Pancreas
| Pancreas | |
|---|---|
 Anatomy of the pancreas | |
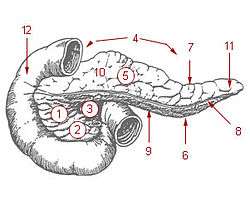 1: Head of pancreas 2: Uncinate process of pancreas 3: Pancreatic notch 4: Body of pancreas 5: Anterior surface of pancreas 6: Inferior surface of pancreas 7: Superior margin of pancreas 8: Anterior margin of pancreas 9: Inferior margin of pancreas 10: Omental tuber 11: Tail of pancreas 12: Duodenum | |
| Details | |
| Precursor | Pancreatic buds |
| Artery | Inferior pancreaticoduodenal artery, anterior superior pancreaticoduodenal artery, posterior superior pancreaticoduodenal artery, splenic artery |
| Vein | Pancreaticoduodenal veins, pancreatic veins |
| Nerve | Pancreatic plexus, celiac ganglia, vagus nerve[1] |
| Lymph | Splenic lymph nodes, celiac lymph nodes and superior mesenteric lymph nodes |
| Identifiers | |
| Latin | Pancreas |
| Greek | Pankrèous |
| MeSH | A03.734 |
| TA | A05.9.01.001 |
| FMA | 7198 |
The pancreas /ˈpæŋkriəs/ is a glandular organ in the digestive system and endocrine system of vertebrates. In humans, it is located in the abdominal cavity behind the stomach. It is an endocrine gland producing several important hormones, including insulin, glucagon, somatostatin, and pancreatic polypeptide which circulate in the blood. The pancreas is also a digestive organ, secreting pancreatic juice containing digestive enzymes that assist digestion and absorption of nutrients in the small intestine. These enzymes help to further break down the carbohydrates, proteins, and lipids in the chyme.
Structure
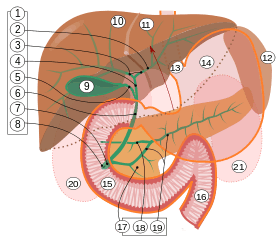
9. Gallbladder, 10–11. Right and left lobes of liver. 12. Spleen.
13. Esophagus. 14. Stomach. Small intestine: 15. Duodenum, 16. Jejunum
17. Pancreas: 18: Accessory pancreatic duct, 19: Pancreatic duct.
20–21: Right and left kidneys (silhouette).
The anterior border of the liver is lifted upwards (brown arrow). Gallbladder with Longitudinal section, pancreas and duodenum with frontal one. Intrahepatic ducts and stomach in transparency.
The pancreas is an endocrine organ that lies in the abdomen, specifically the upper left abdomen. It is found behind the stomach, with the head of the pancreas surrounded by the duodenum.[2] The pancreas is about 15 cm (6 in) long.[3]
Anatomically, the pancreas is divided into a head, which rests within the concavity of the duodenum, a body lying behind the base of the stomach, and a tail, which ends abutting the spleen. The neck of the pancreas lies between the body and head, and lies anterior to the superior mesenteric artery and vein. The head of the pancreas surrounds these two vessels, and a small uncinate process emerges from the lower part of the head, lying behind the superior mesenteric artery.[4]
The pancreas is a secretory structure with an internal hormonal role (endocrine) and an external digestive role (exocrine). It has two main ducts, the main pancreatic duct, and the accessory pancreatic duct. These drain enzymes through the ampulla of Vater into the duodenum.[5]
Margins
The upper margin of the pancreas is blunt and flat to the right; narrow and sharp to the left, near the tail.
It begins on the right in the omental tuber, and is in relation with the celiac artery, from which the hepatic artery courses to the right just above the gland, while the lienal artery runs toward the left in a groove along this border.
The lower margin of the pancreas separates the posterior from the inferior surface; the superior mesenteric vessels emerge under its right extremity.
The frontal margin of the pancreas separates the anterior from the inferior surface of the pancreas, and along this border the two layers of the transverse mesocolon diverge from one another; one passing upward over the frontal surface, the other backward over the inferior surface.
Surfaces
The inferior surface of the pancreas is narrow on the right but broader on the left, and is covered by peritoneum; it lies upon the duodenojejunal flexure and on some coils of the jejunum; its left extremity rests on the left colic flexure.
