Iron-deficiency anemia
| Iron-deficiency anemia | |
|---|---|
 | |
| Classification and external resources | |
| Specialty | Hematology |
| ICD-10 | D50 |
| ICD-9-CM | 280 |
| DiseasesDB | 6947 |
| MedlinePlus | 000584 |
| eMedicine | med/1188 |
| MeSH | D018798 |
Iron-deficiency anemia, also spelled iron deficiency anaemia,[help 1] is anemia due to not enough iron. Anemia is defined as a decrease in the amount of red blood cells (RBCs) or hemoglobin in the blood.[1][2] When anemia comes on slowly, the symptoms are often vague and may include feeling tired, weakness, shortness of breath or poor ability to exercise. Anemia that comes on quickly often has greater symptoms which may include: confusion, feeling like one is going to pass out, and increased thirst. There needs to be significant anemia before a person becomes noticeably pale. There may be additional symptoms depending on the underlying cause.[3]
It is caused by insufficient dietary intake and absorption of iron, or iron loss from bleeding. Bleeding can be from a range of sources such as the intestinal, uterine or urinary tract. The most common cause of iron-deficiency anemia in children in developing countries is parasitic worms. Worms cause intestinal bleeding, which is not always noticeable in feces, and is especially damaging to children.[4] Malaria, hookworms and vitamin A deficiency contribute to anemia during pregnancy in most underdeveloped countries.[5] In women over 50 years old, the most common cause of iron-deficiency anemia is chronic gastrointestinal bleeding from nonparasitic causes, such as gastric ulcers, duodenal ulcers or gastrointestinal cancer.
Iron deficiency causes approximately half of all anemia cases worldwide, and affects women more often than men. Iron-deficiency anemia affects nearly 1 billion.[6] In 2013 anemia due to iron deficiency resulted in about 183,000 deaths – down from 213,000 deaths in 1990.[7]
Signs and symptoms
Iron-deficiency anemia is characterized by the sign of pallor (reduced oxyhemoglobin in skin or mucous membranes), and the symptoms of fatigue, lightheadedness, and weakness. None of the symptoms (or any of the others below) are sensitive or specific. Pallor of mucous membranes (primarily the conjunctiva) in children indicates anemia with best correlation to the actual disease, but in a large study was found to be only 28% sensitive and 87% specific (with high predictive value) in distinguishing children with anemia [hemoglobin (Hb) <11.0 g/dl] and 49% sensitive and 79% specific in distinguishing severe anemia (Hb < 7.0 g/dl).[8] Thus, this sign is reasonably predictive when present, but not helpful when absent, as only one-third to one-half of children who are anemic (depending on severity) will show pallor. Iron-deficiency must be diagnosed by laboratory testing.
Because iron deficiency tends to develop slowly, adaptation occurs and the disease often goes unrecognized for some time, even years; patients often adapt to the systemic effects that anaemia causes. In severe cases, dyspnea (trouble breathing) can occur. Unusual obsessive food cravings, known as pica, may develop. Pagophagia or pica for ice has been suggested to be specific, but is actually neither a specific or sensitive symptom, and is not helpful in diagnosis. When present, it may (or may not) disappear with correction of iron-deficiency anemia.
Other symptoms and signs of iron-deficiency anemia include:
- Anxiety often resulting in OCD-type compulsions and obsessions
- Irritability or a low feeling
- Angina
- Constipation
- Sleepiness/Hypersomnia
- Tinnitus
- Mouth ulcers
- Palpitations
- Hair loss
- Fainting or feeling faint
- Depression
- Breathlessness
- Twitching muscles
- Pale yellow skin
- Tingling, numbness, or burning sensations
- Missed menstrual cycle
- Slow social development
- Glossitis (inflammation or infection of the tongue)
- Angular cheilitis (inflammatory lesions at the mouth's corners)
- Koilonychia (spoon-shaped nails) or nails that are weak or brittle
- Poor appetite
- Pruritus (itchiness)
- Dysphagia due to formation of esophageal webs (Plummer-Vinson syndrome)
- Insomnia
- Restless legs syndrome[9]
Infant development
Iron-deficiency anemia for infants in their earlier stages of development may have greater consequences than it does for adults. An infant made severely iron-deficient during its earlier life cannot recover to normal iron levels even with iron therapy. In contrast, iron deficiency during later stages of development can be compensated with sufficient iron supplements. Iron-deficiency anemia affects neurological development by decreasing learning ability, altering motor functions, and permanently reducing the number of dopamine receptors and serotonin levels. Iron deficiency during development can lead to reduced myelination of the spinal cord, as well as a change in myelin composition. Additionally, iron-deficiency anemia has a negative effect on physical growth. Growth hormone secretion is related to serum transferrin levels, suggesting a positive correlation between iron-transferrin levels and an increase in height and weight. This is also linked to pica, as it can be a cause.
