Intussusception (medical disorder)
| Intussusception | |
|---|---|
|
An intussuception as seen on CT | |
| Classification and external resources | |
| Specialty | Pediatrics, general surgery |
| ICD-10 | K38.8, K56.1 |
| ICD-9-CM | 543.9, 560.0 |
| OMIM | 147710 |
| DiseasesDB | 6913 |
| MedlinePlus | 000958 |
| eMedicine | emerg/385 |
| MeSH | D007443 |
An intussusception is a medical condition in which a part of the intestine invaginates (folds into) into another section of intestine, similar to the way the parts of a collapsible telescope retract into one another.[1] This can often result in an obstruction. The part that prolapses into the other is called the intussusceptum, and the part that receives it is called the intussuscepiens. Intussusception is a medical emergency and a patient should be seen immediately to reduce risk.
Signs and symptoms
Early symptoms can include periodic abdominal pain nausea, vomiting (sometimes green in color from bile), pulling legs to the chest area, and intermittent moderate to severe cramping abdominal pain. Pain is intermittent—not because the intussusception temporarily resolves, but because the intussuscepted bowel segment transiently stops contracting. Later signs include rectal bleeding, often with "red currant jelly" stool (stool mixed with blood and mucus), and lethargy. Physical examination may reveal a "sausage-shaped" mass, felt upon palpating the abdomen.[2] Children, or those unable to communicate symptoms verbally, may cry, draw their knees up to their chest. or experience dyspnea (difficult or painful breathing) with paroxysms of pain.
Fever is not a symptom of intussusception. However, intussusception can cause a loop of bowel to become necrotic, secondary to ischemia due to compression to arterial blood supply. This leads to perforation and sepsis, which causes fever.
In rare cases, intussusception may be a complication of Henoch-Schönlein purpura (HSP), an immune-mediated vasculitis disease in children. Such patients who develop intussusception often present with severe abdominal pain in addition to the classic signs and symptoms of HSP.
Cause
Intussusception causes are not clearly established or understood. They can include infections, anatomical factors, and altered motility. Some researchers suspect infectious agents, including rotavirus, are causative factor, but studies and analysis have not conclusively established this. A review of sparse data on the possible association between natural rotavirus and intussusception has not demonstrated a possible association until very recently. In addition, ecological studies revealed that no seasonality exists for intussusception in the United States, whereas rotavirus has distinct wintertime peaks. In developing countries, patterns of intussusception may be quite variable and different from developed countries. This may likely be due to incomplete reporting of cases in developing countries. Rates of intussusception may also vary according to socioeconomic status in developing country.
Pathophysiology
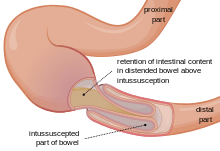
In the most frequent type of intussusception, the ileum enters the cecum. However, other types occur, such as when a part of the ileum or jejunum prolapses into itself. Almost all intussusceptions occur with the intussusceptum having been located proximally to the intussuscipiens. This is because peristaltic action of the intestine pulls the proximal segment into the distal segment. There are, however, rare reports of the opposite being true.
An anatomic lead point (that is, a piece of intestinal tissue that protrudes into the bowel lumen) is present in approximately 10% of intussusceptions.[3]
The trapped section of bowel may have its blood supply cut off, which causes ischemia (lack of oxygen in the tissues). The mucosa (gut lining) is very sensitive to ischemia, and responds by sloughing off into the gut. This creates the classically described "red currant jelly" stool, which is a mixture of sloughed mucosa, blood, and mucus.[4] A study reported that in actuality, only a minority of children with intussusception had stools that could be described as "red currant jelly," and hence intussusception should be considered in the differential diagnosis of children passing any type of bloody stool.[5]
Diagnosis


An Intussusception is often suspected based on history and physical exam, including observation of Dance's sign. Per rectal examination is particularly helpful in children as part of the intussusceptum may be felt by the finger. A definite diagnosis often requires confirmation by diagnostic imaging modalities. Ultrasound is the imaging modality of choice for diagnosis and exclusion of intussusception,due to its high accuracy and lack of radiation. A target-like mass, usually around 3 cm in diameter, confirms the diagnosis. This sign has a doughnut shape created by the hyperechoic central core of bowel and mesentery surrounded by the hypoechoic outer edematous bowel, seen on transverse sonography or computed tomography.[6] In longitudinal imaging intussusception resembles a sandwich.[6]
An x-ray of the abdomen may be indicated to check for intestinal obstruction or free intraperitoneal gas. The latter finding implies that bowel perforation has already occurred. Some institutions use air enema for diagnosis, as the same procedure can be used for treatment.[7]
Classification
- Ileoileal - 5%
- Ileocolic - 77%
- Ileo-ileo-colic - 12%
- Colocolic - 2%
- Multiple - 1%
- Retrograde - 0.2%
- Others - 2.8%[8]
Differential diagnosis
An Intussusception has two main differential diagnoses: acute gastroenteritis and rectal prolapse. Abdominal pain, vomiting, and stool with mucus and blood are present in acute gastroenteritis, but diarrhea is the leading symptom. Rectal prolapse can be differentiated by projecting mucosa that can be felt in continuity with the perianal skin, whereas in intussusception the finger may pass indefinitely into the depth of sulcus.
