Wound
| Wound | |
|---|---|
 Wounded man | |
| Classification and external resources | |
| Specialty | Emergency medicine |
| ICD-10 | T14.0-T14.1 |
| ICD-9-CM | 872-893 |
| MeSH | D014947 |
A wound is a type of injury which happens relatively quickly in which skin is torn, cut, or punctured (an open wound), or where blunt force trauma causes a contusion (a closed wound). In pathology, it specifically refers to a sharp injury which damages the dermis of the skin.
Classification
According to level of contamination a wound can be classified as
- Clean wound, a wound made under sterile conditions where there are no organisms present in the wound and the wound is likely to heal without complications.
- Contaminated wound, where the wound is as a result of accidental injury where there are pathogenic organisms and foreign bodies in the wound.
- Infected wound, where the wound has pathogenic organisms present and multiplying showing clinical signs of infection, where it looks yellow, oozing pus, having pain and redness.
- Colonized wound, where the wound is a chronic one and there are a number of organisms present and very difficult to heal (i.e. a bedsore).
Open
Open wounds can be classified according to the object that caused the wound. The types of open wound are:
- Incisions or incised wounds, caused by a clean, sharp-edged object such as a knife, razor, or glass splinter.
- Lacerations, irregular tear-like wounds caused by some blunt trauma. Lacerations and incisions may appear linear (regular) or stellate (irregular). The term laceration is commonly misused in reference to incisions.
- Abrasions (grazes), superficial wounds in which the topmost layer of the skin (the epidermis) is scraped off. Abrasions are often caused by a sliding fall onto a rough surface.
- Avulsions, injuries in which a body structure is forcibly detached from its normal point of insertion. A type of amputation where the extremity is pulled off rather than cut off.
- Puncture wounds, caused by an object puncturing the skin, such as a splinter, nail or needle.
- Penetration wounds, caused by an object such as a knife entering and coming out from the skin.
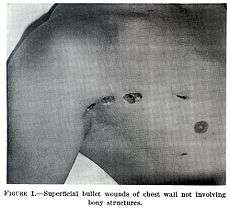
- Gunshot wounds, caused by a bullet or similar projectile driving into or through the body. There may be two wounds, one at the site of entry and one at the site of exit, generally referred to as a "through-and-through."
Closed
Closed wounds have fewer categories, but are just as dangerous as open wounds. The types of closed wounds are:
- Hematomas, also called a blood tumor, caused by damage to a blood vessel that in turn causes blood to collect under the skin.
- Hematomas that originate from internal blood vessel pathology are petechiae, purpura, and ecchymosis. The different classifications are based on size.
- Hematomas that originate from an external source of trauma are contusions, also commonly called bruises.
- Crush injury, caused by a great or extreme amount of force applied over a long period of time.
-

An open wound (an avulsion)
-

A laceration to the leg
-
An infected puncture wound to the bottom of the forefoot.
-
A puncture wound from playing darts.
-

An incision: a small cut in a finger.
Pathophysiology
To heal a wound, the body undertakes a series of actions collectively known as the wound healing process.
Diagnosis
A wound may be recorded for follow-up and observing progress of healing with different techniques which consist of, but not limited to:[1]
- Photographs, with subsequent area quantification using computer processing
- Wound tracings on acetate sheets
- Kundin wound gauge
Management