Cause
A diagnosis of iron-deficiency anemia then requires further investigation as to its cause. It can be caused by increased iron demand / loss or decreased iron intake,[10] and can occur in both children and adults. The cause of chronic blood loss should all be considered, according to the patient's sex, age, and history, and anaemia without an attributable underlying cause is sufficient for an urgent referral to exclude underlying malignancy. In babies and adolescents, rapid growth may outpace dietary intake of iron, and result in deficiency without disease or grossly abnormal diet.[10] In women of childbearing age, heavy or long menstrual periods can also cause mild iron-deficiency anemia.
Parasitosis
The leading cause of iron deficiency worldwide is infestation with parasitic worms (helminths such as tapeworms, flukes, and roundworms). The World Health Organization estimates that "approximately two billion people are infected with soil-transmitted helminths worldwide."[11] Parasitic worms cause both inflammation and chronic blood loss.
Blood loss
Blood contains iron within red blood cells, so blood loss leads to a loss of iron. There are several common causes of blood loss: Women with menorrhagia (heavy periods) are at risk of iron-deficiency anemia because they are at higher-than-normal risk of losing a larger amount blood during menstruation than is replaced in their diet. Slow, chronic blood loss within the body — such as from a peptic ulcer, angiodysplasia, a colon polyp or gastrointestinal cancer, excessively heavy periods — can cause iron-deficiency anemia. Gastrointestinal bleeding can result from regular use of some groups of medication, such as NSAIDs (e.g. aspirin), anticoagulants such as clopidogrel and warfarin, although these are required in some patients, especially those with states causing thrombophilia.
Diet
The body normally gets the iron it requires from foods. If a person consumes too little iron, or iron that is poorly absorbed (non-heme iron), they can become iron deficient over time. Examples of iron-rich foods include meat, eggs, leafy green vegetables and iron-fortified foods. For proper growth and development, infants and children need iron from their diet, too.[12] A high intake of cow’s milk is associated with an increased risk of iron deficiency anaemia.[13] Other risk factors for iron deficiency include low meat intake and low intake of iron-fortified products.[13]
Iron absorption
Iron from food is absorbed into the bloodstream in the small intestine, especially the duodenum and proximal ileum. Many intestinal disorders can reduce the body's ability to absorb iron. There are different mechanisms that may be present.
In cases where there has been a reduction in surface area of the bowel, such as in celiac disease, inflammatory bowel disease or post surgical resection, the body can absorb iron, but there is simply insufficient surface area.
If there is insufficient production of hydrochloric acid in the stomach, hypochlorhydria/achlorhydria (often due to chronic H. pylori infections or long-term proton pump inhibitor therapy) Ferrous and Ferric iron salts will precipitate out of solution in the bowel which are poorly absorbed.
In cases where systemic inflammation is present, iron will be absorbed into enterocytes, but due to the reduction in basolateral ferroportin molecules which allow iron to pass into the systemic circulation, iron is trapped in the enterocytes and is lost from the body when the enterocytes are sloughed off.
Depending on the disease state, one or more mechanisms may occur.
Pregnancy
Without iron supplementation, iron deficiency anemia occurs in many pregnant women because their iron stores need to serve their own increased blood volume as well as be a source of hemoglobin for the growing fetus, and for placental development.[12]
Other less common causes are intravascular hemolysis and hemoglobinuria.
Mechanism
Anemia is one result of significant iron deficiency. When the body has sufficient iron to meet its needs (functional iron), the remainder is stored for later use in all cells, but mostly in the bone marrow, liver, and spleen. These stores are called ferritin complexes and are part of the human (and other animals) iron metabolism systems. Ferritin complexes in humans carry about 4500 iron atoms and form into 24 protein subunits of two different types.[14]
Diagnosis
History
Anemia may be diagnosed from symptoms and signs, but when it is mild, it may not be diagnosed from mild nonspecific symptoms.
The diagnosis of iron-deficiency anemia will be suggested by appropriate history (e.g. anemia in a menstruating woman or an athlete engaged in long-distance running), the presence of occult blood (i.e. hidden blood) in the stool, and often by other history.[15] For example, known celiac disease can cause malabsorption of iron. A travel history to areas in which hookworms and whipworms are endemic may be helpful in guiding certain stool tests for parasites or their eggs.
