Gingival and periodontal pocket
Both the gingival and periodontal pocket are extensions of the gingival sulcus, which exists in health. Gingival and periodontal pockets are dental terms indicating the presence of an abnormal depth of the gingival sulcus near the point at which the gingival tissue contacts the tooth.
Tooth gingival interface
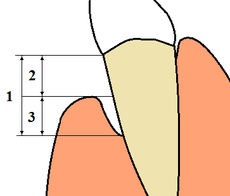
The interface between a tooth and the surrounding gingival tissue is a dynamic structure.[1] The gingival tissue forms a crevice surrounding the tooth, similar to a miniature, fluid-filled moat, wherein food debris, endogenous and exogenous cells, and chemicals float. The depth of this crevice, known as a sulcus, is in a constant state of flux due to microbial invasion and subsequent immune response. Located at the depth of the sulcus is the epithelial attachment, consisting of approximately 1 mm of junctional epithelium and another 1 mm of gingival fiber attachment, comprising the 2 mm of biologic width naturally found in the oral cavity. The sulcus is literally the area of separation between the surrounding epithelium and the surface of the encompassed tooth.
Gingival sulcus
A healthy sulcular depth is 3 millimeters or less. Through much investigation and research, it has been determined that sulcular depths of 3 millimeters or less are readily self-cleansable with a properly used toothbrush or the supplemental use of other oral hygiene aids. When the sulcular depth is chronically in excess of three millimeters, regular home care may be insufficient to properly cleanse the full depth of the sulcus, allowing food debris and microbes to accumulate, forming dental biofilm. This poses a danger to the periodontal ligament (PDL) fibers that attach the gingiva to the tooth. If accumulated microbes remain undisturbed in a sulcus for an extended period of time, they will penetrate and ultimately destroy the delicate soft tissue and periodontal attachment fibers. If left untreated, this process may lead to a deepening of the sulcus, recession, destruction of the periodontium, including the bony tooth socket, tooth mobility, and tooth loss.[2]
Gingival pocket
A gingival pocket presents when the marginal gingiva experiences an edematous reaction, whether due to localized irritation and subsequent inflammation, systemic issues, or drug induced gingival hyperplasia. Regardless of the etiology, when gingival hyperplasia occurs, greater than normal (the measurement in a pre-pathological state) periodontal probing measurements can be read, creating the illusion that periodontal pockets have developed. This phenomenon is also referred to as a false pocket or pseudopocket. The epithelial attachment does not migrate, it simply remains at the same attachment level found in pre-pathological health. The only anatomical landmark experiencing migration is the gingival margin in a coronal direction.
In a gingival pocket, no destruction of the connective tissue fibers (gingival fibers) or alveolar bone occurs. This early sign of disease in the mouth is completely reversible when the etiology of the edematous reaction is eliminated and frequently occurs without dental surgical therapy. However, in certain situations, a gingivectomy is necessary to reduce the gingival pocket depths to a healthy 1–3 mm.
Periodontal pocket
As the original sulcular depth increases and the apical migration of the junctional epithelium has simultaneously occurred, the pocket is now lined by pocket epithelium (PE) instead of junctional epithelium (JE).[3] To have a true periodontal pocket, a probing measurement of 4 mm or more must be clinically evidenced. In this state, much of the gingival fibers that initially attached the gingival tissue to the tooth have been irreversibly destroyed. The depth of the periodontal pockets must be recorded in the patient record for proper monitoring of periodontal disease. Unlike in clinically healthy situations, parts of the sulcular epithelium can sometimes be seen in periodontally involved gingival tissue if air is blown into the periodontal pocket, exposing the newly denuded roots of the tooth. A periodontal pocket can become an infected space and may result in an abscess formation with a papule on the gingival surface. Incision and drainage of the abscess may be necessary, as well as systemic antibiotics; placement of local antimicrobial delivery systems within the periodontal pocket to reduce localized infections may also be considered. It is classified as supra bony and infra bony based on its depth in relation to alveolar bone [4]
Mucogingival defect
If the destruction continues unabated apically and reaches the junction of the attached gingiva and alveolar mucosa, the pocket would thus be in violation of the mucogingival junction and would be termed a mucogingival defect.[5]
External links
- Microflora and periodontal disease, Dent Res J (Isfahan). 2012 December; 9(Suppl 2): S202–S206, Luca Scapoli, et al. at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3692174/
References
- ↑ Fermin A. Carranza. CARRANZA'S CLINICAL PERIODONTOLOGY, 9th edition, 2002. page 101
- ↑ Antonio Nanci, Ten Cate's Oral Histology, Elsevier, 2007, page 3
- ↑ Antonio Nanci, Ten Cate's Oral Histology, Elsevier, 2007, page 383
- ↑ Illustrated Dental Embryology, Histology, and Anatomy, Bath-Balogh and Fehrenbach, Elsevier, 2011, page 129
- ↑ Carranza's Clinical Periodontology, Newman, et al, Elsevier, 2011
| ||||||||||||||||||||||||||||||||||||