Estrogen
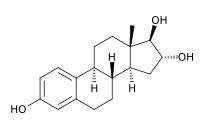
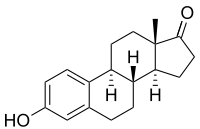
Estrogen or oestrogen (see spelling differences) is the primary female sex hormone and is responsible for development and regulation of the female reproductive system and secondary sex characteristics. Estrogen may also refer to any substance, natural or synthetic, that mimics the effects of the natural hormone.[1] The steroid 17β-estradiol is the most potent and prevalent endogenous estrogen, although several metabolites of estradiol also have estrogenic hormonal activity. Synthetic estrogens are used as part of some oral contraceptives, in estrogen replacement therapy for postmenopausal women, and in hormone replacement therapy for trans women.
The name estrogen comes from the Greek οἶστρος (oistros), literally meaning "verve or inspiration" but figuratively sexual passion or desire,[2] and the suffix -gen, meaning "producer of".
Estrogens are synthesized in all vertebrates[3] as well as some insects.[4] Their presence in both vertebrates and insects suggests that estrogenic sex hormones have an ancient evolutionary history. The three major naturally occurring forms of estrogen in women are estrone (E1), estradiol (E2), and estriol (E3). Another type of estrogen called estetrol (E4) is produced only during pregnancy. Quantitatively, estrogens circulate at lower levels than androgens in both men and women.[5] While estrogen levels are significantly lower in males compared to females, estrogens nevertheless also have important physiological roles in males.[6]
Like all steroid hormones, estrogens readily diffuse across the cell membrane. Once inside the cell, they bind to and activate estrogen receptors (ERs) which in turn modulate the expression of many genes.[7] Additionally, estrogens bind to and activate rapid-signaling membrane estrogen receptors (mERs),[8][9] such as GPER (GPR30).[10]
Types
Steroidal
Endogenous
The three major naturally occurring estrogens in women are estrone (E1), estradiol (E2), and estriol (E3). Estradiol is the predominant estrogen during reproductive years both in terms of absolute serum levels as well as in terms of estrogenic activity. During menopause, estrone is the predominant circulating estrogen and during pregnancy estriol is the predominant circulating estrogen in terms of serum levels. Though estriol is the most plentiful of the three estrogens it is also the weakest, whereas estradiol is the strongest with a potency of approximately 80 times that of estriol.[11] Thus, estradiol is the most important estrogen in non-pregnant females who are between the menarche and menopause stages of life. However, during pregnancy this role shifts to estriol, and in postmenopausal women estrone becomes the primary form of estrogen in the body. Another type of estrogen called estetrol (E4) is produced only during pregnancy. All of the different forms of estrogen are synthesized from androgens, specifically testosterone and androstenedione, by the enzyme aromatase.
Other endogenous estrogens, which are notably not biosynthesized by aromatase, include 27-hydroxycholesterol, dehydroepiandrosterone (DHEA), 7-oxo-DHEA, 7α-hydroxy-DHEA, 16α-hydroxy-DHEA, 7β-hydroxyepiandrosterone, Δ4-androstenedione, Δ5-androstenediol, 3α-androstanediol, and 3β-androstanediol, and have important endogenous functions as estrogens.[12][13]
Some metabolites of estrone, such as 2-hydroxyestrone and 16-hydroxyestrone, are also weak estrogens.
Pharmaceuticals
Estradiol, estrone, and estriol have all been approved as pharmaceutical drugs and are used medically. Estetrol is currently under development for medical indications, but has not yet been approved in any country.
A variety of synthetic estrogen esters, such as estradiol cypionate, estradiol valerate, estradiol acetate, and estradiol benzoate, are used clinically. The aforementioned compounds behave as prodrugs to estradiol, and are longer-lasting in comparison. Esters of estrone and estriol also exist and are employed in clinical medicine.
Ethinyl estradiol (EE) is a more potent synthetic analogue of estradiol that is used widely in hormonal contraceptives. Mestranol, moxestrol, and quinestrol are derivatives of EE used clinically. A related drug is methylestradiol, which is also used clinically.
Conjugated equine estrogens (CEEs), such as Premarin, a commonly prescribed estrogenic drug produced from the urine of pregnant mares, include the natural steroidal estrogens equilin and equilenin, as well as, especially, estrone sulfate (which itself is inactive and becomes active upon conversion into estrone). A related and very similar product to CEEs is esterified estrogens (EEs).
Testosterone, which is available as a pharmaceutical drug, is metabolized in part to estrogens such as estradiol, and can produce significant estrogenic effects at high dosages, most notably gynecomastia in males. The same is true for various synthetic anabolic steroids.
DHEA is available over-the-counter as a dietary supplement, though it is not very estrogenic.

Non-steroidal
Diethylstilbestrol is a non-steroidal estrogen that is no longer used medically. It is a member of the stilbestrol group. Other stilbestrol estrogens that have been used clinically include benzestrol, dienestrol, dienestrol acetate, diethylstilbestrol dipropionate, fosfestrol, hexestrol, and methestrol dipropionate.
Chlorotrianisene, methallenestril, and doisynoestrol are non-steroidal estrogens structurally-distinct from the stilbestrols that have also been used clinically.
A range of synthetic and natural substances have been identified in the environment that possess estrogenic activity.[14]
- Synthetic substances of this kind are known as xenoestrogens.
- Plant products with estrogenic activity are called phytoestrogens.
- Those produced by fungi are known as mycoestrogens.
Unlike estrogens produced by mammals, these substances are not necessarily steroids.
Antiestrogens
Antiestrogens are antagonists of the estrogen receptor (ER). Selective estrogen receptor modulators (SERMs) are partial agonists of the ER, and have estrogenic and antiestrogenic effects in different tissues. Examples of SERMs include tamoxifen, clomifene, and raloxifene. Fulvestrant is a silent antagonist of the ER.