The anterior surface of the pancreas faces the front of the abdomen. Most of the right half of this surface is in contact with the transverse colon, with only areolar tissue intervening.
From its upper part it joins to the neck of the pancreas at a well-marked prominence, the omental tuber which abuts the lesser omentum. Its right edge is marked by a groove for the gastroduodenal artery.
The lower part of the right half, below the transverse colon, is covered by peritoneum continuous with the inferior layer of the transverse mesocolon, and is in contact with the coils of the small intestine.
The superior mesenteric artery passes down in front of the left half across the uncinate process; the superior mesenteric vein runs upward on the right side of the artery and, behind the neck, joins with the lienal vein to form the portal vein.
Blood supply
The pancreas receives blood from branches of both the coeliac artery and superior mesenteric artery. The splenic artery runs along the top margin of the pancreas, and supplies the neck, body and tail of the pancreas through its pancreatic branches, the largest of which is called the greater pancreatic artery. The superior pancreaticoduodenal artery and inferior pancreaticoduodenal artery runs along the anterior and posterior surfaces of the head of the pancreas at its border with the duodenum. These supply the head of the pancreas.[4]
The body and neck of the pancreas drain into the splenic vein; the head drains into the superior mesenteric and portal veins.[4]
Histology

The pancreas contains tissue with an endocrine and exocrine role, and this division is also visible when the pancreas is viewed under a microscope.[5]
The tissues with an endocrine role can be seen under staining as lightly-stained clusters of cells, called pancreatic islets (also called islets of Langerhans).[5]
Darker-staining cells form clusters called acini, which are arranged in lobes separated by a thin fibrous barrier. The secretory cells of each acinus surround a small intercalated duct. Because of their secretory function, these cells have many small granules of zymogens that are visible. The intercalated ducts drains into larger ducts within the lobule, and finally interlobular ducts. The ducts are lined by a single layer of columnar cells. With increasing diameter, several layers of columnar cells may be seen.[5]
Variation
The size of the pancreas varies considerably.[2] Several anatomical variations exist, relating to the embryological development of the two buds of the pancreas. The pancreas develops as two buds on either side of the duodenum. The ventral bud eventually rotates to lie next to the dorsal bud, eventually fusing. If the two buds do not fuse, a pancreas may exist as two separate lobes. This is also called pancreatic divisum. If the ventral bud does not fully rotate, an annular pancreas may exist. This is where sections of the pancreas completely encircle the duodenum, and may even lead to duodenal atresia.[4]
An accessory pancreatic duct may exist if the main duct of pancreas does not regress.[6]
Development
The pancreas forms from the embryonic foregut and is therefore of endodermal origin. Pancreatic development begins with the formation of a ventral and a dorsal pancreatic bud. Each structure communicates with the foregut through a duct. The dorsal pancreatic bud forms the head, body and tail, whereas the ventral pancreatic bud forms the uncinate process.[6]
Differential rotation and fusion of the ventral and dorsal pancreatic buds results in the formation of the definitive pancreas.[7] As the duodenum rotates to the right, it carries with it the ventral pancreatic bud and common bile duct. Upon reaching its final destination, the ventral pancreatic bud fuses with the much larger dorsal pancreatic bud. At this point of fusion, the main ducts of the ventral and dorsal pancreatic buds fuse, forming the main pancreatic duct. The duct of the dorsal bud regresses, leaving the main pancreatic duct.[6]
Differentiation of cells of the pancreas proceeds through two different pathways, corresponding to the dual endocrine and exocrine functions of the pancreas. In progenitor cells of the exocrine pancreas, important molecules that induce differentiation include follistatin, fibroblast growth factors, and activation of the Notch receptor system.[7] Development of the exocrine acini progresses through three successive stages. These are the predifferentiated, protodifferentiated, and differentiated stages, which correspond to undetectable, low, and high levels of digestive enzyme activity, respectively.
The multipotent pancreatic progenitor cells have the capacity to differentiate into all the pancreatic cells: acinar cells, endocrine cells, and ductal cells. These progenitor cells are characterised by the co-expression of the transcription factors PDX1 and NKX6-1. Under the influence of neurogenin-3 and ISL1, but in the absence of notch receptor signaling, these cells differentiate to form two lines of committed endocrine precursor cells. The first line, under the direction of a Pax gene, forms α- and γ- cells, which produce glucagon and pancreatic polypeptides, respectively. The second line, influenced by Pax-6, produces beta cells (β-) and delta cells (δ-), which secrete insulin and somatostatin, respectively.
