to another disease such as systemic sclerosis, systemic lupus erythematosus, or other connective tissue disorders, it is correctly referred to as Raynaud's phenomenon (secondary Raynaud's).[1] If Raynaud's phenomenon is suspected to be secondary to systemic sclerosis, one tool which may help aid in the prediction of systemic sclerosis is thermography.[2]
Its pathophysiology includes hyperactivation of the sympathetic nervous system causing extreme vasoconstriction of the peripheral blood vessels, leading to tissue hypoxia. Chronic, recurrent cases of Raynaud's phenomenon can result in atrophy of the skin, subcutaneous tissues, and muscle. In rare cases it can cause ulceration and ischemic gangrene.[3]
Signs and symptoms

The condition can cause pain within the affected extremities, discoloration (paleness), and sensations of cold and/or numbness. This can often be distressing to those who are not diagnosed, and sometimes it can be obstructive. If someone with Raynaud's is placed into a cold climate, it could potentially become dangerous.
.jpg)
- When exposed to cold temperatures, the blood supply to the fingers or toes, and in some cases the nose or earlobes, is markedly reduced; the skin turns pale or white (called pallor) and becomes cold and numb.
- When the oxygen supply is depleted, the skin color turns blue (called cyanosis).
- These events are episodic, and when the episode subsides or the area is warmed, the blood flow returns, and the skin color first turns red (rubor), and then back to normal, often accompanied by swelling, tingling, and a painful "pins and needles" sensation.
All three color changes are observed in classic Raynaud's. However, not all patients see all of the aforementioned color changes in all episodes, especially in milder cases of the condition. Symptoms are thought to be due to reactive hyperemias of the areas deprived of blood flow.
In pregnancy, this sign normally disappears owing to increased surface blood flow. Raynaud's has also occurred in breastfeeding mothers, causing nipples to turn white and become extremely painful.[4] Nifedipine, a calcium channel blocker and vasodilator, was recommended to increase blood flow to the extremities and noticeably relieved pain in the breast in an extremely small study group.[5]
Cause
Primary
Raynaud's disease, or "Primary Raynaud's", is diagnosed if the symptoms are idiopathic, that is, if they occur by themselves and not in association with other diseases. Some refer to Primary Raynaud's disease as "being allergic to coldness". It often develops in young women in their teens and early adulthood. Primary Raynaud's is thought to be at least partly hereditary, although specific genes have not yet been identified.[6]
Smoking increases frequency and intensity of attacks, and there is a hormonal component. Caffeine also worsens the attacks. Sufferers are more likely to have migraines and angina.
Secondary
Raynaud's phenomenon, or "Secondary Raynaud's", occurs secondary to a wide variety of other conditions.
Secondary Raynaud's has a number of associations:
- Connective tissue disorders:
- Eating disorders:
- Obstructive disorders:
- Drugs:
- beta-blockers
- cytotoxic drugs – particularly chemotherapeutics and most especially bleomycin
- ciclosporin
- bromocriptine
- ergotamine
- sulfasalazine
- anthrax vaccines whose primary ingredient is the Anthrax Protective Antigen
- stimulant medications such as those used to treat ADHD[8]
- OTC psedoephedrine medications (Chlor-Trimeton, Sudafed, others)[9]
- Occupation:
- jobs involving vibration, particularly drilling and prolonged use of a String trimmer (weed whacker), suffer from vibration white finger
- exposure to vinyl chloride, mercury
- exposure to the cold (e.g., by working as a frozen food packer)
- Others:
- physical trauma, such as that sustained in auto accidents or other traumatic events
- Lyme disease
- hypothyroidism
- cryoglobulinemia
- malignancy
- chronic fatigue syndrome
- reflex sympathetic dystrophy
- carpal tunnel syndrome
- magnesium deficiency
- multiple sclerosis
- erythromelalgia (clinically presenting as the opposite of Raynaud's, with hot and warm extremities) often co-exists in patients with Raynaud's[10])
Raynaud's can herald these diseases by periods of more than twenty years in some cases, making it effectively their first presenting symptom. This may be the case in the CREST syndrome, of which Raynaud's is a part.
Patients with Secondary Raynaud's can also have symptoms related to their underlying diseases. Raynaud's phenomenon is the initial symptom that presents for 70% of patients with scleroderma, a skin and joint disease.