Biosynthesis

Estrogens, in females, are produced primarily by the ovaries, and during pregnancy, the placenta. Follicle-stimulating hormone (FSH) stimulates the ovarian production of estrogens by the granulosa cells of the ovarian follicles and corpora lutea. Some estrogens are also produced in smaller amounts by other tissues such as the liver, adrenal glands, and the breasts. These secondary sources of estrogens are especially important in postmenopausal women. Fat cells produce estrogen as well.[15]
In females, synthesis of estrogens starts in theca interna cells in the ovary, by the synthesis of androstenedione from cholesterol. Androstenedione is a substance of weak androgenic activity which serves predominantly as a precursor for more potent androgens such as testosterone as well as estrogen. This compound crosses the basal membrane into the surrounding granulosa cells, where it is converted either immediately into estrone, or into testosterone and then estradiol in an additional step. The conversion of androstenedione to testosterone is catalyzed by 17β-hydroxysteroid dehydrogenase (17β-HSD), whereas the conversion of androstenedione and testosterone into estrone and estradiol, respectively is catalyzed by aromatase, enzymes which are both expressed in granulosa cells. In contrast, granulosa cells lack 17α-hydroxylase and 17,20-lyase, whereas theca cells express these enzymes and 17β-HSD but lack aromatase. Hence, both granulosa and theca cells are essential for the production of estrogen in the ovaries.
Estrogen levels vary through the menstrual cycle, with levels highest near the end of the follicular phase just before ovulation.
Function
The actions of estrogen are mediated by the estrogen receptor (ER), a dimeric nuclear protein that binds to DNA and controls gene expression. Like other steroid hormones, estrogen enters passively into the cell where it binds to and activates the estrogen receptor. The estrogen:ER complex binds to specific DNA sequences called a hormone response element to activate the transcription of target genes (in a study using an estrogen-dependent breast cancer cell line as model, 89 such genes were identified).[16] Since estrogen enters all cells, its actions are dependent on the presence of the ER in the cell. The ER is expressed in specific tissues including the ovary, uterus and breast. The metabolic effects of estrogen in postmenopausal women has been linked to the genetic polymorphism of the ER.[17]
While estrogens are present in both men and women, they are usually present at significantly higher levels in women of reproductive age. They promote the development of female secondary sexual characteristics, such as breasts, and are also involved in the thickening of the endometrium and other aspects of regulating the menstrual cycle. In males, estrogen regulates certain functions of the reproductive system important to the maturation of sperm[18][19][20] and may be necessary for a healthy libido.[21] Furthermore, there are several other structural changes induced by estrogen in addition to other functions.
- Structural
- Promote formation of female secondary sex characteristics
- Accelerate metabolism
- Increase fat store
- Stimulate endometrial growth
- Increase uterine growth
- Increase vaginal lubrication
- Thicken the vaginal wall
- Maintenance of vessel and skin
- Reduce bone resorption, increase bone formation
- Protein synthesis
- Increase hepatic production of binding proteins
- Coagulation
- Increase circulating level of factors 2, 7, 9, 10, plasminogen
- Decrease antithrombin III
- Increase platelet adhesiveness
- Lipid
- Increase HDL, triglyceride
- Decrease LDL, fat deposition
- Fluid balance
- Gastrointestinal tract
- Reduce bowel motility
- Increase cholesterol in bile
- Melanin
- Increase pheomelanin, reduce eumelanin
- Cancer
- Support hormone-sensitive breast cancers (see section below)
- Lung function
- Uterus lining
- Estrogen together with progesterone promotes and maintains the uterus lining in preparation for implantation of fertilized egg and maintenance of uterus function during gestation period, also upregulates oxytocin receptor in myometrium
- Ovulation
- Surge in estrogen level induces the release of luteinizing hormone, which then triggers ovulation by releasing the egg from the Graafian follicle in the ovary.
- Sexual receptivity in estrus
- Promotes sexual receptivity,[23] and induces lordosis behavior.[24] In non-human mammals, it also induces estrus (in heat) prior to ovulation, which also induces lordosis behavior. Female non-human mammals are not sexually receptive without the estrogen surge, i.e., they have no mating desire when not in estrus.
- Lordosis behavior
- Regulates the stereotypical sexual receptivity behavior; this lordosis behavior is estrogen-dependent, which is regulated by the ventromedial nucleus of the hypothalamus.[25]
- Sexual desire
- Sex drive is dependent on androgen levels[26] only in the presence of estrogen, but without estrogen, free testosterone level actually decreases sexual desire (instead of increases sex drive), as demonstrated for those women who have hypoactive sexual desire disorder, and the sexual desire in these women can be restored by administration of estrogen (using oral contraceptive).[27] In non-human mammals, mating desire is triggered by estrogen surge in estrus.
