Patellofemoral pain syndrome
| Patellofemoral pain syndrome | |
|---|---|
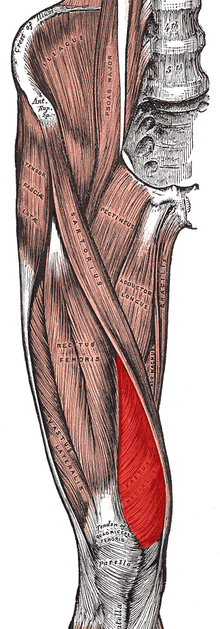
 Diagram of the bones of the lower extremity. Rough distribution of areas affected by PFPS highlighted in red: patella and distal femur. | |
| Classification and external resources | |
| Specialty | Orthopedics, sports medicine |
| ICD-10 | M22.2 |
| ICD-9-CM | 719.46 |
| DiseasesDB | 33163 |
| eMedicine | article/308471 |
| Patient UK | Patellofemoral pain syndrome |
| MeSH | D046788 |
Patellofemoral pain syndrome (PFPS) is a syndrome characterized by knee pain ranging from severe to mild discomfort seemingly originating from the contact of the posterior surface of the patella (back of the kneecap) with the femur (thigh bone).
The population most at risk from PFPS are runners, cyclists, basketball players and other sports participants. Onset can be gradual or the result of a single incident and is often caused by a change in training regime that includes dramatic increases in training time, distance or intensity, it can be compounded by worn or inappropriate footwear. Symptoms include discomfort while sitting with bent knees or descending stairs and generalised knee pain. Treatment involves resting and physical therapy that includes stretching and strengthening exercises for the legs.
Definition
There is no universally accepted definition. Selected definitions include:
- "anterior knee pain involving the patella and retinaculum that excludes other intraarticular and peri-patellar pathology"[1]
Runner's knee
PFPS is one of a handful of conditions sometimes referred to as runner's knee.[1] The other conditions being Chondromalacia patellae, Iliotibial band syndrome, and Plica syndrome
Patellofemoral pain syndrome vs. chondromalacia patellae
Chondromalacia patellae is a term sometimes treated synonymously with PFPS.[2] However, there is general consensus that PFPS is a term that applies only to individuals without cartilage damage,[2] thereby distinguishing it from chondromalacia patellae, a condition characterized by softening of the patellar articular cartilage.[1] Despite this academic distinction, the diagnosis of PFPS is typically made clinically, based only on the history and physical examination rather than on the results of any medical imaging. Therefore, it is unknown whether most persons with a diagnosis of PFPS have cartilage damage or not, making the difference between PFPS and chondromalacia theoretical rather than practical.[2] It is thought that only some individuals with anterior knee pain will have true chondromalacia patellae.[1]
Signs and symptoms
The onset of the condition is usually gradual,[3] although some cases may appear suddenly following trauma.[1]
- Knee pain - the most common symptom is diffuse peripatellar pain (vague pain around the kneecap) and localized retropatellar pain (pain focused behind the kneecap). Affected individuals typically have difficulty describing the location of the pain, and may place their hands over the anterior patella or describe a circle around the patella (the "circle sign").[1] Pain is usually initiated when load is put on the knee extensor mechanism, e.g. ascending or descending stairs or slopes, squatting, kneeling, cycling, running or prolonged sitting with flexed (bent) knees.[2][4][5] The latter feature is sometimes termed the "movie sign" or "theatre sign" because individuals might experience pain while sitting to watch a film or similar activity.[2] The pain is typically aching with occasional sharp pains.[1]
- Crepitus (joint noises)[2] may be present
- Giving-way of the knee[2] may be reported
Causes
In most patients with PFPS an examination of their history will highlight a precipitating event that caused the injury. Changes in activity patterns such as excessive increases in running mileage, repetitions such as running up steps and the addition of strength exercises that affect the patellofemoral joint are commonly associated with symptom onset. Excessively worn or poorly fitted footwear often contribute. To prevent recurrence the causal behaviour should be identified and managed correctly.[1]
The medical cause of PFPS is thought to be increased pressure on the patellofemoral joint.[2] There are several theorized mechanisms relating to how this increased pressure occurs:
- Increased levels of physical activity[2]
- Malalignment of the patella as it moves through the femoral groove[2]
- Quadriceps muscle imbalance[2]
- Tight anatomical structures, e.g. retinaculum or iliotibial band.[2]
The cause of pain and dysfunction often results from either abnormal forces (e.g. increased pull of the lateral quadriceps retinaculum with acute or chronic lateral PF subluxation/dislocation) or prolonged repetitive compressive or shearing forces (running or jumping) on the PF joint. The result is synovial irritation and inflammation and subchondral bony changes in the distal femur or patella known as "bone bruises". Secondary causes of PF Syndrome are fractures, internal knee derangement, osteoarthritis of the knee and bony tumors in or around the knee.[6]
Diagnosis
Differential diagnosis
The diagnosis of patellofemoral pain syndrome is made by ruling out patellar tendinitis, prepatellar bursitis, plica syndrome, Sinding–Larsen–Johansson syndrome, and Osgood–Schlatter disease.[7]