Treatment
The condition is not usually immediately life-threatening. The intussusception can be treated with either a barium or water-soluble contrast enema or an air-contrast enema, which both confirms the diagnosis of intussusception, and in most cases successfully reduces it. The success rate is over 80%. However, approximately 5–10% of these recur within 24 hours.
Cases where it cannot be reduced by an enema or the intestine is damaged require surgical reduction. In a surgical reduction, the surgeon opens the abdomen and manually squeezes (rather than pulls) the part that has telescoped. If the surgeon cannot successfully reduce it, or the bowel is damaged, they resect the affected section. More often, the intussusception can be reduced by laparoscopy, pulling the segments of intestine apart with forceps.
Prognosis
Intussusception may become a medical emergency if not treated early, as it eventually causes death if not reduced. In developing countries where medical hospitals are not easily accessible, especially when other problems complicate the intussusception, death becomes almost inevitable. When intussusception or any other severe medical problem is suspected, the person must be taken to a hospital immediately.
The outlook for intussusception is excellent when treated quickly, but when untreated it can lead to death within two to five days. It requires fast treatment, because the longer the intestine segment is prolapsed the longer it goes without bloodflow, and the less effective a non-surgical reduction is. Prolonged intussusception also increases the likelihood of bowel ischemia and necrosis, requiring surgical resection.
Epidemiology
The condition is diagnosed most often in infancy and early childhood. It strikes about 2,000 infants (one in every 1,900) in the United States in the first year of life. Its incidence begins to rise at about one to five months of life, peaks at four to nine months of age, and then gradually declines at around 18 months.
Intussusception occurs more frequently in boys than in girls, with a ratio of approximately 3:1.[9]
In adults, intussusception represents the cause of approximately 1% of bowel obstructions and is frequently associated with neoplasm, malignant or otherwise.[10]
References
- ↑ Gylys, Barbara A. and Mary Ellen Wedding (2009), Medicasl Terminology Systems, F.A. Davis Company
- ↑ Cera, SM (2008). "Intestinal Intussusception". Clin Colon Rectal Surg 21 (2): 106–13. doi:10.1055/s-2008-1075859. ISSN 1531-0043. PMC 2780199. PMID 20011406.
- ↑ Chapter X.4. Intussusception from Case Based Pediatrics For Medical Students and Residents, by Lynette L. Young, MD. Department of Pediatrics, University of Hawaii John A. Burns School of Medicine. December 2002
- ↑ Toso C, Erne M, Lenzlinger PM, Schmid JF, Büchel H, Melcher G, Morel P (2005). "Intussusception as a cause of bowel obstruction in adults" (PDF). Swiss Med Wkly 135 (5-6): 87–90. PMID 15729613.
- ↑ Yamamoto, LG; Morita, SY; Boychuk, RB; Inaba, AS; Rosen, LM; Yee, LL; Young, LL (May 1997). "Stool appearance in intussusception: assessing the value of the term "currant jelly."". The American journal of emergency medicine 15 (3): 293–8. doi:10.1016/s0735-6757(97)90019-x. PMID 9148991.
- 1 2 Park NH, Park SI, Park CS, Lee EJ, Kim MS, Ryu JA, Bae JM (2007). "Ultrasonographic findings of small bowel intussusception, focusing on differentiation from ileocolic intussusception". Br J Radiol 80 (958): 798–802. doi:10.1259/bjr/61246651. ISSN 0007-1285. PMID 17875595.
- ↑ Singh C , Prakash M., Adult Intussception : A Case Report, WebmedCentral RADIOLOGY 2011;2(7):WMC002052 External link in
|publisher=(help) - ↑ Bailey & Love's/24th/1195
- ↑ Lonnie King, M.D., FACEP (2006). "Pediatrics: Intussusception". Retrieved 2006-06-05.
- ↑ Gayer G, Zissin R, Apter S, Papa M, Hertz M (2002). "Pictorial review: adult intussusception--a CT diagnosis". Br J Radiol 75 (890): 185–90. PMID 11893645.
Further reading
|