Fetal development
In rodents, estrogens (which are locally aromatized from androgens in the brain) play an important role in psychosexual differentiation, for example, by masculinizing territorial behavior;[28] the same is not true in humans.[29] In humans, the masculinizing effects of prenatal androgens on behavior (and other tissues, with the possible exception of effects on bone) appear to act exclusively through the androgen receptor.[30] Consequently, the utility of rodent models for studying human psychosexual differentiation has been questioned.[31]
Breast development
Estrogen, in conjunction with growth hormone (GH) and its secretory product insulin-like growth factor 1 (IGF-1), is critical in mediating breast development during puberty, as well as breast maturation during pregnancy in preparation of lactation and breastfeeding.[32][33] Estrogen is primarily and directly responsible for inducing the ductal component of breast development,[34][35][36] as well as for causing fat deposition and connective tissue growth.[34][35] It is also indirectly involved in the lobuloalveolar component, by increasing progesterone receptor expression in the breasts[34][36][37] and by inducing the secretion of prolactin.[38][39] Allowed for by estrogen, progesterone and prolactin work together to complete lobuloalveolar development during pregnancy.[35][40]
Androgens such as testosterone powerfully oppose estrogen action in the breasts, such as by reducing estrogen receptor expression in them.[41][42]
Heart disease
Women suffer less from heart disease due to vasculo-protective action of estrogen which helps in preventing atherosclerosis.[43] It also helps in maintaining the delicate balance between fighting infections and protecting arteries from damage thus lowering the risk of cardiovascular disease.[44]
Immunological role
Estrogen has anti-inflammatory properties and helps in mobilization of polymorphonuclear white blood cells or neutrophils.[44]
Cognition
Verbal memory scores are frequently used as one measure of higher level cognition. These scores vary in direct proportion to estrogen levels throughout the menstrual cycle, pregnancy, and menopause. Furthermore estrogens when administered shortly after natural or surgical menopause prevents decreases in verbal memory. In contrast, estrogens have little effect on verbal memory if first administered years after menopause.[45] Estrogens also have positive influences on other measures of cognitive function.[46] However the effect of estrogens on cognition is not uniformly favorable and is dependent on the timing of the dose and the type of cognitive skill being measured.[47]
The protective effects of estrogens on cognition may be mediated by estrogens anti-inflammatory effects in the brain.[48]
Mental health
Estrogen is considered to play a significant role in women’s mental health. Sudden estrogen withdrawal, fluctuating estrogen, and periods of sustained estrogen low levels correlate with significant mood lowering. Clinical recovery from postpartum, perimenopause, and postmenopause depression has been shown to be effective after levels of estrogen were stabilized and/or restored.[49][50][51]
Compulsions in male lab mice, such as those in obsessive-compulsive disorder (OCD), may be caused by low estrogen levels. When estrogen levels were raised through the increased activity of the enzyme aromatase in male lab mice, OCD rituals were dramatically decreased. Hypothalamic protein levels in the gene COMT are enhanced by increasing estrogen levels which are believed to return mice that displayed OCD rituals to normal activity. Aromatase deficiency is ultimately suspected which is involved in the synthesis of estrogen in humans and has therapeutic implications in humans having obsessive-compulsive disorder.[52]
Local application of estrogen in the rat hippocampus has been shown to inhibit the re-uptake of serotonin. Contrarily, local application of estrogen has been shown to block the ability of fluvoxamine to slow serotonin clearance, suggesting that the same pathways which are involved in SSRI efficacy may also be affected by components of local estrogen signaling pathways.[53]
Binge eating
Estrogen may play a role in suppressing binge eating. Hormone replacement therapy using estrogen may be a possible treatment for binge eating behaviors in females. Estrogen replacement has been shown to suppress binge eating behaviors in female mice.[54] The mechanism by which estrogen replacement inhibits binge-like eating involves the replacement of serotonin (5-HT) neurons. Women exhibiting binge eating behaviors are found to have increased brain uptake of neuron 5-HT, and therefore less of the neurotransmitter serotonin in the cerebrospinal fluid.[55] Estrogen works to activate 5-HT neurons, leading to suppression of binge like eating behaviors.[54]
It is also suggested that there is an interaction between hormone levels and eating at different points in the female menstrual cycle. Research has predicted increased emotional eating during hormonal flux, which is characterized by high progesterone and estradiol levels that occur during the mid-luteal phase. It is hypothesized that these changes occur due to brain changes across the menstrual cycle that are likely a genomic effect of hormones. These effects produce menstrual cycle changes, which result in hormone release leading to behavioral changes, notably binge and emotional eating. These occur especially prominently among women who are genetically vulnerable to binge eating phenotypes.[56]
Binge eating is associated with decreased estradiol and increased progesterone.[57] Klump et al.[58] Progesterone may moderate the effects of low estradiol (such as during dysregulated eating behavior), but that this may only be true in women who have had clinically diagnosed binge episodes (BEs). Dysregulated eating is more strongly associated with such ovarian hormones in women with BEs than in women without BEs.[58]
The implantation of 17β-estradiol pellets in ovariectomized mice significantly reduced binge eating behaviors and injections of GLP-1 in ovariectomized mice decreased binge-eating behaviors.[54]
The associations between binge eating, menstrual-cycle phase and ovarian hormones correlated.[57][59][59][60]
Medical applications
Oral contraceptives
Since estrogen circulating in the blood can negatively feed-back to reduce circulating levels of FSH and LH, most oral contraceptives contain a synthetic estrogen, along with a synthetic progestin. Even in men, the major hormone involved in LH feedback is estradiol, not testosterone.[61][62]
Hormone replacement therapy
Estrogen and other hormones are given to postmenopausal women in order to prevent osteoporosis as well as treat the symptoms of menopause such as hot flushes, vaginal dryness, urinary stress incontinence, chilly sensations, dizziness, fatigue, irritability, and sweating. Fractures of the spine, wrist, and hips decrease by 50–70% and spinal bone density increases by ~5% in those women treated with estrogen within 3 years of the onset of menopause and for 5–10 years thereafter.
Before the specific dangers of conjugated equine estrogens were well understood, standard therapy was 0.625 mg/day of conjugated equine estrogens (such as Premarin). There are, however, risks associated with conjugated equine estrogen therapy. Among the older postmenopausal women studied as part of the Women's Health Initiative (WHI), an orally administered conjugated equine estrogen supplement was found to be associated with an increased risk of dangerous blood clotting. The WHI studies used one type of estrogen supplement, a high oral dose of conjugated equine estrogens (Premarin alone and with medroxyprogesterone acetate as PremPro).[63]
In a study by the NIH, esterified estrogens were not proven to pose the same risks to health as conjugated equine estrogens. Hormone replacement therapy has favorable effects on serum cholesterol levels, and when initiated immediately upon menopause may reduce the incidence of cardiovascular disease, although this hypothesis has yet to be tested in randomized trials. Estrogen appears to have a protector effect on atherosclerosis: it lowers LDL and triglycerides, it raises HDL levels and has endothelial vasodilatation properties plus an anti-inflammatory component.