When Raynaud's phenomenon is limited to one hand or one foot, it is referred to as Unilateral Raynaud's. This is an uncommon form, and it is always secondary to local or regional vascular disease. It commonly progresses within several years to affect other limbs as the vascular disease progresses.[11]
Diagnosis
It is important to distinguish Raynaud's disease (primary Raynaud's) from phenomenon (secondary Raynaud's). Looking for signs of arthritis or vasculitis as well as a number of laboratory tests may separate them.
A careful medical history will often reveal whether the condition is primary or secondary. Once this has been established, an examination is largely to identify or exclude possible secondary causes.
- Digital artery pressure: pressures are measured in the arteries of the fingers before and after the hands have been cooled. A decrease of at least 15 mmHg is diagnostic (positive).
- Doppler ultrasound: to assess blood flow.
- Full blood count: this may reveal a normocytic anaemia suggesting the anaemia of chronic disease or renal failure.
- Blood test for urea and electrolytes: this may reveal renal impairment.
- Thyroid function tests: this may reveal hypothyroidism.
- An autoantibody screen, tests for rheumatoid factor, Erythrocyte sedimentation rate, and C-reactive protein, which may reveal specific causative illnesses or a generalised inflammatory process.
- Nail fold vasculature: this can be examined under the microscope.
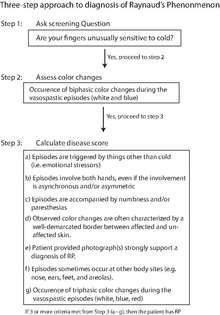
To aid in the diagnosis of Raynaud's phenomenon, multiple sets of diagnostic criteria have been proposed.[12][13][14][15] Table 1 below provides a summary of these various diagnostic criteria.[16]
Recently, International Consensus Criteria were developed for the diagnosis of primary Raynaud's phenomenon by a panel of multiple experts in the fields of rheumatology and dermatology.[16]
Management
Raynaud's phenomenon (secondary Raynaud's) is managed primarily by treating the underlying cause and as with Raynaud's disease (primary Raynaud's), avoiding triggers, such as cold, emotional and environmental stress, vibrations and repetitive motions, and avoiding smoking (including passive smoking) and sympathomimetic drugs.[17]
Drugs can be helpful for moderate or severe RP.
- Vasodilators – calcium channel blockers such as the dihydropyridines nifedipine, amlodipine or diltiazem, preferably slow release preparations – are often first line treatment.[17] They have the common side effects of headache, flushing, and ankle edema; but these are not typically of sufficient severity to require cessation of treatment.[18] The limited evidence available shows that calcium channel blockers are only slightly effective in reducing how often the attacks happen.[19] Patients whose RP is secondary to Erythromelalgia often cannot use vasodilators for therapy as they trigger 'Flares' in EM patients causing the extremities to become burning red due to there being too much blood in the extremity.
- Patients with severe RP prone to ulceration or large artery thrombotic events may be prescribed aspirin.[17]
- Sympatholytic agents, such as the alpha-adrenergic blocker prazosin may provide temporary relief.[17]
- Losartan can, and topical nitrates may, reduce the severity and frequency of attacks, and the phosphodiesterase inhibitors sildenafil and tadalafil may reduce their severity.[17]
- Angiotensin receptor blockers or ACE inhibitors may aid blood flow to the fingers,[17] and there is some evidence that angiotensin receptor blockers (often losartan) reduce frequency and severity of attacks,[20] and possibly better than nifedipine.[21][22]
- The prostaglandin iloprost is used to manage critical ischemia and pulmonary hypertension in RP, and the endothelin receptor antagonist bosentan is used to manage severe pulmonary hypotension and prevent finger ulcers in SSc.[17]
- Statins have a protective effect on blood vessels, and SSRIs such as fluoxetine may help RP symptoms but the data is weak.[17]
Surgery
- In severe cases, a Endoscopic thoracic sympathectomy (ETS) procedure can be performed.[23] Here, the nerves that signal the blood vessels of the fingertips to constrict are surgically cut. Microvascular surgery of the affected areas is another possible therapy. This procedure should be considered as a last resort however.
- Infusions of prostaglandins, e.g. prostacyclin, may be tried, with amputation in exceptionally severe cases.