The overall treatment depends on the type, cause, and depth of the wound as well as whether or not other structures beyond the skin (dermis) are involved. Treatment of recent lacerations involves examining, cleaning, and closing the wound. Minor wounds, like bruises, will heal on their own, with skin discoloration usually disappearing in 1–2 weeks. Abrasions, which are wounds with intact skin (non-penetration through dermis to subcutaneous fat), usually require no active treatment except keeping the area clean, initially with soap and water. Puncture wounds may be prone to infection depending on the depth of penetration. The entry of puncture wound is left open to allow for bacteria or debris to be removed from inside.
Cleaning
Evidence to support the cleaning of wounds before closure is poor.[2] For simple lacerations, cleaning can be accomplished using a number of different solutions, including tap water and sterile saline solution.[2] Infection rates may be lower with the use of tap water in regions where water quality is high.[2] Cleaning of a wound is also known as wound toilet.[3]
Closure
If a person presents to a healthcare center within 6 hours of a laceration they are typically closed immediately after evaluating and cleaning the wound. After this point in time, however, there is a theoretical concern of increased risks of infection if closed immediately.[4] Thus some healthcare providers may delay closure while others may be willing to immediately close up to 24 hours after the injury.[4] A single study has found that using clean non sterile gloves is equivalent to using sterile gloves during wound closure.[5][6]
If closure of a wound is decided upon a number of techniques can be used. These include bandages, a cyanoacrylate glue, staples, and sutures. Absorbable sutures have the benefit over non absorbable sutures of not requiring removal. They are often preferred in children.[7] Buffering the pH of lidocaine makes the freezing less painful.[8]
Adhesive glue and sutures have comparable cosmetic outcomes for minor lacerations <5 cm in adults and children.[9] The use of adhesive glue involves considerably less time for the doctor and less pain for the person with the cut. The wound opens at a slightly higher rate but there is less redness.[10] The risk for infections (1.1%) is the same for both. Adhesive glue should not be used in areas of high tension or repetitive movements, such as joints or the posterior trunk.[9]
Dressings
In the case of clean surgical wounds, there is no evidence that the use of topical antibiotics reduces infection rates in comparison with non-antibiotic ointment or no ointment at all.[11] Antibiotic ointments can irritate the skin, slow healing, and greatly increase the risk of developing contact dermatitis and antibiotic resistance.[11] Because of this, they should only be used when a person shows signs of infection and not as a preventative.[11]
The effectiveness of dressings and creams containing silver to prevent infection or improve healing is not currently supported by evidence.[12]
Alternative medicine
There is moderate evidence that honey is more effective than antiseptic followed by gauze for healing wounds infected after surgical operations. There is a lack of quality evidence relating to the use of honey on other types of wounds, such as minor acute wounds, mixed acute and chronic wounds, pressure ulcers, Fournier's gangrene, venous leg ulcers, diabetic foot ulcers and Leishmaniasis.[13]
There is no good evidence that therapeutic touch is useful in healing.[14] More than 400 species of plants are identified as potentially useful for wound healing.[15] Only three randomized controlled trials, however, have been done for the treatment of burns.[16]
Complications
Bacterial infection of wound can impede the healing process and lead to life-threatening complications. Scientists at Sheffield University have identified a way of using light to rapidly detect the presence of bacteria. They are developing a portable kit in which specially designed molecules emit a light signal when bound to bacteria. Current laboratory-based detection of bacteria can take hours or even days.[17]
Workup
Individuals who have wounds that are not healing should be investigated to find the causes. Many microbiological agents can be responsible for this. The basic workup includes evaluating the wound, its extent and severity. Cultures are usually obtained both from the wound site and blood. X rays are obtained and a tetanus shot may be administered if there is any doubt about prior vaccination [18]
Chronic
Non-healing wounds of the diabetic foot are considered one of the most significant complications of diabetes, representing a major worldwide medical, social, and economic burden that greatly affects patient quality of life. Almost 24 million Americans—one in every 12—are diabetic and the disease is causing widespread disability and death at an epidemic pace, according to the Centers for Disease Control and Prevention. Of those with diabetes, 6.5 million are estimated to suffer with chronic or non-healing wounds. Associated with inadequate circulation, poorly functioning veins, and immobility, non-healing wounds occur most frequently in the elderly and in people with diabetes—populations that are sharply rising as the nation ages and chronic diseases increase.
Although diabetes can ravage the body in many ways, non-healing ulcers on the feet and lower legs are common outward manifestations of the disease. Also, diabetics often suffer from nerve damage in their feet and legs, allowing small wounds or irritations to develop without awareness. Given the abnormalities of the microvasculature and other side effects of diabetes, these wounds take a long time to heal and require a specialized treatment approach for proper healing.
As many as 25% of diabetic patients will eventually develop foot ulcers, and recurrence within five years is 70%. If not aggressively treated, these wounds can lead to amputations. It is estimated that every 30 seconds a lower limb is amputated somewhere in the world because of a diabetic wound. Amputation often triggers a downward spiral of declining quality of life, frequently leading to disability and death. In fact, only about one third of diabetic amputees will live more than five years, a survival rate equivalent to that of many cancers.
Many of these lower extremity amputations can be prevented through an interdisciplinary approach to treatment involving a variety of advanced therapies and techniques, such as debridement, hyperbaric oxygen treatment therapy, dressing selection, special shoes, and patient education. When wounds persist, a specialized approach is required for healing.[19]
History