Research is underway to determine if risks of estrogen supplement use are the same for all methods of delivery. In particular, estrogen applied topically may have a different spectrum of side-effects than when administered orally,[64] and transdermal estrogens do not affect clotting as they are absorbed directly into the systemic circulation, avoiding first-pass metabolism in the liver. This route of administration is thus preferred in women with a history of thrombo-embolic disease.
Estrogen is also used in the therapy of vaginal atrophy, hypoestrogenism (as a result of hypogonadism, castration, or primary ovarian failure), amenorrhea, dysmenorrhea, and oligomenorrhea. Estrogens can also be used to suppress lactation after child birth.
Breast cancer
About 80% of breast cancers, once established, rely on supplies of the hormone estrogen to grow: they are known as hormone-sensitive or hormone-receptor-positive cancers. Suppression of production of estrogen in the body is a treatment for these cancers.
Research suggests the common table mushroom has anti-aromatase[65] properties and therefore possible anti-estrogen activity. In 2009, a case-control study of the eating habits of 2,018 women in southeast China revealed that women who consumed greater than 10 grams of fresh mushrooms or greater than 4 grams of dried mushrooms per day had an approximately 50% lower incidence of breast cancer. Chinese women who consumed mushrooms and green tea had a 90% lower incidence of breast cancer.[66] However the study was relatively small (2,018 patients participating) and limited to Chinese women of southeast China.
Hormone-receptor-positive breast cancers are treated with drugs which suppress production or interfere with the action of estrogen in the body.[67] This technique, in the context of treatment of breast cancer, is known variously as hormonal therapy, hormone therapy, or anti-estrogen therapy (not to be confused with hormone replacement therapy). Certain foods such as soy may also suppress the proliferative effects of estrogen and are used as an alternative to hormone therapy.[68]
Prostate cancer
Under certain circumstances, estrogen may also be used in males for treatment of prostate cancer.[69]
Miscellaneous
In humans and mice, estrogen promotes wound healing.[70]
At one time, estrogen was used to induce growth attenuation in tall girls.[71] Recently, estrogen-induced growth attenuation was used as part of the controversial Ashley Treatment to keep a developmentally disabled girl from growing to adult size.[72]
Most recently, estrogen has been used in experimental research as a way to treat women suffering from bulimia nervosa, in addition to cognitive behavioral therapy, which is the established standard for treatment in bulimia cases. The estrogen research hypothesizes that the disease may be linked to a hormonal imbalance in the brain.[73]
Estrogen has also been used in studies which indicate that it may be an effective drug for use in the treatment of traumatic liver injury.[74]
Health risks and warning labels
Hyperestrogenism (elevated levels of estrogen) may be a result of exogenous administration of estrogen or estrogen-like substances, or may be a result of physiologic conditions such as pregnancy. Any of these causes is linked with an increase in the risk of thrombosis.[75]
The estrogen-alone substudy of the WHI reported an increased risk of stroke and deep vein thrombosis (DVT) in postmenopausal women 50 years of age or older and an increased risk of dementia in postmenopausal women 65 years of age or older using 0.625 mg of Premarin conjugated equine estrogens (CEE). The estrogen-plus-progestin substudy of the WHI reported an increased risk of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli and DVT in postmenopausal women 50 years of age or older and an increased risk of dementia in postmenopausal women 65 years of age or older using PremPro, which is 0.625 mg of CEE with 2.5 mg of the progestin medroxyprogesterone acetate (MPA).[76][77][78]
The labeling of estrogen-only products in the U.S. includes a boxed warning that unopposed estrogen (without progestogen) therapy increases the risk of endometrial cancer. Based on a review of data from the WHI, on January 8, 2003 the FDA changed the labeling of all estrogen and estrogen with progestin products for use by postmenopausal women to include a new boxed warning about cardiovascular and other risks.
Cosmetics
Some hair shampoos on the market include estrogens and placental extracts; others contain phytoestrogens. In 1998, there were case reports of four prepubescent African-American girls developing breasts after exposure to these shampoos.[79] In 1993, the FDA determined that not all over-the-counter topically applied hormone-containing drug products for human use are generally recognized as safe and effective and are misbranded. An accompanying proposed rule deals with cosmetics, concluding that any use of natural estrogens in a cosmetic product makes the product an unapproved new drug and that any cosmetic using the term "hormone" in the text of its labeling or in its ingredient statement makes an implied drug claim, subjecting such a product to regulatory action.[80]
In addition to being considered misbranded drugs, products claiming to contain placental extract may also be deemed to be misbranded cosmetics if the extract has been prepared from placentas from which the hormones and other biologically active substances have been removed and the extracted substance consists principally of protein. The FDA recommends that this substance be identified by a name other than "placental extract" and describing its composition more accurately because consumers associate the name "placental extract" with a therapeutic use of some biological activity.[80]
History
In 1929 Adolf Butenandt and Edward Adelbert Doisy independently isolated and determined the structure of estrogen.[81] Thereafter, the pace of hormonal drug research accelerated.
The "first orally effective estrogen", Emmenin, derived from the late-pregnancy urine of Canadian women, was introduced in 1930 by Collip and Ayerst Laboratories. Estrogens are not water-soluble and cannot be given orally, but the urine was found to contain estriol glucuronide, which is water-soluble and becomes active in the body after hydrolysis.
Scientists continued to search for new sources of estrogen because of concerns associated with the practicality of introducing the drug into the market. At the same time, a German pharmaceutical drug company, formulated a similar product as Emmenin that was introduced to German women to treat menopausal symptoms.