Blood tests
| Change | Parameter |
|---|---|
| ↓ | ferritin, hemoglobin, MCV |
| ↑ | TIBC, transferrin, RDW |
Anemia is often first shown by routine blood tests, which generally include a complete blood count (CBC) which is performed by an instrument which gives an output as a series of index numbers. A sufficiently low hemoglobin (Hb) by definition makes the diagnosis of anemia, and a low hematocrit value is also characteristic of anemia. Further studies will be undertaken to determine the anemia's cause. If the anemia is due to iron deficiency, one of the first abnormal values to be noted on a CBC, as the body's iron stores begin to be depleted, will be a high red blood cell distribution width (RDW), reflecting an increased variability in the size of red blood cells (RBCs). In the course of slowly depleted iron status, an increasing RDW normally appears even before anemia appears.
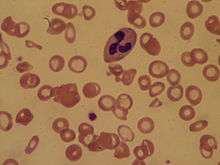
A low mean corpuscular volume (MCV) often appears next during the course of body iron depletion. It corresponds to a high number of abnormally small red blood cells. A low MCV, a low mean corpuscular hemoglobin or mean corpuscular hemoglobin concentration, and the appearance of the RBCs on visual examination of a peripheral blood smear narrows the problem to a microcytic anemia (literally, a "small red blood cell" anemia). The numerical values for these measures are all calculated by modern laboratory equipment.
The blood smear of a person with iron deficiency shows many hypochromic (pale and relatively colorless) and rather small RBCs, and may also show poikilocytosis (variation in shape) and anisocytosis (variation in size). With more severe iron-deficiency anemia, the peripheral blood smear may show hypochromic pencil-shaped cells, and occasionally small numbers of nucleated red blood cells.[16] Very commonly, the platelet count is slightly above the high limit of normal in iron deficiency anemia (this is mild thrombocytosis). This effect was classically postulated to be due to high erythropoietin levels in the body as a result of anemia, cross-reacting to activate thrombopoietin receptors in the precursor cells that make platelets; however, this process has not been corroborated. Such slightly increased platelet counts present no danger, but remain valuable as an indicator even if their origin is not yet known.
Body-store iron deficiency is diagnosed by tests such as a low serum ferritin, a low serum iron level, an elevated serum transferrin and a high total iron binding capacity. A low serum ferritin is the most sensitive lab test for iron deficiency anemia. However, serum ferritin can be elevated by any type of chronic inflammation and so is not always a reliable test of iron status if it is within normal limits (i.e. this test is meaningful if abnormally low, but less meaningful if normal).
Serum iron levels (i.e. iron not part of the hemoglobin in red cells) may be measured directly in the blood, but these levels increase immediately with iron supplementation (the patient must stop supplements for 24 hours), and pure blood-serum iron concentration in any case is not as sensitive as a combination of total serum iron, along with a measure of the serum iron-binding protein levels (TIBC). The ratio of serum iron to TIBC (called iron saturation or transferrin saturation index or percent) is the most specific indicator of iron deficiency, when it is sufficiently low. The iron saturation (or transferrin saturation) of < 5% almost always indicates iron deficiency, while levels from 5% to 10% make the diagnosis of iron deficiency possible but not definitive. Saturations over 12% (taken alone) make the diagnosis unlikely. Normal saturations are usually slightly lower for women (>12%) than for men (>15%), but this may indicate simply an overall slightly poorer iron status for women in the "normal" population.
Iron-deficiency anemia and thalassemia minor present with many of the same lab results. It is very important not to treat a people with thalassemia with an iron supplement, as this can lead to hemochromatosis (accumulation of iron in various organs, especially the liver). A hemoglobin electrophoresis provides useful evidence for distinguishing these two conditions, along with iron studies.
Screening
It is unclear if screening pregnant women for iron deficiency during pregnancy improves outcomes in the developing world.[17]
Gold standard
Conventionally, a definitive diagnosis requires a demonstration of depleted body iron stores obtained by bone marrow aspiration, with the marrow stained for iron.[18][19] Because this is invasive and painful, while a clinical trial of iron supplementation is inexpensive and not traumatic, patients are often treated based on clinical history and serum ferritin levels without a bone marrow biopsy. Furthermore, a study published April 2009[20] questions the value of stainable bone marrow iron following parenteral iron therapy.
Treatment
Anemia is sometimes treatable, but certain types of anemia may be lifelong. If the cause is dietary iron deficiency, eating more iron-rich foods, such as beans, lentils or red meat, or taking iron supplements will usually correct the anemia. Alternatively, intravenous iron can be administered.