Examination
Patellofemoral grinding test.[8]
Treatment
As patellofemoral pain syndrome is the most common cause of anterior knee pain in the outpatient,[1] a variety of treatments for patellofemoral pain syndrome are implemented. However, there is little supporting evidence.[9] Most patients with patellofemoral pain syndrome respond well to conservative therapy.[9][10]
Exercises
There is consistent but very low quality evidence that exercise therapy for PFPS reduces pain, improves function and aids long-term recovery.[11] However, there is insufficient evidence to compare the effectiveness of different types of exercises with each other, and exercises with other forms of treatment.[11]
Exercise therapy is the recommended first line treatment of PFPS.[1] Various exercises have been studied and recommended.[12] Exercises are described according to 3 parameters:[4]
- Type of muscle activity (concentric, eccentric or isotonic)
- Type of joint movement (dynamic, isometric or static)
- Reaction forces (closed or open kinetic chain)
Concentric muscle activity involves contraction (shortening) of the muscle(s). During eccentric activities muscles lengthen in an actively controlled manner. During isotonic activity the muscle tension remains the same.[4]
Static/isometric exercises are those in which the position of the knee does not change, whereas dynamic exercises involves a change in the position of the knee. Isokinetic exercises are where the lower leg moves at a predetermined fixed speed, requiring an isokinetic dynamometer to control velocity.[4]
Where the foot is held in contact with a fixed surface, the term closed kinetic chain is used, and open kinetic chain when the surface is not fixed.[4]
The majority of exercise programs intended to treat PFPS are designed to strengthen the quadriceps muscles.[4] Emphasis during exercise may be placed on coordinated contraction of the medial and lateral parts of the quadriceps as well as of the hip adductor, hip abductor and gluteal muscles.[4] Many exercise programs include stretches designed to improve lower limb flexibility.[4] Electromyographic biofeedback allows visualization of specific muscle contractions and may help individuals performing the exercises to target the intended muscles during the exercise.[4] Electrostimulation may be used to apply external stimuli resulting in contraction of specific muscles and thus exercise.[2]
A 2011 systematic review stated that evidence supports the use of quadriceps exercise for managing patellofemoral pain syndrome and that quadriceps strengthening is considered to be the "gold" standard treatment for patellofemoral pain syndrome.[9] Quadriceps strengthening is commonly suggested because the quadriceps muscles help to stabilize the patella. Quadriceps weakness and quadriceps muscle imbalance may contribute to abnormal patellar tracking.[9] If the strength of the vastus medialis muscle is inadequate, the usually larger and stronger vastus lateralis muscle will pull sideways (laterally) on the kneecap. Strengthening the vastus medialis to prevent or counter the lateral force of the vastus lateralis is one way of relieving PFPS. Moderate evidence supports the addition of hip abductor and external rotator strengthening, as well as exercises targeting hip flexion and hip extension.[9][13][13] When executing these exercises, proper form is very important in order to ensure that the musculature is activated in such a way that will not lead to further injury. Inflexibility has often been cited as a source of patellofemoral pain syndrome. Stretching of the laterial knee has been suggested to help.[14]
Medication
Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used to treat PFPS, however there is only very limited evidence that they are effective.[2] NSAIDs may reduce pain in the short term, overall however, after three months pain is not improved.[15] There is no evidence that one type of NSAID is superior to another in PFPS, and therefore some authors have recommended that the NSAID with least side effects and which is cheapest should be used.[2]
Glycosaminoglycan polysulfate (GAGPS) inhibits proteolytic enzymes and increases synthesis and degree of polymerization of hyaluronic acid in synovial fluid.[2] There is contradictory evidence that it is effective in PFPS.[2]
Medical imaging
Magnetic resonance imaging rarely can give useful information for managing patellofemoral pain syndrome and treatment should focus on an appropriate rehabilitation program including correcting strength and flexibility concerns.[16] In the uncommon cases where a patient has mechanical symptoms like a locked knee, knee effusion, or failure to improve following physical therapy, then an MRI may give more insight into diagnosis and treatment.[16]
Rest
Patellofemoral pain syndrome may also result from overuse or overload of the PF joint. For this reason, knee activity should be reduced until the pain is resolved.[17][18] Those with pain originating from sitting too long should straighten the leg or walk periodically. Those who engage in high impact activity such as running should consider a nonimpact activity such as swimming.