In 1938, British scientists obtained a patent on a newly formulated nonsteroidal estrogen, diethylstilbestrol (DES), that was cheaper and more powerful than the previously manufactured estrogens. Soon after, concerns over the side effects of DES were raised in scientific journals while the drug manufacturers came together to lobby for governmental approval of DES. It was only until 1941 when estrogen therapy was finally approved by the Food and Drug Administration (FDA) for the treatment of menopausal symptoms.[82]
Environmental effects
Estrogens are among the wide range of endocrine-disrupting compounds (EDCs) because they have high estrogenic potency. When an EDC makes its way into the environment, it may cause male reproductive dysfunction to wildlife.[83] The estrogen excreted from farm animals makes its way into fresh water systems.[84] During the germination period of reproduction the fish are exposed to low levels of estrogen which may cause reproductive dysfunction to male fish.[85][86]
See also
- Antiestrogen
- Estrogen insensitivity syndrome
- Aromatase deficiency
- Aromatase excess syndrome
- Aromatase inhibitor
- Atrophic vaginitis
- Endocrine disruptor
- List of steroid abbreviations
- Sexual motivation and hormones
References
- ↑ "estrogen (CHEBI:50114)". ChEBI. Retrieved 15 July 2015.
- ↑ "Greek Word Study Tool: oistros". Perseus Digital Library. Retrieved 2011-12-28.
- ↑ Ryan KJ (August 1982). "Biochemistry of aromatase: significance to female reproductive physiology". Cancer Res. 42 (8 Suppl): 3342s–3344s. PMID 7083198.
- ↑ Mechoulam R, Brueggemeier RW, Denlinger DL (September 2005). "Estrogens in insects" (PDF). Cellular and Molecular Life Sciences 40 (9): 942–944. doi:10.1007/BF01946450.
- ↑ Burger HG (2002). "Androgen production in women". Fertility and Sterility. 77 Suppl 4: S3–5. doi:10.1016/S0015-0282(02)02985-0. PMID 12007895.
- ↑ Lombardi G, Zarrilli S, Colao A, Paesano L, Di Somma C, Rossi F, De Rosa M (2001). "Estrogens and health in males". Molecular and Cellular Endocrinology 178 (1-2): 51–5. doi:10.1016/S0303-7207(01)00420-8. PMID 11403894.
- ↑ Whitehead SA, Nussey S (2001). Endocrinology: an integrated approach. Oxford: BIOS: Taylor & Francis. ISBN 1-85996-252-1.
- ↑ Soltysik K, Czekaj P (April 2013). "Membrane estrogen receptors - is it an alternative way of estrogen action?". J. Physiol. Pharmacol. 64 (2): 129–42. PMID 23756388.
- ↑ Micevych PE, Kelly MJ (2012). "Membrane estrogen receptor regulation of hypothalamic function". Neuroendocrinology 96 (2): 103–10. doi:10.1159/000338400. PMC 3496782. PMID 22538318.
- ↑ Prossnitz ER, Arterburn JB, Sklar LA (2007). "GPR30: A G protein-coupled receptor for estrogen". Mol. Cell. Endocrinol. 265–266: 138–42. doi:10.1016/j.mce.2006.12.010. PMC 1847610. PMID 17222505.
- ↑ Files JA, Ko MG, Pruthi S (2011). "Bioidentical hormone therapy". Mayo Clin. Proc. 86 (7): 673–80, quiz 680. doi:10.4065/mcp.2010.0714. PMC 3127562. PMID 21531972.
- ↑ Baker ME (2013). "What are the physiological estrogens?". Steroids 78 (3): 337–40. doi:10.1016/j.steroids.2012.12.011. PMID 23313336.
- ↑ Miller KK, Al-Rayyan N, Ivanova MM, Mattingly KA, Ripp SL, Klinge CM, Prough RA (2013). "DHEA metabolites activate estrogen receptors alpha and beta". Steroids 78 (1): 15–25. doi:10.1016/j.steroids.2012.10.002. PMC 3529809. PMID 23123738.
- ↑ Fang H, Tong W, Shi LM, Blair R, Perkins R, Branham W, Hass BS, Xie Q, Dial SL, Moland CL, Sheehan DM (2001). "Structure-activity relationships for a large diverse set of natural, synthetic, and environmental estrogens". Chem. Res. Toxicol. 14 (3): 280–94. doi:10.1021/tx000208y. PMID 11258977.
- ↑ Nelson LR, Bulun SE (September 2001). "Estrogen production and action". J. Am. Acad. Dermatol. 45 (3 Suppl): S116–24. doi:10.1067/mjd.2001.117432. PMID 11511861.
- ↑ Lin CY, Ström A, Vega VB, Kong SL, Yeo AL, Thomsen JS, Chan WC, Doray B, Bangarusamy DK, Ramasamy A, Vergara LA, Tang S, Chong A, Bajic VB, Miller LD, Gustafsson JA, Liu ET (2004). "Discovery of estrogen receptor alpha target genes and response elements in breast tumor cells". Genome Biol. 5 (9): R66. doi:10.1186/gb-2004-5-9-r66. PMC 522873. PMID 15345050.
- ↑ Darabi M, Ani M, Panjehpour M, Rabbani M, Movahedian A, Zarean E (2011). "Effect of estrogen receptor β A1730G polymorphism on ABCA1 gene expression response to postmenopausal hormone replacement therapy". Genet Test Mol Biomarkers 15 (1-2): 11–5. doi:10.1089/gtmb.2010.0106. PMID 21117950.
- ↑ Raloff J (December 6, 1997). "Science News Online (12/6/97): Estrogen's Emerging Manly Alter Ego". Science News. Retrieved 2008-03-04.
- ↑ Hess RA, Bunick D, Lee KH, Bahr J, Taylor JA, Korach KS, Lubahn DB (1997). "A role for estrogens in the male reproductive system". Nature 390 (6659): 447–8. doi:10.1038/37352. PMID 9393999.
