Left bundle branch block
| Left bundle branch block | |
|---|---|
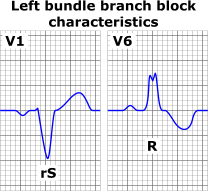 ECG characteristics of a typical LBBB showing wide QRS complexes with abnormal morphology in leads V1 and V6. | |
| Classification and external resources | |
| Specialty | Cardiology, Emergency Medicine |
| ICD-10 | I44.4 - I44.7 |
| DiseasesDB | 7352 |
| eMedicine | ped/2501 |
Left bundle branch block (LBBB) is a cardiac conduction abnormality seen on the electrocardiogram (ECG).[1] In this condition, activation of the left ventricle of the heart is delayed, which causes the left ventricle to contract later than the right ventricle.
Causes
Among the causes of LBBB are:
- Aortic stenosis
- Dilated cardiomyopathy
- Acute myocardial infarction
- Extensive coronary artery disease
- Primary disease of the cardiac electrical conduction system
- Long standing hypertension leading to aortic root dilatation and subsequent aortic regurgitation
- Lyme disease
- Side effect of some cardiac surgeries (e.g., aortic root reconstruction)
Diagnosis
The criteria to diagnose a left bundle branch block on the electrocardiogram:
- The heart rhythm must be supraventricular in origin
- The QRS duration must be ≥ 120 ms[2]
- There should be a QS or rS complex in lead V1
- There should be a notched ('M'-shaped) R wave in lead V6.
The T wave should be deflected opposite the terminal deflection of the QRS complex. This is known as appropriate T wave discordance with bundle branch block. A concordant T wave may suggest ischemia or myocardial infarction.
There are also partial blocks of the left bundle branch: "left anterior fascicular block" (LAFB)[3] and a "left posterior fascicular block" (LPFB).[4] This refers to the bifurcation of the left bundle branch.
Diagnostic consequences
The presence of LBBB results in that electrocardiography (ECG) cannot be used to diagnose left ventricular hypertrophy or Q wave infarction, because LBBB in itself results in widened QRS complex, and changes in the ST-T segment consistent with ischemia or injury.[5]
Treatment
- Patients with LBBB require complete cardiac evaluation, and those with LBBB and syncope or near-syncope may require a pacemaker.
- Some patients with LBBB, a markedly prolonged QRS (usually > 150 ms), and systolic heart failure may benefit from a biventricular pacemaker, which allows for better synchrony of heart contractions.[6]
See also
References
- ↑ "Conduction Blocks 2006 KCUMB". Retrieved 2009-01-20.
- ↑ "Lesson VI - EKG Conduction Abnormalities". Retrieved 2009-01-07.
- ↑ x20050921122910832459 at GPnotebook
- ↑ x20050921123129832459 at GPnotebook
- ↑ Emily Groepper, Nasar Nallamothu, Wilfred Lam, Frank Aguirre, Kristi Bergman, Patricia Good, Patricia Wright (May 13, 2014). "Electrocardiography > Left Bundle Branch Block (LBBB)". SIU School of Medicine. Retrieved 2015-07-02.
- ↑ Stevenson WG, Hernaddez AF, Carson PE, et al. Indications for cardiac resynchronization therapy: 2011 update from the Heart Failure Society of America guideline committee. J Card Fail 2012; 18:94-106.
External links
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||