Insulin and glucagon can be detected in the human fetal circulation by the fourth or fifth month of fetal development.[7]
Function
The pancreas is a dual-function gland, having features of both endocrine and exocrine glands.
Endocrine
The part of the pancreas with endocrine function is made up of approximately 3 million[8] cell clusters called pancreatic islets. These small micro organs are arranged along the pancreas in the form of density routes.[8] Four main cell types exist in the islets. They are relatively difficult to distinguish using standard staining techniques, but they can be classified by their secretion: α alpha cells secrete glucagon (increase glucose in blood), β beta cells secrete insulin (decrease glucose in blood), δ delta cells secrete somatostatin (regulates/stops α and β cells) and PP cells, or γ (gamma) cells, secrete pancreatic polypeptide.[9]
The islets are a compact collection of endocrine cells arranged in clusters and cords and are crisscrossed by a dense network of capillaries. The capillaries of the islets are lined by layers of endocrine cells in direct contact with vessels, and most endocrine cells are in direct contact with blood vessels, either by cytoplasmic processes or by direct apposition. According to the volume The Body, by Alan E. Nourse,[10] the islets are "busily manufacturing their hormone and generally disregarding the pancreatic cells all around them, as though they were located in some completely different part of the body." The pancreatic islets play an imperative role in glucose metabolism and regulation of blood glucose concentration.
Exocrine
The pancreas also functions as an exocrine gland that assists the digestive system. It secretes pancreatic fluid that contains digestive enzymes that pass to the small intestine. These enzymes help to further break down the carbohydrates, proteins and lipids (fats) in the chyme.
In humans, the secretory activity of the pancreas is regulated directly via the effect of hormones in the blood on the pancreatic islets and indirectly through the effect of the autonomic nervous system on the blood flow.[11]
The exocrine component of the pancreas, often called simply the exocrine pancreas, is the portion of the pancreas that performs exocrine functions. It has ducts that are arranged in clusters called acini (singular acinus). Pancreatic secretions are secreted into the lumen of the acinus, and then accumulate in intralobular ducts that drain to the main pancreatic duct, which drains directly into the duodenum.
Control of the exocrine function of the pancreas is via the hormones gastrin, cholecystokinin and secretin, which are secreted by cells in the stomach and duodenum, in response to distension and/or food and which cause secretion of pancreatic juices.
There are two main classes of exocrine pancreatic secretions:
| Secretion | Cell producing it | Primary signal |
| bicarbonate ions | Centroacinar cells | Secretin |
| digestive enzymes | Basophilic cells | CCK |
Pancreatic secretions from ductal cells contain bicarbonate ions and are alkaline in order to neutralize the acidic chyme that the stomach churns out.
The pancreas is also the main source of enzymes for digesting fats (lipids) and proteins. (The enzymes that digest polysaccharides, by contrast, are primarily produced by the walls of the intestines.)
The cells are filled with secretory granules containing the precursor digestive enzymes. The major proteases which the pancreas secretes are trypsinogen and chymotrypsinogen. Secreted to a lesser degree are pancreatic lipase and pancreatic amylase. The pancreas also secretes phospholipase A2, lysophospholipase, and cholesterol esterase.
The precursor enzymes (termed zymogens or proenzymes) are inactive variants of the enzymes; thus autodegradation, which can lead to pancreatitis, is avoided. Once released in the intestine, the enzyme enteropeptidase (formerly, and incorrectly, called enterokinase) present in the intestinal mucosa activates trypsinogen by cleaving it to form trypsin. The free trypsin then cleaves the rest of the trypsinogen, as well as chymotrypsinogen to its active form chymotrypsin.
Innervation
- Sympathetic (adrenergic)
- α2: decreases secretion from beta cells, increases secretion from alpha cells, β2: increases secretion from beta cells
- Parasympathetic (muscarinic)
- M3: increases stimulation of alpha cells and beta cells[12]
Clinical significance
A puncture of the pancreas, which may lead to the secretion of digestive enzymes such as lipase and amylase into the abdominal cavity as well as subsequent pancreatic self-digestion and digestion and damage to organs within the abdomen, generally requires prompt and experienced medical intervention.