- ↑ "Science Blog – Estrogen Linked To Sperm Count, Male Fertility". Science Blog. Retrieved 2008-03-04.
- ↑ Hill RA, Pompolo S, Jones ME, Simpson ER, Boon WC (2004). "Estrogen deficiency leads to apoptosis in dopaminergic neurons in the medial preoptic area and arcuate nucleus of male mice". Mol. Cell. Neurosci. 27 (4): 466–76. doi:10.1016/j.mcn.2004.04.012. PMID 15555924.
- ↑ Massaro D, Massaro GD (December 2004). "Estrogen regulates pulmonary alveolar formation, loss, and regeneration in mice". Am. J. Physiol. Lung Cell Mol. Physiol. 287 (6): L1154–9. doi:10.1152/ajplung.00228.2004. PMID 15298854.
- ↑ Christensen A, Dewing P, Micevych P (November 2011). "Membrane-initiated estradiol signaling induces spinogenesis required for female sexual receptivity". J Neurosci. 31 (48): 17583–17589. doi:10.1523/JNEUROSCI.3030-11.2011. PMID 22131419.
- ↑ Handa RJ, Ogawa S, Wang JM, Herbison AE (January 2012). "Roles for oestrogen receptor β in adult brain function". J Neuroendocrinol. 24 (1): 160–173. doi:10.1111/j.1365-2826.2011.02206.x. PMC 3348521. PMID 21851428.
- ↑ Kow LM, Pfaff DW (May 1998). "Mapping of neural and signal transduction pathways for lordosis in the search for estrogen actions on the central nervous system". Behav. Brain Res. 92 (2): 169–180. doi:10.1016/S0166-4328(97)00189-7. PMID 9638959.
- ↑ Warnock JK, Swanson SG, Borel RW, Zipfel LM, Brennan JJ (2005). "Combined esterified estrogens and methyltestosterone versus esterified estrogens alone in the treatment of loss of sexual interest in surgically menopausal women". Menopause 12 (4): 359–60. doi:10.1097/01.GME.0000153933.50860.FD. PMID 16037752.
- ↑ Heiman JR, Rupp H, Janssen E, Newhouse SK, Brauer M, Laan E (May 2011). "Sexual desire, sexual arousal and hormonal differences in premenopausal US and Dutch women with and without low sexual desire". Horm Behav. 59 (5): 772–779. doi:10.1016/j.yhbeh.2011.03.013. PMID 21514299.
- ↑ Wu MV, Manoli DS, Fraser EJ, Coats JK, Tollkuhn J, Honda S, Harada N, Shah NM (October 2009). "Estrogen masculinizes neural pathways and sex-specific behaviors". Cell 139 (1): 61–72. doi:10.1016/j.cell.2009.07.036. PMC 2851224. PMID 19804754.
- ↑ Rochira V, Carani C (October 2009). "Aromatase deficiency in men: a clinical perspective". Nature Reviews Endocrinology 5 (10): 559–68. doi:10.1038/nrendo.2009.176. PMID 19707181.
- ↑ Wilson JD (September 2001). "Androgens, androgen receptors, and male gender role behavior". Horm Behav 40 (2): 358–66. doi:10.1006/hbeh.2001.1684. PMID 11534997.
- ↑ Baum MJ (November 2006). "Mammalian animal models of psychosexual differentiation: when is 'translation' to the human situation possible?". Horm Behav 50 (4): 579–88. doi:10.1016/j.yhbeh.2006.06.003. PMID 16876166.
- ↑ Brisken C, O'Malley B (2010). "Hormone action in the mammary gland". Cold Spring Harb Perspect Biol 2 (12): a003178. doi:10.1101/cshperspect.a003178. PMC 2982168. PMID 20739412.
- ↑ Kleinberg DL (1998). "Role of IGF-I in normal mammary development". Breast Cancer Res. Treat. 47 (3): 201–8. doi:10.1023/a:1005998832636. PMID 9516076.
- 1 2 3 Johnson LR (2003). Essential Medical Physiology. Academic Press. p. 770. ISBN 978-0-12-387584-6.
- 1 2 3 Norman AW, Henry HL (30 July 2014). Hormones. Academic Press. p. 311. ISBN 978-0-08-091906-5.
- 1 2 Coad J, Dunstall M (2011). Anatomy and Physiology for Midwives,with Pageburst online access,3: Anatomy and Physiology for Midwives. Elsevier Health Sciences. p. 413. ISBN 0-7020-3489-4.
- ↑ Haslam SZ, Osuch JR (1 January 2006). Hormones and Breast Cancer in Post-Menopausal Women. IOS Press. p. 69. ISBN 978-1-58603-653-9.
- ↑ Silbernagl S, Despopoulos A (1 January 2011). Color Atlas of Physiology. Thieme. pp. 305–. ISBN 978-3-13-149521-1.
- ↑ Fadem B (2007). High-yield Comprehensive USMLE Step 1 Review. Lippincott Williams & Wilkins. pp. 445–. ISBN 978-0-7817-7427-7.
- ↑ Blackburn S (14 April 2014). Maternal, Fetal, & Neonatal Physiology. Elsevier Health Sciences. pp. 146–. ISBN 978-0-323-29296-2.
- ↑ Strauss JF, Barbieri RL (13 September 2013). Yen and Jaffe's Reproductive Endocrinology. Elsevier Health Sciences. pp. 236–. ISBN 978-1-4557-2758-2.
- ↑ Wilson CB, Nizet V, Maldonado Y, Remington JS, Klein JO (24 February 2015). Remington and Klein's Infectious Diseases of the Fetus and Newborn Infant. Elsevier Health Sciences. pp. 190–. ISBN 978-0-323-24147-2.