From the Classical Period to the Medieval Period, the body and the soul were believed to be intimately connected, based on several theories put forth by the philosopher Plato. Wounds on the body were believed to correlate with wounds to the soul and vice versa; wounds were seen as an outward sign of an inward illness. Thus, a man who was wounded physically in a serious way was said to be hindered not only physically but spiritually as well. If the soul was wounded, that wound may also eventually become physically manifest, revealing the true state of the soul.[20] Wounds were also seen as writing on the "tablet" of the body. Wounds acquired in war, for example, told the story of a soldier in a form which all could see and understand, and the wounds of a martyr told the story of their faith.[20]
Research
In humans and mice it has been shown that estrogen might affect the speed and quality of wound healing.[21]
See also
- International Red Cross Wound Classification System
- European Wound Management Association
- Journal of Burns and Wounds
- Wound bed preparation
References
- ↑ Thomas, AC; Wysocki, AB (February 1990). "The healing wound: a comparison of three clinically useful methods of measurement.". Decubitus 3 (1): 18–20, 24–5. PMID 2322408. Retrieved 15 June 2013.
- 1 2 3 Fernandez R, Griffiths R, (15 February 2012). "Water for wound cleansing". Cochrane Database of Systematic Reviews 2: CD003861. doi:10.1002/14651858.CD003861.pub3. PMID 22336796.
- ↑ Simple wound management on patient.info website, viewed 2012-01-08
- 1 2 Eliya, MC; Banda, GW (Sep 7, 2011). Eliya, Martha C, ed. "Primary closure versus delayed closure for non bite traumatic wounds within 24 hours post injury". Cochrane database of systematic reviews (Online) 9 (9): CD008574. doi:10.1002/14651858.CD008574.pub2. PMID 21901725.
- ↑ Perelman, VS; Francis, GJ; Rutledge, T; Foote, J; Martino, F; Dranitsaris, G (March 2004). "Sterile versus nonsterile gloves for repair of uncomplicated lacerations in the emergency department: a randomized controlled trial". Annals of Emergency Medicine 43 (3): 362–70. doi:10.1016/j.annemergmed.2003.09.008. PMID 14985664.
- ↑ van den Broek, PJ (2011). "[Sterile gloves are necessary in minor surgery]". Nederlands tijdschrift voor geneeskunde 155 (18): A3341. PMID 21466736.
- ↑ "BestBets: Absorbable sutures in pediatric lacerations".
- ↑ Cepeda MS, Tzortzopoulou A, Thackrey M, Hudcova J, Arora Gandhi P, Schumann R (2010). Tzortzopoulou, Aikaterini, ed. "Adjusting the pH of lidocaine for reducing pain on injection". Cochrane Database Syst Rev 12 (12): CD006581. doi:10.1002/14651858.CD006581.pub2. PMID 21154371.
- 1 2 Cals, JW; de Bont EGPM (2012). ". Minor incised traumatic laceration". BMJ 345: e6824. doi:10.1136/bmj.e6824. PMID 23092899.
- ↑ Farion, K; et al. (2002). Farion, Ken J, ed. "Tissue adhesives for traumatic lacerations in children and adults". Cochrane Database Syst Rev (3): CD003326. doi:10.1002/14651858.CD003326. PMID 12137689.
- 1 2 3 American Academy of Dermatology (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Academy of Dermatology), retrieved 5 December 2013, which cites
- ↑ D'Amico G, Pagliaro L, Pietrosi G, Tarantino I (2010). d'Amico, Gennaro, ed. "Emergency sclerotherapy versus vasoactive drugs for bleeding oesophageal varices in cirrhotic patients". Cochrane Database Syst Rev 3 (3): CD002233. doi:10.1002/14651858.CD002233.pub2. PMID 20238318.
- ↑ Jull AB, Cullum N, Dumville JC, Westby MJ, Deshpande S, Walker N (6 March 2015). "Honey as a topical treatment for wounds". Cochrane Database of Systematic Reviews 3: CD005083. doi:10.1002/14651858.CD005083.pub4. PMID 25742878.
- ↑ O'Mathúna, DP; Ashford, RL (Jul 29, 2014). "Therapeutic touch for healing acute wounds.". The Cochrane database of systematic reviews 7: CD002766. doi:10.1002/14651858.CD002766.pub3. PMID 25069726.
- ↑ Ghosh, PK; Gaba, A (2013). "Phyto-extracts in wound healing.". Journal of pharmacy & pharmaceutical sciences : a publication of the Canadian Society for Pharmaceutical Sciences, Societe canadienne des sciences pharmaceutiques 16 (5): 760–820. PMID 24393557.
- ↑ Bahramsoltani, R; Farzaei, MH; Rahimi, R (September 2014). "Medicinal plants and their natural components as future drugs for the treatment of burn wounds: an integrative review.". Archives of dermatological research 306 (7): 601–17. doi:10.1007/s00403-014-1474-6. PMID 24895176.
- ↑ "Light to detect wound infection" (web). UK scientists have identified a way of using light to rapidly detect the presence of bacteria. bodat. BBC News. 11 March 2007. Retrieved 2008-03-17.
- ↑ Work Up eMedicine General Surgery. Retrieved on 2010-01-27
- ↑ "The Clinical Case for Use of Hyperbaric Oxygen Therapy in the Treatment of Diabetic Wounds," Diversified Clinical Services, copyright 2009
- 1 2 Reichardt, Paul F. (1984). "Gawain and the image of the wound". PMLA 99 (2): 154–161. doi:10.2307/462158. JSTOR 462158.
- ↑ Desiree May Oh, MD, Tania J. Phillips, MD (2006). "Sex Hormones and Wound Healing". Wounds.
External links
| Wikiquote has quotations related to: Wounds |
| Look up wound in Wiktionary, the free dictionary. |
| Wikimedia Commons has media related to Wounds. |
- US based wound healing society
- Association for the Advancement of Wound Care AAWC
- European Wound Management Association - EWMA works to promote the advancement of education and research.
| ||||||||||||||||||||||||||||||||||||||||||||
|