The difference between iron intake and iron absorption, also known as bioavailability, can be great. Iron absorption problems are worsened when iron is taken in conjunction with milk, tea, coffee and other substances. A number of methods that can help mitigate this, including:
- Fortification with ascorbic acid increases bioavailability in both presence and absence of inhibiting substances, but is subject to deterioration from moisture or heat. Ascorbic acid fortification is usually limited to sealed, dried foods, but individuals can easily take ascorbic acid with a basic iron supplement for the same benefits. The primary benefit over ascorbic acid is durability and shelf life, particularly for products like milk, which undergo heat treatment.
- Microencapsulation with lecithin binds and protects the iron particles from the action of inhibiting substances.
- Using an iron amino acid chelate, such as NaFeEDTA, similarly binds and protects the iron particles. A study by the hematology unit of the University of Chile indicated chelated iron (ferrous bis-glycine chelate) can work with ascorbic acid to achieve even higher absorption levels.
- Separating intake of iron and inhibiting substances by a few hours
- Using nondairy milk (such as soy, rice, or almond milk) or goats' milk instead of cows' milk
- Gluten-free diets can resolve some instances of iron-deficiency anemia, if it is a result of celiac disease.
- Heme iron, found only in animal foods, such as meat, fish and poultry, is more easily absorbed than nonheme iron, found in plant foods and supplements.[21][22]
Iron bioavailability comparisons require stringent controls, because the largest factor affecting bioavailability is the subject's existing iron level. Informal studies on bioavailability usually do not take this factor into account, so exaggerated claims from health supplement companies based on this sort of evidence should be ignored. Scientific studies are still in progress to determine which approaches yield the best results and the lowest costs.
If anemia does not respond to oral treatments, it may be necessary to administer iron parenterally using a drip or hemodialysis. Parenteral iron involves risks of fever, chills, backache, myalgia, dizziness, syncope, rash, and with some preparations, anaphylactic shock. The total incidence of adverse events is much lower than that with oral tablets (where the dose needs to be reduced or treatment stopped in over 40% of subjects) and blood transfusions.
A follow-up blood test is important to demonstrate whether the treatment has been effective; it can be undertaken after two to four weeks. With oral iron, this usually requires a delay of three months for tablets to have a significant effect.
Iron supplementation and infection risk
Because one of the functions of elevated ferritin (an acute phase reaction protein) in acute infections is thought to be to sequester iron from bacteria, it is generally thought that Parenteral iron supplementation (which circumvents this mechanism) should be avoided in patients who have active bacterial infections bacteraemia. Replacement of iron stores is seldom such an emergency situation that it cannot wait for such infections to be treated, although occasionally cases will arise where this is not possible, such as chronic osteomyelitis.
Iron deficiency protects against infection by creating an unfavorable environment for bacterial growth. Some studies have found iron supplementation can lead to an increase in infectious disease morbidity in areas where bacterial infections or where malaria are common. For example, children receiving iron-enriched foods have demonstrated an increased rate in diarrhea overall and enteropathogen shedding. Nevertheless, while iron deficiency might lessen infections by certain pathogenic diseases, it also leads to a reduction in resistance to other strains of viral or bacterial infections, such as Salmonella typhimurium or Entamoeba histolytica. Overall, it is sometimes difficult to decide whether iron supplementation will be beneficial or harmful to an individual in an environment prone to many infectious diseases; however, this is a different question than the question of supplementation in individuals who are already ill with a bacterial infection.
Epidemiology

A moderate degree of iron-deficiency anemia affected approximately 610 million people worldwide or 8.8% of the population.[6] It is slightly more common in female (9.9%) than males (7.8%).[6] Mild iron deficiency anemia affects another 375 million.[6]
Notes
- ↑ The anemia and anaemia difference is a regional variation; the hyphen is optional (several major dictionaries use it and several do not).
References
- ↑ "Anemia". http://www.merriam-webster.com/. Retrieved 7 July 2014. External link in
|website=(help) - ↑ Stedman's Medical Dictionary (28th ed.). Philadelphia: Lippincott Williams & Wilkins. 2006. p. Anemia. ISBN 9780781733908.
- ↑ Janz, TG; Johnson, RL; Rubenstein, SD (Nov 2013). "Anemia in the Emergency Department: Evaluation and Treatment". Emergency Medicine Practice 15 (11): 1–15; quiz 15–6. PMID 24716235.
- ↑ Calis JC, Phiri KS, Faragher EB, et al. (2008). "Severe Anemia in Malawian Children". N. Engl. J. Med. 358 (9): 888–99. doi:10.1056/NEJMoa072727. PMID 18305266.