- A more recent treatment for severe Raynaud's is the use of botulinum toxin. The 2009 article[24] studied 19 patients ranging in age from 15 to 72 years with severe Raynaud's phenomenon of which 16 patients (84%) reported pain reduction at rest. 13 patients reported immediate pain relief, 3 more had gradual pain reduction over 1–2 months. All 13 patients with chronic finger ulcers healed within 60 days. Only 21% of the patients required repeated injections. A 2007 article[25] describes similar improvement in a series of 11 patients. All patients had significant relief of pain.
Low level laser therapy
Low level laser therapy has been shown to reduce frequency and severity of Raynaud attacks in patients. Results varied depending on the other symptoms present with the disease. [26] [27]
See also
References
- ↑ "What Is Raynaud's?". National Heart, Lung, and Blood Institute (NHLBI).
- ↑ Anderson ME, Moore TL, Lunt M, Herrick AL (March 2007). "The 'distal-dorsal difference': a thermographic parameter by which to differentiate between primary and secondary Raynaud's phenomenon". Rheumatology 46 (3): 533–8. doi:10.1093/rheumatology/kel330. PMID 17018538.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease. St. Louis, Mo: Elsevier Saunders. p. 542. ISBN 0-7216-0187-1.
- ↑ Holmen OL, Backe B (2009). "An underdiagnosed cause of nipple pain presented on a camera phone". BMJ 339: b2553. doi:10.1136/bmj.b2553.
- ↑ Anderson JE, Held N, Wright K (April 2004). "Raynaud's phenomenon of the nipple: a treatable cause of painful breastfeeding". Pediatrics 113 (4): e360–4. doi:10.1542/peds.113.4.e360. PMID 15060268.
- ↑ Pistorius MA, Planchon B, Schott JJ, Lemarec H (February 2006). "[Heredity and genetic aspects of Raynaud's disease]". Journal Des Maladies Vasculaires (in French) 31 (1): 10–5. doi:10.1016/S0398-0499(06)76512-X. PMID 16609626.
- ↑ Gayraud M (January 2007). "Raynaud's phenomenon". Joint, Bone, Spine 74 (1): e1–8. doi:10.1016/j.jbspin.2006.07.002. PMID 17218139.
- ↑ Goldman, William, Ryan Seltzer, and Peter Reuman. "Association between treatment with central nervous system stimulants and Raynaud's syndrome in children: A retrospective case–control study of rheumatology patients." Arthritis & Rheumatism 58.2 (2008): 563-566.
- ↑ "Raynaud's disease Treatments and drugs - Mayo Clinic". www.mayoclinic.org. Retrieved 2015-12-13.
- ↑ Berlin AL, Pehr K (March 2004). "Coexistence of erythromelalgia and Raynaud's phenomenon". Journal of the American Academy of Dermatology 50 (3): 456–60. doi:10.1016/S0190-9622(03)02121-2. PMID 14988692.
- ↑ Priollet P (October 1998). "[Raynaud's phenomena: diagnostic and treatment study]". La Revue du praticien (in French) 48 (15): 1659–64. PMID 9814067.
- ↑ Brennan P, Silman A, Black C (May 1993). "Validity and reliability of three methods used in the diagnosis of Raynaud's phenomenon. The UK Scleroderma Study Group". British Journal of Rheumatology 32 (5): 357–361. doi:10.1093/rheumatology/32.5.357. PMID 8495253.
- ↑ Wigley FM (September 2002). "Clinical Practice.Raynaud's phenomenon". New England Journal of Medicine 347 (13): 1001–1008. doi:10.1056/nejmcp013013. PMID 12324557.
- ↑ LeRoy EC, Medsger TA (September–October 1992). "Raynaud's phenomenon: a proposal for classification". Clinical and Experimental Rheumatology 10 (5): 485–488. PMID 1458701.
- ↑ Maricq HR, Weinrich MC (March 1998). "Diagnosis of Raynaud's phenomenon assisted by color charts". Journal of Rheumatology 15 (3): 454–459. PMID 3379622.
- 1 2 Maverakis E, Patel F, Kronenberg D (2014). "International consensus criteria for the diagnosis of Raynaud's phenomenon". Journal of Autoimmunity 48: 60–5. doi:10.1016/j.jaut.2014.01.020. PMC 4018202. PMID 24491823.
