Metamizole
 | |
 | |
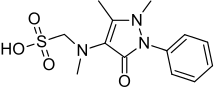
| Systematic (IUPAC) name | |
|---|---|
|
[(2,3-dihydro-1,5-dimethyl-3-oxo-2-phenyl-1H-pyrazol-4-yl)methylamino] methanesulfonic acid | |
| Clinical data | |
| Trade names | Originally Novalgin,[1] now generic[2] |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category |
|
| Legal status |
|
| Routes of administration | Oral, IM, IV, rectal |
| Pharmacokinetic data | |
| Bioavailability | 100% (active metabolites)[5] |
| Protein binding | 48%-58% (active metabolites)[5] |
| Metabolism | Liver[5] |
| Biological half-life | 14 minutes (parent compound; parenteral);[4] metabolites: 2–4 hours[5] |
| Excretion | Urine (96%, IV; 85%, oral), faeces (4%, IV).[4] |
| Identifiers | |
| CAS Number | 68-89-3 (sodium salt) |
| ATC code | N02BB02 |
| PubChem |
CID 80254 CID 3111 |
| DrugBank |
DB04817 |
| ChemSpider | 3000 |
| UNII |
VSU62Z74ON |
| ChEBI |
CHEBI:59033 |
| ChEMBL |
CHEMBL487894 |
| Chemical data | |
| Formula | C13H17N3O4S |
| Molar mass | 311.357 g/mol |
| |
| |
| (verify) | |
Metamizole (INN), or dipyrone (BAN, USAN), is an ampyrone sulfonate analgesic (pain reliever), antispasmodic (spasm reliever) and antipyretic (fever reducer) similar to paracetamol in that it has minimal anti-inflammatory effects and which is most commonly given orally or parenterally (by injection) to prevent and treat pain related to surgery or for the treatment of acute pain.[4][5] It was first introduced into clinical use in Germany in 1922 under the brandname "Novalgin" and for many years it was available over-the-counter in most countries, until its toxicities became apparent,[6] although in some countries it is available over-the-counter, its use is usually restricted in developed countries, due to its potential for causing toxic reactions.[7]
Metamizole is marketed under various trade names.[2][3]
Despite its potential haematologic (blood-related) toxicity (that is potential for causing blood dyscrasias) it produces no clinically relevant effects in the way of kidney toxicity, cardiovascular toxicity and GI toxicity when compared to non-steroidal anti-inflammatory drugs (NSAIDs).[5] Unlike paracetamol and similarly to the NSAIDs it can trigger bronchospasm or anaphylaxis, especially in those with asthma.[7]
Medical uses
It is primarily used for perioperative pain, although the clinical trial data to support this use is limited at best.[7] It is also used for acute injury, colic, cancer pain, other acute/chronic forms of pain and high fever unresponsive to other agents.[4]
Special populations
Its use in pregnancy is advised against, although animal studies are reassuring in that they show minimal risk of birth defects; its use in the elderly or those with liver/kidney impairment is advised against, but if these groups of people must be treated a lower dose and caution is usually advised; its use in lactation is advised against as it is excreted in breast milk.[4]
Adverse effects
It is known to cause minimal side effects in most people given it; serious side effects include agranulocytosis, aplastic anaemia, hypersensitivity reactions (like anaphylaxis and bronchospasm), toxic epidermal necrolysis and it may provoke acute attacks of porphyria, as it is chemically related to sulfonamides.[3][5][7] The relative risk for agranulocytosis appears to greatly vary according to the country of estimates on said rate and opinion on the risk is strongly divided.[3][8]
Contraindications
Previous hypersensitivity (such as agranulocytosis or anaphylaxis) to metamizole or any of the excipients (e.g. lactose) in the preparation used, acute porphyria, impaired haematopoiesis (such as due to treatment with chemotherapy agents), third trimester of pregnancy (potential for adverse effects in the newborn), lactation, children with a body weight below 16 kg, history of aspirin-induced asthma and other hypersensitivity reactions to analgesics.[4]
| Drug(s) | Interaction/reason for theoretical potential for interaction |
|---|---|
| Ciclosporin | Decreased serum levels of ciclosporin. |
| Chlorpromazine | Additive hypothermia (low body temperature) may result. |
| Methotrexate | Additive risk for haematologic (blood) toxicity. |
Oral anticoagulants (blood thinners), lithium, captopril, triamterene and antihypertensives may also interact with metamizole, as other pyrazolones are known to interact adversely with these substances.