- ↑ Rosano GM, Panina G (1999). "Oestrogens and the heart". Therapie 54 (3): 381–5. PMID 10500455.
- 1 2 Nadkarni S, Cooper D, Brancaleone V, Bena S, Perretti M (November 2011). "Activation of the annexin A1 pathway underlies the protective effects exerted by estrogen in polymorphonuclear leukocytes". Arterioscler. Thromb. Vasc. Biol. 31 (11): 2749–59. doi:10.1161/ATVBAHA.111.235176. PMC 3357483. PMID 21836070.
- ↑ Sherwin BB (2012). "Estrogen and cognitive functioning in women: lessons we have learned". Behavioral Neuroscience 126 (1): 123–7. doi:10.1037/a0025539. PMID 22004260.
- ↑ Hara Y, Waters EM, McEwen BS, Morrison JH (2015). "Estrogen Effects on Cognitive and Synaptic Health Over the Lifecourse". Physiological Reviews 95 (3): 785–807. doi:10.1152/physrev.00036.2014. PMID 26109339.
- ↑ Korol DL, Pisani SL (2015). "Estrogens and cognition: Friends or foes?: An evaluation of the opposing effects of estrogens on learning and memory". Hormones and Behavior 74: 105–15. doi:10.1016/j.yhbeh.2015.06.017. PMID 26149525.
- ↑ Au A, Feher A, McPhee L, Jessa A, Oh S, Einstein G (2016). "Estrogens, inflammation and cognition". Frontiers in Neuroendocrinology. doi:10.1016/j.yfrne.2016.01.002. PMID 26774208.
- ↑ Douma SL, Husband C, O'Donnell ME, Barwin BN, Woodend AK (2005). "Estrogen-related mood disorders: reproductive life cycle factors". Advances in Nursing Science 28 (4): 364–75. doi:10.1097/00012272-200510000-00008. PMID 16292022.
- ↑ Osterlund MK, Witt MR, Gustafsson JA (2005). "Estrogen action in mood and neurodegenerative disorders: estrogenic compounds with selective properties-the next generation of therapeutics". Endocrine 28 (3): 235–42. doi:10.1385/ENDO:28:3:235. PMID 16388113.
- ↑ Lasiuk GC, Hegadoren KM (October 2007). "The effects of estradiol on central serotonergic systems and its relationship to mood in women". Biol Res Nurs 9 (2): 147–60. doi:10.1177/1099800407305600. PMID 17909167.
- ↑ Hill RA, McInnes KJ, Gong EC, Jones ME, Simpson ER, Boon WC (February 2007). "Estrogen deficient male mice develop compulsive behavior". Biol. Psychiatry 61 (3): 359–66. doi:10.1016/j.biopsych.2006.01.012. PMID 16566897.
- ↑ Benmansour S, Weaver RS, Barton AK, Adeniji OS, Frazer A (April 2012). "Comparison of the effects of estradiol and progesterone on serotonergic function". Biol. Psychiatry 71 (7): 633–41. doi:10.1016/j.biopsych.2011.11.023. PMC 3307822. PMID 22225849.
- 1 2 3 Cao X, Xu P, Oyola MG, Xia Y, Yan X, Saito K, Zou F, Wang C, Yang Y, Hinton A, Yan C, Ding H, Zhu L, Yu L, Yang B, Feng Y, Clegg DJ, Khan S, DiMarchi R, Mani SK, Tong Q, Xu Y (2014). "Estrogens stimulate serotonin neurons to inhibit binge-like eating in mice". J. Clin. Invest. 124 (10): 4351–62. doi:10.1172/JCI74726. PMC 4191033. PMID 25157819.
- ↑ Jimerson DC, Lesem MD, Kaye WH, Hegg AP, Brewerton TD (1990). "Eating disorders and depression: is there a serotonin connection?". Biol. Psychiatry 28 (5): 443–54. doi:10.1016/0006-3223(90)90412-u. PMID 2207221.
- ↑ Klump KL, Keel PK, Racine SE, Burt SA, Burt AS, Neale M, Sisk CL, Boker S, Hu JY (2013). "The interactive effects of estrogen and progesterone on changes in emotional eating across the menstrual cycle". J Abnorm Psychol 122 (1): 131–7. doi:10.1037/a0029524. PMC 3570621. PMID 22889242.
- 1 2 Edler C, Lipson SF, Keel PK (2007). "Ovarian hormones and binge eating in bulimia nervosa". Psychol Med 37 (1): 131–41. doi:10.1017/S0033291706008956. PMID 17038206.
- 1 2 Klump KL, Racine SE, Hildebrandt B, Burt SA, Neale M, Sisk CL, Boker S, Keel PK (2014). "Ovarian Hormone Influences on Dysregulated Eating: A Comparison of Associations in Women with versus without Binge Episodes". Clin Psychol Sci 2 (4): 545–559. doi:10.1177/2167702614521794. PMID 25343062.
- 1 2 Klump KL, Keel PK, Culbert KM, Edler C (2008). "Ovarian hormones and binge eating: exploring associations in community samples". Psychol Med 38 (12): 1749–57. doi:10.1017/S0033291708002997. PMC 2885896. PMID 18307829.
- ↑ Lester NA, Keel PK, Lipson SF (2003). "Symptom fluctuation in bulimia nervosa: relation to menstrual-cycle phase and cortisol levels". Psychol Med 33 (1): 51–60. doi:10.1017/s0033291702006815. PMID 12537036.
- ↑ "Proluton Depot 250 mg". PharmaOffshore.com. Pharma Offshore. Retrieved 15 July 2015.
- ↑ "Heal Yourself At Home". Heal Yourself At Home. Retrieved 15 July 2015.
- ↑ "NIH – Menopausal Hormone Therapy Information". National Institutes of Health. August 27, 2007. Retrieved 2008-03-04.