- 1 2 3 4 5 6 7 8 Mikuls, Ted R; Canella, Amy C; Moore, Gerald F; Erickson, Alan R; Thiele, Geoffery M; O'Dell, James R (2013). "Connective Tissue Diseases". Rheumatology. London: Manson Publishing. p. 117. ISBN 978-1-84076-173-3.
- ↑ Smith CR, Rodeheffer RJ (January 1985). "Raynaud's phenomenon: pathophysiologic features and treatment with calcium-channel blockers". The American Journal of Cardiology 55 (3): 154B–157B. doi:10.1016/0002-9149(85)90625-3. PMID 3881908.
- ↑ Ennis H, Anderson ME, Wilkinson J, Herrick AL (2014). "Calcium channel blockers for primary Raynaud's phenomenon.". Cochrane Database Syst Rev 1: CD002069. doi:10.1002/14651858.CD002069.pub4. PMID 24482037.
- ↑ Pancera P, Sansone S, Secchi S, Covi G, Lechi A (November 1997). "The effects of thromboxane A2 inhibition (picotamide) and angiotensin II receptor blockade (losartan) in primary Raynaud's phenomenon". Journal of Internal Medicine 242 (5): 373–6. doi:10.1046/j.1365-2796.1997.00219.x. PMID 9408065.
- ↑ Dziadzio M, Denton CP, Smith R, et al. (December 1999). "Losartan therapy for Raynaud's phenomenon and scleroderma: clinical and biochemical findings in a fifteen-week, randomized, parallel-group, controlled trial". Arthritis and Rheumatism (Elsevier Saunergic blockers such as prazosin can be used to control Raynaud's vasospasms under supervision of a health care provider) 42 (12): 2646–55. doi:10.1002/1529-0131(199912)42:12-2646:AID-ANR21-3.0.CO;2-T (inactive 2015-10-18). PMID 10616013.
- ↑ Waldo R (March 1979). "Prazosin relieves Raynaud's vasospasm". JAMA 241 (10): 1037. doi:10.1001/jama.241.10.1037. PMID 762741.
- ↑ Wang WH, Lai CS, Chang KP, et al. (October 2006). "Peripheral sympathectomy for Raynaud's phenomenon: a salvage procedure". The Kaohsiung Journal of Medical Sciences 22 (10): 491–9. doi:10.1016/S1607-551X(09)70343-2. PMID 17098681.
- ↑ Neumeister MW, Chambers CB, Herron MS, et al. (July 2009). "Botox therapy for ischemic digits". Plastic and Reconstructive Surgery 124 (1): 191–201. doi:10.1097/PRS.0b013e3181a80576. PMID 19568080.
- ↑ Van Beek AL, Lim PK, Gear AJ, Pritzker MR (January 2007). "Management of vasospastic disorders with botulinum toxin A". Plastic and Reconstructive Surgery 119 (1): 217–26. doi:10.1097/01.prs.0000244860.00674.57. PMID 17255677.
- ↑ Hirschl, M. et. al (December 2004). "Low level laser therapy in primary Raynaud's phenomenon--results of a placebo controlled, double blind intervention study.". J Rheumatol. 31 (12): 2408–12. PMID 15570642.
- ↑ Koyama, T. et. al (July 2007). "LOW REACTIVE-LEVEL LASER THERAPY IMPROVED SYSTEMIC SCLEROSIS-ASSOCIATED RAYNAUD’S PHENOMENON". LASER THERAPY 16 (3): 151–157. doi:10.5978/islsm.16.151.
Further reading
- Bakst R, Merola JF, Franks AG, Sanchez M (October 2008). "Raynaud's phenomenon: pathogenesis and management". Journal of the American Academy of Dermatology 59 (4): 633–53. doi:10.1016/j.jaad.2008.06.004. PMID 18656283.
External links
| Wikimedia Commons has media related to Raynaud's phenomenon. |
- Raynaud's & Scleroderma Association, a national charity and self-help organisation, committed to supporting patients and carers who have these conditions
- Questions and Answers about Raynaud’s Phenomenon at National Institutes of Health
- Overview at Medical College of Wisconsin
- Raynaud's Disease at healthatoz.com
- Raynaud's Phenomenon on YouTube
- Raynaud's Disease on YouTube
- What Is Raynaud's Disease at National Heart, Lung, and Blood Institute
- Testimonial of cure for Raynaud's phenomenon
- Raynaud's Disease at Mayo Clinic
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|