Overdose
It is considered fairly safe on overdose, but in these cases supportive measures are usually advised as well as measures to limit absorption (such as activated charcoal) and accelerate excretion (such as haemodialysis).[4]
Physicochemistry
It is a sulfonic acid and comes in calcium, sodium and magnesium salt forms.[3] Its sodium salt monohydrate form is a white/almost crystalline powder that is unstable in the presence of light, highly soluble in water and ethanol but practically insoluble in dichloromethane[9]
Pharmacology
Its precise mechanism of action is unknown, although it is believed that inhibiting brain and spinal cord prostaglandin (fat-like molecules that are involved in inflammation, pain and fever) synthesis might be involved.[7] Recently, researchers uncovered another potential mechanism involving metamizole being a prodrug. In this proposal, not yet verified by other researchers, the metamizole itself breaks down into other chemicals that are the actual active agents. The result is a couple of cannabinoid and NSAID arachidonic acid conjugates (although not in the strict chemical meaning of the word) of metamizole's breakdown products.[10] Despite this studies in animals have found that the first cannabinoid receptor is not involved in the analgesia induced by metamizole.[11] Although it seems to inhibit fevers caused by prostaglandins, especially prostaglandin E2.[12] It appears to produce its therapeutic effects by means of its metabolites, especially N-methyl-4-aminoantipyrine (MAA) and 4-aminoantipyrine (AA).[4]
| Metabolite | Acronym | Biologically active? | Pharmacokinetic properties |
|---|---|---|---|
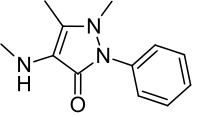 N-methyl-4-aminoantipyrine | MAA | Yes | Bioavailability≈90%. Plasma protein binding: 58%. Excreted in the urine as 3±1% of the initial (oral) dose |
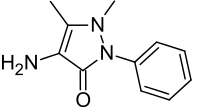 4-aminoantipyrine | AA | Yes | Bioavailability≈22.5%. Plasma protein binding: 48%. Excreted in the urine as 6±3% of the initial (oral) dose |
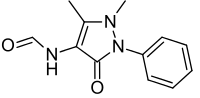 N-formyl-4-aminoantipyrine | FAA | No | Plasma protein binding: 18%. Excretion in the urine as 23±4% of the initial oral dose |
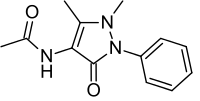 N-acetyl-4-aminoantipyrine | AAA | No | Plasma protein binding: 14%. Excretion in the urine as 26±8% of the initial oral dose |
History
Ludwig Knorr was a student of Emil Fischer who won the Nobel Prize for his work on purines and sugars, which included the discovery of phenylhydrazine.[1][13] In the 1880s, Knorr was trying to make quinolone derivatives from phenylhydrazine, and instead made a pyrazole derivative, which after a methylation, he made into phenazone, also called antipyrine, which has been called "the 'mother' of all modern antipyretic analgesics."[1][14]:26–27 Sales of that drug exploded, and in the 1890s chemists at Teerfarbenfabrik Meister, Lucius & Co. (a precursor of Hoechst AG which is now Sanofi), made another derivative called pyramidon which was three times more active than antipyrine.[1]
In 1893, a derivative of antipyrine, aminopyrine, was made by Friedrich Stolz at Hoechst.[14]:26–27 Yet later, chemists at Hoechst made a derivative, melubrine (sodium antipyrine aminomethanesulfonate), which was introduced in 1913,[15] and yet later metamizole was synthesized; metamilzole is a methyl derivative of melubrine and is also a more soluble prodrug of pyramidon.[1][14]:26–27 Metamizole was first marketed as "Novalgin" in 1922.[1][16]:86
Metamizole had strong worldwide sales up until the 1970s, but there had been reports of agranulocytosis in the literature since the 1930s.[16]:91 In the 1970s AMA Drug Evaluations and other formularies called attention to these events and warned physicians against liberal use of metamizole, and the drug was banned in several countries.[16]:91 International controversy became heated in the 1970s and 1980s, especially with regard to marketing of the drug in the developing world, where agranulocytosis was difficult to manage and usually led to death, unlike in the developed world, where patients could generally be saved.[16]:92
One difficulty in determining the risk of agranulocytosis was the lack of consistent epidemiological data; estimates ranged from 9 cases per 1000 uses to 2 cases per 10 million uses, and there was no known mechanism of toxicity.[16]:92 Hoechst commissioned a study of the drug to get better data, which published in JAMA in 1986.[16]:94[17] The study reported wildly inconsistent country-to-country variation in agranulocytosis and only intensified the controversy with supporters of the drug finding vindication and critics now additionally angry over the conduct of the study.[16]:94–97 As of 2014 the safety of the drug remained controversial.[8]
Society and culture
Legal status
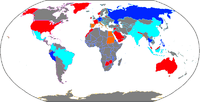
Metamizole is banned completely in several countries, available by prescription in others (sometimes with strong warnings, sometimes without them), and available over the counter in yet others, based on the judgement of regulators of the risk of drug-induced agranulocytosis and the level of development of the regulatory system.[6][8][18][19] For example, it is not available in the US, but is recommended and used as a first line treatment for postoperative pain in Germany.[6][8]
Brand names
Metamizole is generic, and in countries where it is marketed, it is available under many brand names.[2]
References
- 1 2 3 4 5 6 Brune, K (1997). "The early history of non-opioid analgesics". Acute Pain 1: 33. doi:10.1016/S1366-0071(97)80033-2.