It is possible for one to live without a pancreas, provided that the person takes insulin for proper regulation of blood glucose concentration and pancreatic enzyme supplements to aid digestion.[13]
Inflammation
Inflammation of the pancreas is known as pancreatitis. Pancreatitis is most often associated with recurrent gallstones or chronic alcohol use, although a variety of other causes, including measles, mumps, some medications, the congenital condition alpha-1 antitrypsin deficiency and even some scorpion stings, may cause pancreatitis. Pancreatitis is likely to cause intense pain in the central abdomen, that often radiates to the back, and may be associated with jaundice. In addition, due to causing problems with fat digestion and bilirubin excretion, pancreatitis often presents with pale stools and dark urine.[14]
In pancreatitis, enzymes of the exocrine pancreas damage the structure and tissue of the pancreas. Detection of some of these enzymes, such as amylase and lipase in the blood, along with symptoms and findings on X-ray, are often used to indicate that a person has pancreatitis. A person with pancreatitis is also at risk of shock. Pancreatitis is often managed medically with analgesics, removal of gallstones or treatment of other causes, and monitoring to ensure a patient does not develop shock.[14]
Cancer
Pancreatic cancers, particularly the most common type, pancreatic adenocarcinoma, remain very difficult to treat, and are mostly diagnosed only at a stage that is too late for surgery, which is the only curative treatment. Pancreatic cancer is rare in those younger than 40, and the median age of diagnosis is 71.[15] Risk factors include: smoking, obesity, diabetes, and certain rare genetic conditions including: multiple endocrine neoplasia type 1 and hereditary nonpolyposis colon cancer among others.[16] About 25% of cases are attributable to tobacco smoking,[17] while 5-10% of cases are linked to inherited genes.[15]
There are several types of pancreatic cancer, involving both the endocrine and exocrine tissue. Pancreatic adenocarcinoma, which affects the exocrine part of the pancreas, is by far the most common form. The many types of pancreatic endocrine tumors are all uncommon or rare, and have varied outlooks. However the incidence of these cancers has been rising sharply; it is not clear to what extent this reflects increased detection, especially through medical imaging, of tumors that would be very slow to develop. Insulinomas (largely benign) and gastrinomas are the most common types.[18] In the United States pancreatic cancer is the fourth most common cause of deaths due to cancer.[19] The disease occurs more often in the developed world, which had 68% of new cases in 2012.[20] Pancreatic adenocarcinoma typically has poor outcomes with the average percentage alive for at least one and five years after diagnosis being 25% and 5% respectively.[20][21] In localized disease where the cancer is small (< 2 cm) the number alive at five years is approximately 20%.[22] For those with neuroendocrine cancers the number alive after five years is much better at 65%, varying considerably with type.[20]
A solid pseudopapillary tumour is a low-grade malignant tumour of the pancreas of papillary architecture that typically afflicts young women.[23]
Diabetes
Type 1 diabetes
Diabetes mellitus type 1 is a chronic autoimmune disorder in which the immune system attacks the insulin-secreting cells of the pancreas. People with type 1 diabetes therefore lack the insulin needed to keep blood sugar levels within optimal ranges. If left untreated, this leads to high blood sugar and the array of associated symptoms. Type 1 diabetes develops in people of all ages but is most often diagnosed before adulthood. For type 1 diabetics, insulin injections are critical for survival.[24]
Type 2 diabetes
Diabetes mellitus type 2 is the most common form of diabetes. The causes for high blood sugar in this form of diabetes usually are a combination of insulin resistance and impaired insulin secretion, with both genetic and environmental factors playing an important role in the development of the disease. The management of type 2 diabetes relies on a series of changes in diet and physical activity with the purpose of reducing blood sugar levels to normal ranges and increasing insulin sensitivity.[24] Biguanides such as metformin are also used as part of the treatment along with insulin therapy.[25]
History
The pancreas was first identified for western civilization by Herophilus (335–280 BC), a Greek anatomist and surgeon. Only a few hundred years later, Rufus of Ephesus, another Greek anatomist, gave the pancreas its name. Etymologically, the term "pancreas", a modern Latin adaptation of Greek πάγκρεας,[26] [πᾶν ("all", "whole"), and κρέας ("flesh")],[27] originally means sweetbread,[28] although literally meaning all-flesh, presumably because of its fleshy consistency. It was only in 1889 when Oskar Minkowski discovered that removing the pancreas from a dog caused it to become diabetic (insulin was later discovered by Frederick Banting and Charles Herbert Best in 1921).