Ice
To reduce inflammation ice can be applied to the PF joint after an activity. The ice should be kept in place for 10 to 15 minutes.
Braces and taping
There is no statistically or clinically significant difference in pain symptoms between taping and non-taping in individuals with PFPS.[15]
Knee braces are ineffective in treating PFPS.[15] The technique of McConnell taping involves pulling the patella medially with tape (medial glide). Findings from some studies suggest that there is limited benefit with patella taping or bracing when compared to quadriceps exercises alone.[9]
Arch support
Low arches can cause overpronation or the feet to roll inward too much increasing the Q angle and genu valgum. Poor lower extremity biomechanics may cause stress on the knees and ultimately patellofemoral pain syndrome. Stability or motion control shoes are designed for people with pronation issues. Arch supports and custom orthotics may also help to improve lower extremity biomechanics.[19][20]
Surgery
The scientific consensus is that surgery should be avoided except in very severe cases in which conservative treatments fail.[2] The majority of individuals with PFPS receive nonsurgical treatment.[4]
Treatments Lacking Supportive Research
There is no evidence to support the use of acupuncture, low-level laser therapy, or chiropractic patellar mobilization to treat PFPS.[21] Most studies touting the benefits of alternative therapies for PFPS were conducted with flawed experimental design, and therefore did not produce reliable results.[22]
Epidemiology
Specific populations at high risk of primary Patellofemoral Syndrome include runners, bicyclists, basketball players, young athletes and females.
See also
References
- 1 2 3 4 5 6 7 8 9 10 Dixit, S; DiFiori, JP; Burton, M; Mines, B (Jan 15, 2007). "Management of patellofemoral pain syndrome.". American family physician 75 (2): 194–202. PMID 17263214.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Heintjes, E; Berger, MY; Bierma-Zeinstra, SM; Bernsen, RM; Verhaar, JA; Koes, BW (2004). "Pharmacotherapy for patellofemoral pain syndrome.". The Cochrane database of systematic reviews (3): CD003470. doi:10.1002/14651858.CD003470.pub2. PMID 15266488.
- ↑ Callaghan, MJ; Selfe, J (Apr 18, 2012). "Patellar taping for patellofemoral pain syndrome in adults.". The Cochrane database of systematic reviews 4: CD006717. doi:10.1002/14651858.CD006717.pub2. PMID 22513943.
- 1 2 3 4 5 6 7 8 9 10 van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma-Zeinstra SMA, van Middelkoop M (2013). "Exercise for treating patellofemoral pain syndrome (Protocol)". Cochrane Database of Systematic Reviews 2: CD010387. doi:10.1002/14651858.CD010387.
- ↑ Smith TO, Drew BT, Meek TH, Clark AB (2013). "Knee orthoses for treating patellofemoral pain syndrome (Protocol)". Cochrane Database of Systematic Reviews 5: CD010513. doi:10.1002/14651858.CD010513.
- ↑ Plamondon, Tom (12 Aug 2009). "Special tests in the clinical examination of patellofemoral syndrome". Doctors Lounge. Retrieved 2012-08-20.
- ↑ Prins, Maarten R.; Van Der Wurff, Peter (2009). "Females with patellofemoral pain syndrome have weak hip muscles: A systematic review". Australian Journal of Physiotherapy 55 (1): 9–15. doi:10.1016/S0004-9514(09)70055-8. PMID 19226237.
- ↑ Gerard A. Malanga, Scott F. Nadler (2006). Musculoskeletal physical examination : an evidence-based approach. Philadelphia, Penns.: Elsevier Mosby. pp. 302–304. ISBN 9781560535911.
- 1 2 3 4 5 6 Bolgla, LA; Boling, MC (2011). "An update for the conservative management of patellofemoral pain syndrome: A systematic review of the literature from 2000 to 2010". International journal of sports physical therapy 6 (2): 112–25. PMC 3109895. PMID 21713229.