- ↑ Menon DV, Vongpatanasin W (2006). "Effects of transdermal estrogen replacement therapy on cardiovascular risk factors". Treat Endocrinol 5 (1): 37–51. doi:10.2165/00024677-200605010-00005. PMID 16396517.
- ↑ Chen S, Kao YC, Laughton CA (1997). "Binding characteristics of aromatase inhibitors and phytoestrogens to human aromatase". J. Steroid Biochem. Mol. Biol. 61 (3-6): 107–15. doi:10.1016/S0960-0760(97)80001-5. PMID 9365179.
- ↑ Zhang M, Huang J, Xie X, Holman CD (March 2009). "Dietary intakes of mushrooms and green tea combine to reduce the risk of breast cancer in Chinese women". Int. J. Cancer 124 (6): 1404–8. doi:10.1002/ijc.24047. PMID 19048616.
- ↑ "Hormonal Therapy". breastcancer.org. July 26, 2007. Retrieved 2008-03-04.
- ↑ Kurzer MS (2002). "Hormonal effects of soy in premenopausal women and men". J. Nutr. 132 (3): 570S–573S. PMID 11880595.
- ↑ Oh WK (2002). "The evolving role of estrogen therapy in prostate cancer". Clin Genitourinary Cancer 1 (2): 81–9. doi:10.3816/CGC.2002.n.009. PMID 15046698.
- ↑ Oh DM, Phillips, TJ (2006). "Sex Hormones and Wound Healing". Wounds 18 (1): 8–18.
- ↑ Lee JM, Howell JD (2006). "Tall girls: the social shaping of a medical therapy". Arch Pediatr Adolesc Med 160 (10): 1077–8. doi:10.1001/archpedi.160.10.1035. PMID 17018462.
- ↑ Gunther DF, Diekema DS (2006). "Attenuating growth in children with profound developmental disability: a new approach to an old dilemma". Arch Pediatr Adolesc Med 160 (10): 1013–7. doi:10.1001/archpedi.160.10.1013. PMID 17018459.
- ↑ Andersson G (January 9, 2007). "Bulimia May Result from Hormonal Imbalance". Karolinska Institutet. Retrieved 2008-03-04.
- ↑ Hsieh YC, Yu HP, Frink M, Suzuki T, Choudhry MA, Schwacha MG, Chaudry IH (2007). "G protein-coupled receptor 30-dependent protein kinase A pathway is critical in nongenomic effects of estrogen in attenuating liver injury after trauma-hemorrhage". Am. J. Pathol. 170 (4): 1210–8. doi:10.2353/ajpath.2007.060883. PMC 1829455. PMID 17392161.
- ↑ Mitchell RS, Kumar V, Robbins SL, Abbas AK, Fausto N (2007). "4". Robbins basic pathology (8th ed.). Saunders/Elsevier. ISBN 1-4160-2973-7.
- ↑ FDA (January 8, 2003). "FDA Approves New Labels for Estrogen and Estrogen with Progestin Therapies for Postmenopausal Women Following Review of Women's Health Initiative Data". Archived from the original on December 21, 2007. Retrieved 2006-10-26.
- ↑ Kolata G (2003-01-09). "F.D.A. Orders Warning on All Estrogen Labels". The New York Times. Retrieved 2006-10-26.
- ↑ NLM (2006-04-01). "IMPORTANT WARNING". Drug Information: Estrogen. MedlinePlus. Archived from the original on 2006-10-09. Retrieved 2006-10-26.
- ↑ Sanghavi DM (2006-10-17). "Preschool Puberty, and a Search for the Causes". The New York Times. Retrieved 2008-06-04.
- 1 2 FDA (February 1995). "Products containing estrogenic hormones, placental extract or vitamins". Guide to Inspections of Cosmetic Product Manufacturers. Archived from the original on October 14, 2007. Retrieved 2006-10-24.
- ↑ Tata JR (2005). "One hundred years of hormones". EMBO Reports 6 (6): 490–6. doi:10.1038/sj.embor.7400444. PMC 1369102. PMID 15940278.
- ↑ Rothenberg, Carla J. (April 25, 2005). "The Rise and Fall of Estrogen Therapy: The History of HRT" (PDF). Retrieved 2006-10-27.
- ↑ Wang S, Huang W, Fang G, Zhang Y, Qiao H (2008). "Analysis of steroidal estrogen residues in food and environmental samples". International Journal of Environmental Analytical Chemistry 88 (1): 1–25. doi:10.1080/03067310701597293.
- ↑ Wise A, O'Brien K, Woodruff T (October 2011). "Are Oral Contraceptives a Significant Contributor to the Estrogenicity of Drinking Water?". Environ Sci Technol 45 (1): 51–60. doi:10.1021/es1014482. PMID 20977246. Lay summary – Chemical & Engineering News.
- ↑ Liney KE, Jobling S, Shears JA, Simpson P, Tyler CR (October 2005). "Assessing the sensitivity of different life stages for sexual disruption in roach (Rutilus rutilus) exposed to effluents from wastewater treatment works". Environ. Health Perspect. 113 (10): 1299–307. doi:10.1289/ehp.7921. PMC 1281270. PMID 16203238.
- ↑ Jobling S, Williams R, Johnson A, Taylor A, Gross-Sorokin M, Nolan M, Tyler CR, van Aerle R, Santos E, Brighty G (April 2006). "Predicted exposures to steroid estrogens in U.K. rivers correlate with widespread sexual disruption in wild fish populations". Environ. Health Perspect. 114 Suppl 1 (Suppl 1): 32–9. doi:10.1289/ehp.8050. PMC 1874167. PMID 16818244.
External links
- MedlinePlus DrugInfo medmaster-a682922
- Estrogens - Lab Tests Online
- Nussey and Whitehead: Endocrinology, an integrated approach, Taylor and Francis 2001. Free online textbook.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||