Nissen fundoplication
| Nissen fundoplication | |
|---|---|
| Intervention | |
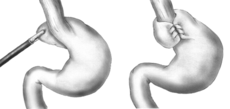 Diagram of a Nissen fundoplication. | |
| ICD-9-CM | 44.66, 44.67 |
Nissen fundoplication, sometimes known as laparoscopic fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD it is usually performed when medical therapy has failed, but with paraesophageal hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal (270° anterior), Belsey (270° anterior transthoracic), Dor (anterior 180-200°), Lind (300° posterior), and Toupet fundoplications (posterior 270°) are alternative procedures with somewhat different indications and outcomes.[1]
History
Dr. Rudolph Nissen (1896–1981) first performed the procedure in 1955 and published the results of two cases in a 1956 Swiss Medical Weekly.[2] In 1961 he published a more detailed overview of the procedure.[3] Nissen originally called the surgery "gastroplication." The procedure has borne his name since it gained popularity in the 1970s.[4]
Technique
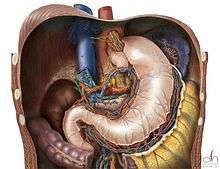
In a fundoplication, the gastric fundus (upper part) of the stomach is wrapped, or plicated, around the lower end of the esophagus and stitched in place, reinforcing the closing function of the lower esophageal sphincter. The esophageal hiatus is also narrowed down by sutures to prevent or treat concurrent hiatal hernia, in which the fundus slides up through the enlarged esophageal hiatus of the diaphragm.
In a Nissen fundoplication, also called a complete fundoplication, the fundus is wrapped all the way 360 degrees around the esophagus. In contrast, surgery for achalasia is generally accompanied by either a Dor or Toupet partial fundoplication, which is less likely than a Nissen wrap to aggravate the dysphagia that characterizes achalasia. In a Dor (anterior) fundoplication, the fundus is laid over the top of the esophagus; while in a Toupet (posterior) fundoplication, the fundus is wrapped around the back of the esophagus.
The procedure is now routinely performed laparoscopically. When used to alleviate gastroesophageal reflux symptoms in patients with delayed gastric emptying, it is frequently combined with modification of the pylorus via pyloromyotomy or pyloroplasty.
Mechanism of relief
Whenever the stomach contracts, it also closes off the esophagus instead of squeezing stomach acids into it. This prevents the reflux of gastric acid (in GERD). Although antacids and PPI drug therapy can reduce the effects of reflux acid, successful surgical treatment has the advantage of eliminating drug side-effects and damaging effects from other components of reflux such as bile or gastric contents.[1]
Complications
Nissen (complete) fundoplication is generally considered to be safe and effective, with a mortality rate of less than 1% and many of the most common post-operative complications minimized or eliminated by the partial fundoplication procedures now more commonly used. Studies have shown that after 10 years, 89.5% of patients are still symptom-free.[5]
Complications include "gas bloat syndrome", dysphagia (trouble swallowing), dumping syndrome, excessive scarring, vagus nerve injury, and rarely, achalasia.[6] The fundoplication can also come undone over time in about 5-10% of cases, leading to recurrence of symptoms. If the symptoms warrant a repeat surgery, the surgeon may use Marlex or another form of artificial mesh to strengthen the connection.[7] Postoperative irritable bowel syndrome, which lasts for roughly 2 weeks, is possible.
In "gas bloat syndrome", fundoplication can alter the mechanical ability of the stomach to eliminate swallowed air by belching, leading to an accumulation of gas in the stomach or small intestine. Data varies, but some degree of gas-bloat may occur in as many as 41% of Nissen patients; whereas the occurrence is less with patients undergoing partial anterior fundoplication.[8] Gas bloat syndrome is usually self-limiting within 2 to 4 weeks, but in some it may persist. The offending gas may also come from dietary sources (especially carbonated beverages), or involuntary swallowing of air (aerophagia). If postoperative gas-bloat syndrome does not resolve with time, dietary restrictions, counselling regarding aerophagia, and correction – either by endoscopic balloon dilatation or repeat surgery to revise the Nissen fundoplication to a partial fundoplication – may be necessary.[8]
Vomiting is sometimes impossible or, if not, very painful after a fundoplication with the likelihood of this complication typically decreasing in the months after surgery. In some cases, the purpose of this operation is to correct excessive vomiting. However, when its purpose is to reduce gastric reflux, difficulty in vomiting may be an undesired outcome. Initially, vomiting is impossible; however, small amounts of vomit may be produced after the wrap settles over time, and in extreme cases such as alcohol poisoning or food poisoning, the patient may be able to vomit freely with some amount of pain. Outcomes have improved in recent years, especially at the most skilled and successful clinics.
References
- 1 2 Renee C. Minjarez, M.D. and Blair A. Jobe, M.D. (2006). "[Surgical therapy for gastroesophageal reflux disease.]". GI Motility online. doi:10.1038/gimo56.
- ↑ Nissen R (1956). "[A Simple Operation for Control of Reflux Esophagitis.]". Schweizerische Medizinische Wochenschrift (in German) 86 (Suppl 20): 590–2. PMID 13337262.
- ↑ Nissen R (1961). "Gastropexy and "Fundoplication" in Surgical Treatment of Hiatal Hernia". The American Journal of Digestive Diseases 6 (10): 954–61. doi:10.1007/BF02231426. PMID 14480031.
- ↑ Stylopoulos N, Rattner DW; Rattner (2005). "The History of Hiatal Hernia surgery: From Bowditch to Laparoscopy". Ann. Surg. 241 (1): 185–93. PMC 1356862. PMID 15622007.
- ↑ Minjarez, RC; Jobe BA. "Surgical therapy for gastroesophageal reflux disease". GI Motility online. doi:10.1038/gimo56 (inactive 2015-01-09).
- ↑ Waring JP (1999). "Postfundoplication complications. Prevention and management". Gastroenterol. Clin. North Am. 28 (4): 1007–19, viii–ix. doi:10.1016/S0889-8553(05)70102-3. PMID 10695014.
- ↑ Curet MJ, Josloff RK, Schoeb O, Zucker KA; Josloff; Schoeb; Zucker (1999). "Laparoscopic reoperation for failed antireflux procedures". Archives of surgery 134 (5): 559–63. doi:10.1001/archsurg.134.5.559. PMID 10323431.
- 1 2 Booth, et al., What Is the Current Rate of Gas-Bloat Syndrome Following Open and Laparoscopic Antireflux Surgery?, o(eso Knowledge, http://www.hon.ch/OESO/books/Vol_6_Barrett_s_Esophagus/Articles/vol2/art023.html