- ↑ Dreyfuss ML, Stoltzfus RJ, Shrestha JB, et al. (2000). "Hookworms, Malaria and Vitamin A Deficiency Contribute to Anemia and Iron Deficiency Among Pregnant Women in the Plains of Nepal". J. Nutr. 130 (10): 2527–36. PMID 11015485.
- 1 2 3 4 Vos, T; Flaxman, AD; Naghavi, M; Lozano, R; Michaud, C; Ezzati, M; Shibuya, K; Salomon, JA; et al. (Dec 15, 2012). "Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries 1990-2010: a Systematic Analysis for the Global Burden of Disease Study 2010". Lancet 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ↑ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, Regional, and National Age-Sex Specific All-Cause and Cause-Specific Mortality for 240 Causes of Death, 1990-2013: a Systematic Analysis for the Global Burden of Disease Study 2013". Lancet 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ↑ Pallor in diagnosis of iron deficiency in children
- ↑ Rangarajan, Sunad; D'Souza, George Albert. (April 2007). "Restless legs syndrome in Indian patients having iron deficiency anemia in a tertiary care hospital". Sleep Medicine. 8 (3): 247–51. doi:10.1016/j.sleep.2006.10.004. PMID 17368978.
- 1 2 "NPS News 70: Iron deficiency anaemia". NPS Medicines Wise. October 1, 2010. Retrieved November 5, 2010.
- ↑ World Health Organization Fact Sheet No. 366, Soil Transmitted Helminth Infections, updated June 2013
- 1 2 "Iron deficiency anemia". Mayo Clinic. March 4, 2011. Retrieved December 11, 2012.
- 1 2 Decsi, T.; Lohner, S. (2014). "Gaps in meeting nutrient needs in healthy toddlers.". Ann Nutr Metab 65 (1): 22–8. doi:10.1159/000365795. PMID 25227596.
- ↑ Handout: Iron Deficiency Anemia – National Anemia Action Council
- ↑ Brady PG (October 2007). "Iron deficiency anemia: a call for". Southern Medical Journal 100 (10): 966–967. doi:10.1097/SMJ.0b013e3181520699. PMID 17943034. Retrieved July 23, 2012.
- ↑ Stephen J. McPhee, Maxine A. Papadakis. Current medical diagnosis and treatment 2009 page.428
- ↑ Siu, AL; U.S. Preventive Services Task, Force (6 October 2015). "Screening for Iron Deficiency Anemia and Iron Supplementation in Pregnant Women to Improve Maternal Health and Birth Outcomes: U.S. Preventive Services Task Force Recommendation Statement.". Annals of internal medicine 163 (7): 529–36. doi:10.7326/m15-1707. PMID 26344176.
- ↑ Mazza, J.; Barr, R. M.; McDonald, J. W.; Valberg, L. S. (21 October 1978). "Usefulness of the serum ferritin concentration in the detection of iron deficiency in a general hospital". Canadian Medical Association Journal 119 (8): 884–886. PMC 1819106. PMID 737638. Retrieved 2009-05-04.
- ↑ Kis, AM; Carnes, M (July 1998). "Detecting Iron Deficiency in Anemic Patients with Concomitant Medical Problems". J Gen Intern Med. 13 (7): 455–61. doi:10.1046/j.1525-1497.1998.00134.x. PMC 1496985. PMID 9686711.
- ↑ Thomason, Ronald W.; Almiski, Muhamad S. (April 2009). "Evidence That Stainable Bone Marrow Iron Following Parenteral Iron Therapy Does Not Correlate With Serum Iron Studies and May Not Represent Readily Available Storage Iron". American Journal of Clinical Pathology 131 (4): 580–585. doi:10.1309/AJCPBAY9KRZF8NUC. PMID 19289594. Retrieved 2009-05-04.
- ↑ National Institutes of Health. "Dietary Supplement Fact Sheet: Iron". United States of America, Department of Health and Human Services. Retrieved March 8, 2012.
- ↑ Miret, Silvia; Simpson, Robert J.; McKie, Andrew T. (1 July 2003). "Physiology and molecular biology of dietary iron absorption". Annual Review of Nutrition 23 (1): 283–301. doi:10.1146/annurev.nutr.23.011702.073139.
- ↑ "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002.
External links
- The Importance of Iron – From IronTherapy.Org
- Interactive material on Iron Metabolism – From IronAtlas.com
- Establishing the cause of anemia – From AnaemiaWorld.com
- Handout: Iron Deficiency Anemia – From the National Anemia Action Council
- NPS News 70: Iron deficiency anaemia: NPS – Better choices, Better health – From the National Prescribing Service
- 1993342985 at GPnotebook