- 1 2 3 Drugs.com Drugs.com international listings for Metamizole Page accessed June 21, 2015
- 1 2 3 4 5 Brayfield, A, ed. (13 December 2013). "Dipyrone". Martindale: The Complete Drug Reference. Pharmaceutical Press. Retrieved 19 April 2014.
- 1 2 3 4 5 6 7 8 9 10 11 "Fachinformation (Zusammenfassung der Merkmale des Arzneimittels) Novaminsulfon injekt 1000 mg Lichtenstein Novaminsulfon injekt 2500 mg Lichtenstein". Winthrop Arzneimittel GmbH (in German). Zinteva Pharm GmbH. February 2013. Retrieved 19 April 2014.
- 1 2 3 4 5 6 7 Jage, J; Laufenberg-Feldmann, R; Heid, F (20 March 2008). "Medikamente zur postoperativen Schmerztherapie: Bewährtes und Neues" [Drugs for postoperative analgesia: routine and new aspects. Part 1: non-opioids]. Der Anaesthesist (in German) 57 (4): 382–390. doi:10.1007/s00101-008-1326-x. PMID 18351305.
- 1 2 3 4 United Nations Department of Economic and Social Affairs (2005). Consolidated List of Products Whose Consumption and/or Sale Have Been Banned, Withdrawn, Severely Restricted of Not Approved by Governments (PDF) (12th ed.). New York: United Nations. pp. 171–5. Retrieved 3 April 2013.
- 1 2 3 4 5 Brack, A; Rittner, HL; Schäfer, M (March 2004). "Nichtopioidanalgetika zur perioperativen Schmerztherapie" [Non-opioid analgesics for perioperative pain therapy. Risks and rational basis for use]. Der Anaesthesist (in German) 53 (3): 263–80. doi:10.1007/s00101-003-0641-5. PMID 15021958.
- 1 2 3 4 Pogatzki-Zahn E, Chandrasena C, Schug SA. Nonopioid analgesics for postoperative pain management. Curr Opin Anaesthesiol. 2014 Oct;27(5):513-9. PMID 25102238
- ↑ Council of Europe; Council of Europe. European Directorate for the Quality of Medicines & HealthCare (EDQM); Rada Europy; European Pharmacopoeia Commission; European Directorate for the Quality of Medicines & Healthcare (2013). European Pharmacopoeia: Published in Accordance with the Convention on the Elaboration of a European Pharmacopoeia (European Treaty Series No. 50). Council of Europe. ISBN 978-92-871-7527-4.
- ↑ Jasiecka, A; Maślanka, T; Jaroszewski, JJ (2014). "Pharmacological characteristics of metamizole". Polish Journal of Veterinary Sciences 17 (1): 207–14. doi:10.2478/pjvs-2014-0030. PMID 24724493.
- ↑ Elmas, P; Ulugol, A (November 2013). "Involvement of cannabinoid CB1 receptors in the antinociceptive effect of dipyrone". Journal of Neural Transmission 120 (11): 1533–8. doi:10.1007/s00702-013-1052-7. PMID 23784345.
- ↑ Malvar, DD; Aguiar, FA; Vaz, AD; Assis, DC; de Melo, MC; Jabor, VA; Kalapothakis,, E; Ferreira, SH; Clososki, GC; de Souza, GE (April 2014). "The dipyrone metabolite 4-MAA induces hypothermia and inhibits PGE2-dependent and -independent fever while 4-AA only blocks PGE2 -dependent fever". British Journal of Pharmacology 171 (15): 3666–79. doi:10.1111/bph.12717. PMID 24712707.
- ↑ Nobel Committee Emil Fischer - Biographical
- 1 2 3 Enrique Ravina. The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. John Wiley & Sons, 2011 ISBN 9783527326693
- ↑ New and Nonofficial Remedies: Melubrine. JAMA 61(11):869. 1913
- 1 2 3 4 5 6 7 Silverman M et al. Bad Medicine: The Prescription Drug Industry in the Third World. Stanford University Press, 1992 ISBN 9780804766678
- ↑ The International Agranulocytosis and Aplastic Anemia Study. Risks of agranulocytosis and aplastic anemia. A first report of their relation to drug use with special reference to analgesics. JAMA 256(13) 1749-1757 PMID 3747087
- ↑ Department of Economic and Social Affairs of the United Nations Secretariat Consolidated List of Products Whose Consumption and/or Sale Have Been Banned, Withdrawn, Severely Restricted or not Approved by Governments Fourteenth Issue (New data only) (January 2005 – October 2008): Pharmaceuticals United Nations – New York, 2009
- ↑ Rogosch, T; Sinning, C; Podlewski, A; Watzer, B; Schlosburg, J; Lichtman, AH; Cascio, MG; Bisogno, T; Di Marzo, V; Nüsing, R; Imming, P (January 2012). "Novel bioactive metabolites of dipyrone (metamizol)" (PDF). Bioorganic & Medicinal Chemistry 20 (1): 101–7. doi:10.1016/j.bmc.2011.11.028. PMC 3248997. PMID 22172309.
| ||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||