- ↑ Earl, JE; Vetter, CS (Aug 2007). "Patellofemoral pain". Physical medicine and rehabilitation clinics of North America 18 (3): 439–58, viii. doi:10.1016/j.pmr.2007.05.004. PMID 17678761.
- 1 2 van der Heijden, RA; Lankhorst, NE; van Linschoten, R; Bierma-Zeinstra, SM; van Middelkoop, M (20 January 2015). "Exercise for treating patellofemoral pain syndrome.". The Cochrane database of systematic reviews 1: CD010387. doi:10.1002/14651858.CD010387.pub2. PMID 25603546.
- ↑ van der Heijden, Rianne A; Lankhorst, Nienke E; van Linschoten, Robbart; Bierma-Zeinstra, Sita MA; van Middelkoop, Marienke; van Middelkoop, Marienke (2013). "Exercise for treating patellofemoral pain syndrome". Reviews. doi:10.1002/14651858.CD010387.
- 1 2 Putra, BE; Sutarina, N (2014). "Combination of hip‑quadriceps strengthening exercise: Is it more potential than single
conventional strengthening exercise to reduce pain in patellofemoral pain syndrome patients?". Saudi Journal of Sports Medicine 14 (1): 9–13. doi:10.4103/1319-6308.131579. line feed character in
|title=at position 88 (help) - ↑ Arendt, edited by Stefano Zaffagnini, David Dejour, Elizabeth A. (2010). Patellofemoral pain, instability, and arthritis clinical presentation, imaging, and treatment. Berlin: Springer. p. 134. ISBN 9783642054242.
- 1 2 3 Rodriguez-Merchan, EC (Mar 2014). "Evidence Based Conservative Management of Patello-femoral Syndrome.". Archives of bone and joint surgery 2 (1): 4–6. PMC 4151435. PMID 25207305.
- 1 2 American Medical Society for Sports Medicine (24 April 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Medical Society for Sports Medicine), retrieved 29 July 2014, which cites
- Rixe, JA; Glick, JE; Brady, J; Olympia, RP (Sep 2013). "A review of the management of patellofemoral pain syndrome.". The Physician and sportsmedicine 41 (3): 19–28. doi:10.3810/psm.2013.09.2023. PMID 24113699.
- ↑ Thomeé, R.; Renström, P.; Karlsson, J.; Grimby, G. (2007). "Patellofemoral pain syndrome in young women". Scandinavian Journal of Medicine & Science in Sports 5 (4): 237–44. doi:10.1111/j.1600-0838.1995.tb00040. PMID 7552769.
- ↑ Tria Jr, AJ; Palumbo, RC; Alicea, JA (1992). "Conservative care for patellofemoral pain". The Orthopedic clinics of North America 23 (4): 545–54. PMID 1408039.
- ↑ Gross, M. L.; Davlin, L. B.; Evanski, P. M. (1991). "Effectiveness of orthotic shoe inserts in the long-distance runner". The American Journal of Sports Medicine 19 (4): 409–12. doi:10.1177/036354659101900416. PMID 1897659.
- ↑ Eng, JJ; Pierrynowski, MR (1993). "Evaluation of soft foot orthotics in the treatment of patellofemoral pain syndrome". Physical therapy 73 (2): 62–8; discussion 68–70. PMID 8421719.
- ↑ Crossley, K; Bennell, K; Green, S; McConnell, J (April 2001). "A systematic review of physical interventions for patellofemoral pain syndrome.". Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine 11 (2): 103–10. doi:10.1097/00042752-200104000-00007. PMID 11403109.
- ↑ Bizzini, M; Childs, JD; Piva, SR; Delitto, A (Jan 2003). "Systematic review of the quality of randomized controlled trials for patellofemoral pain syndrome.". The Journal of orthopaedic and sports physical therapy 33 (1): 4–20. doi:10.2519/jospt.2003.33.7.F4. PMID 12570282.
External links
- Patellofemoral pain syndrome at DMOZ
- Patient handout for patellofemoral pain syndrome by the American Academy of Family Physicians
- Runner's Knee Prescribe Treatments for patellofemoral syndrome on PrescribeExercise.com
- Patellofemoral Pain Syndrome by the Institute for Physical and Sports Therapy
- Patellofemoral Joint Syndromes Treatment & Management at eMedicine
| ||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||