The organ is mentioned prominently in the 1992 film Encino Man. Pauly Shore's character Stoney often refers to the organ in unrelated contexts, perhaps demonstrating a fundamental misunderstanding of what the pancreas does.
Other animals
Pancreatic tissue is present in all vertebrate species, but its precise form and arrangement vary widely. There may be up to three separate pancreases, two of which arise from ventral buds, and the other dorsally. In most species (including humans), these fuse in the adult, but there are several exceptions. Even when a single pancreas is present, two or three pancreatic ducts may persist, each draining separately into the duodenum (or equivalent part of the foregut). Birds, for example, typically have three such ducts.[29]
In teleosts, and a few other species (such as rabbits), there is no discrete pancreas at all, with pancreatic tissue being distributed diffusely across the mesentery and even within other nearby organs, such as the liver or spleen. In a few teleost species, the endocrine tissue has fused to form a distinct gland within the abdominal cavity, but otherwise it is distributed among the exocrine components. The most primitive arrangement, however, appears to be that of lampreys and lungfish, in which pancreatic tissue is found as a number of discrete nodules within the wall of the gut itself, with the exocrine portions being little different from other glandular structures of the intestine.[29]
Gallery
-

The celiac artery and its branches; the stomach has been raised and the peritoneum removed
-

Lymphatics of stomach, etc., the stomach has been turned upward
-

Transverse section through the middle of the first lumbar vertebra, showing the relations of the pancreas
-

The duodenum and pancreas
-

Pancreas of a human embryo at end of sixth week
-
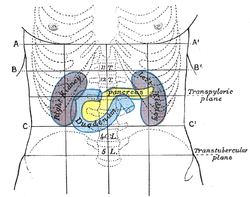
Front of abdomen, showing surface markings for duodenum, pancreas, and kidneys
-

Dog pancreas magnified 100 times
-

Pancreas
-

Pancreas
See also
This article incorporates text in the public domain from the 20th edition of Gray's Anatomy (1918)
- Sweetbread – pancreas as a food
References
- ↑ Physiology: 6/6ch2/s6ch2_30 - Essentials of Human Physiology
- 1 2 Khan, Ali Nawaz. "Chronic Pancreatitis Imaging". Medscape. Retrieved 5 January 2014.
- ↑ "Cancer of the Pancreas". NHS. Retrieved 5 November 2014.
- 1 2 3 4 Drake, Richard L.; Vogl, Wayne; Tibbitts, Adam W.M. Mitchell; illustrations by Richard; Richardson, Paul (2005). Gray's anatomy for students. Philadelphia: Elsevier/Churchill Livingstone. pp. 288–290, 297, 303. ISBN 978-0-8089-2306-0.
- 1 2 3 4 Young, Barbara, ed. (2006). Wheater's functional histology : a text and colour atlas (5th ed.). Churchill Livingstone/Elsevier. pp. 299–301. ISBN 978-0-443-06850-8.
- 1 2 3 Schoenwolf, Gary C. (2009). Larsen's human embryology (4th ed.). Philadelphia: Churchill Livingstone/Elsevier. pp. 241–244. ISBN 978-0-443-06811-9.
- 1 2 3 Carlson, Bruce M. (2004). Human embryology and developmental biology. St. Louis: Mosby. pp. 372–4. ISBN 0-323-01487-9.
- 1 2 3 Ionescu-Tirgoviste, Constantin; Gagniuc, Paul A.; Gubceac, Elvira; Mardare, Liliana; Popescu, Irinel; Dima, Simona; Militaru, Manuella (2015-09-29). "A 3D map of the islet routes throughout the healthy human pancreas". Scientific Reports 5: 14634. doi:10.1038/srep14634. PMC 4586491. PMID 26417671.
- ↑ BRS physiology 4th edition ,page 255-256, Linda S. Constanzo, Lippincott publishing
- ↑ The Body, by Alan E. Nourse, (op. cit., p. 171.)
- ↑ "New Research Redraws Pancreas Anatomy". 7 July 2011.
- ↑ Verspohl EJ, Tacke R, Mutschler E, Lambrecht G; Tacke; Mutschler; Lambrecht (1990). "Muscarinic receptor subtypes in rat pancreatic islets: binding and functional studies". Eur. J. Pharmacol. 178 (3): 303–311. doi:10.1016/0014-2999(90)90109-J. PMID 2187704.
- ↑ Banks, PA; Conwell, DL; Toskes, PP (2010). "The management of acute and chronic pancreatitis.". Gastroenterology & Hepatology 6 (2 Suppl 3): 1–16. PMC 2886461. PMID 20567557.
- 1 2 Britton, the editors Nicki R. Colledge, Brian R. Walker, Stuart H. Ralston ; illustrated by Robert (2010). Davidson's principles and practice of medicine. (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. pp. 871–874. ISBN 978-0-7020-3085-7.
- 1 2 Ryan DP, Hong TS, Bardeesy N; Hong; Bardeesy (September 2014). "Pancreatic adenocarcinoma". N. Engl. J. Med. 371 (11): 1039–49. doi:10.1056/NEJMra1404198. PMID 25207767.
- ↑ "Pancreatic Cancer Treatment (PDQ®) Patient Version". National Cancer Institute. 2014-04-17. Retrieved 8 June 2014.
- ↑ Wolfgang, CL; Herman, JM; Laheru, DA; Klein, AP; Erdek, MA; Fishman, EK; Hruban, RH (Sep 2013). "Recent progress in pancreatic cancer.". CA: a cancer journal for clinicians 63 (5): 319. doi:10.3322/caac.21190. PMC 3769458. PMID 23856911.
- ↑ Burns, WR; Edil, BH (March 2012). "Neuroendocrine pancreatic tumors: guidelines for management and update.". Current treatment options in oncology 13 (1): 24–34. doi:10.1007/s11864-011-0172-2. PMID 22198808.
- ↑ Hariharan D, Saied A, Kocher HM; Saied; Kocher (2008). "Analysis of mortality rates for pancreatic cancer across the world". HPB 10 (1): 58–62. doi:10.1080/13651820701883148. PMC 2504856. PMID 18695761.
- 1 2 3 World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.7. ISBN 9283204298.
- ↑ "American Cancer Society: Cancer Facts & Figures 2010: see page 4 for incidence estimates, and page 19 for survival percentages" (PDF).
- ↑ "Pancreatic Cancer Treatment (PDQ®) Health Professional Version". NCI. 2014-02-21. Retrieved 8 June 2014.
- ↑ Patil TB, Shrikhande SV, Kanhere HA, Saoji RR, Ramadwar MR, Shukla PJ (2006). "Solid pseudopapillary neoplasm of the pancreas: a single institution experience of 14 cases". HPB:the official journal of the International Hepato Pancreato Biliary Association 8 (2): 148–50. doi:10.1080/13651820510035721. PMC 2131425. PMID 18333264.
- 1 2 Melmed, S; Polonsky, KS; Larsen, PR; Kronenberg, HM (2011). Williams Textbook of Endocrinology (12th ed.). Saunders. ISBN 978-1437703245.
- ↑ Longo, D; Fauci, A; Kasper, D; Hauser, S; Jameson, J; Loscalzo, J (2012). Harrison's Principles of Internal Medicine (18th ed.). New York: McGraw-Hill. pp. 2995–3000. ISBN 978-0071748896.
- ↑ Terry O'Brien. A2Z Book of word Origins. Rupa Publications. p. 86. ISBN 978-81-291-1809-7.
- ↑ Harper, Douglas. "Pancreas". Online Etymology Dictionary. Retrieved 2007-04-04.
- ↑ Tamara M. Green (2008). The Greek and Latin Roots of English. Rowman & Littlefield. p. 176. ISBN 978-0-7425-4780-3.
- 1 2 Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, PA: Holt-Saunders International. pp. 357–359. ISBN 0-03-910284-X.
External links
-
 Media related to Pancreas at Wikimedia Commons
Media related to Pancreas at Wikimedia Commons
| ||||||||||||||||||||
|
