Hydranencephaly
| Hydranencephaly Hydrancephaly | |
|---|---|
|
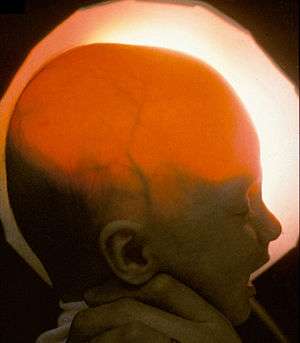
Image of a baby with hydrancephaly, light passes through the skull indicating lack of forebrain. Courtesy of D. P. Agamanolis http://neuropathology-web.org" | |
| Classification and external resources | |
| Specialty | medical genetics |
| ICD-10 | Q04.3 |
| ICD-9-CM | 742.3 |
| DiseasesDB | 31516 |
| eMedicine | radio/351 |
| MeSH | D006832 |
Hydranencephaly or hydrancephaly [1] is a condition in which the brain's cerebral hemispheres are absent to varying degrees and the remaining cranial cavity is filled with cerebrospinal fluid.[2]
Hydranencephaly (or hydrancephaly)[3] is a type of cephalic disorder. These disorders are congenital conditions that derive from either damage to, or abnormal development of, the fetal nervous system in the earliest stages of development in utero. Cephalic is the medical term for “head” or “head end of body.” These conditions do not have any definitive identifiable cause factor; instead generally attributed to a variety of hereditary or genetic conditions, but also by environmental factors such as maternal infection, pharmaceutical intake, or even exposure to high levels of radiation.[4]
This should not be confused with hydrocephalus, which is an accumulation of cerebrospinal fluid in the ventricles of the brain.
In hemihydranencephaly, only half of the cranial cavity is filled with fluid.[5]
Presentation
Usually the cerebellum and brain stem are formed normally, although in some cases the cerebellum may also be absent. An infant with hydranencephaly may appear normal at birth or may have some distortion of the skull and upper facial features due to fluid pressure inside the skull. The infant's head size and spontaneous reflexes such as sucking, swallowing, crying, and moving the arms and legs may all seem normal, depending on the severity of the condition. However, after a few weeks the infant sometimes becomes irritable and has increased muscle tone (hypertonia). After several months of life, seizures and hydrocephalus may develop, if they did not exist at birth. Other symptoms may include visual impairment, lack of growth, deafness, blindness, spastic quadriparesis (paralysis), and intellectual deficits.
Some infants may have additional abnormalities at birth including seizures, myoclonus (involuntary sudden, rapid jerks), limited thermoregulation abilities, and respiratory problems.
Still other infants display no obvious symptoms at birth, going many months without a confirmed diagnosis of hydranencephaly. In some cases a severe hydrocephalus, or other cephalic condition, is misdiagnosed.
Causes
Hydranencephaly is an extreme form of porencephaly, which is characterized by a cyst or cavity in the cerebral hemispheres.
Although the exact cause of hydranencephaly remains undetermined in most cases, the most likely general cause is by vascular insult such as stroke or injury, intrauterine infections, or traumatic disorders after the first trimester of pregnancy. In a number of cases where intrauterine infection was determined the causing factor, most involved toxoplasmosis and viral infections such as enterovirus, adenovirus, parvovirus, cytomegalic, herpes simplex, Epstein-Barr, and syncytial viruses. Another cause factor is determined to be monochorionic twin pregnancies, involving the death of one twin in the second trimester, which in turn causes vascular exchange to the living twin through placental circulation through twin-to-twin transfusion, causing hydranencephaly in the surviving fetus.[6] One medical journal reports hydranencephaly as an autosomal inherited disorder with an unknown mode of transmission, where an unknown blockage of the carotid artery where it enters the cranium causes obstruction and damage to the cerebral cortex.[3]
As a recessive genetic condition, both parents must carry the asymptomatic gene and pass it along to their child, a chance of 25 percent. Despite determination of cause, hydranencephaly afflicts both males and females in equal numbers.
Though hydranencephaly is typically a congenital disorder, it can occur as a postnatal diagnosis in the aftermath of meningitis, intracerebral infarction, and ischemia (stroke), or other traumatic brain injury.[7]
Diagnosis
Diagnosis may be delayed for several months because the infant's early behavior appears to be relatively normal. Transillumination, an examination in which light is passed through body tissues, can be used to diagnose hydranencephaly. An accurate, confirmed diagnosis is generally impossible until after birth, though prenatal diagnosis using fetal ultrasonography (ultrasound) can identify characteristic physical abnormalities that exist. Through thorough clinical evaluation, via physical findings, detailed patient history, and advanced imaging techniques, such as angiogram, computerized tomography (CT scan), magnetic resonance imaging (MRI), or more rarely transillumination after birth are the most accurate diagnostic techniques.[3] However, diagnostic literature fails to provide a clear distinction between severe obstructive hydrocephalus and hydranencephaly, leaving some children with an unsettled diagnosis.[7]
Preliminary diagnosis may be made in utero via standard ultrasound, and can be confirmed with a standard anatomy ultrasound. This sometimes proves to provide a misdiagnosis of differential diagnoses including bilaterally symmetric schizencephaly (a less destructive developmental process on the brain), severe hydrocephalus (cerebrospinal fluid excess within the skull), and alobar holoprosencephaly (a neurological developmental anomaly). Once destruction of the brain is complete, the cerebellum, midbrain, thalami, basal ganglia, choroid plexus, and portions of the occipital lobes typically remain preserved to varying degrees. Though the cerebral cortex is absent, in most cases the fetal head remains enlarged due to the continued production by the choroid plexus of cerebrospinal fluid that is inadequately reabsorbed causing increased intracranial pressure.[6]
Occurrence
This condition possesses isolated occurrences, affecting less than 1 in 10,000 births worldwide[6] and officially classifying hydranencephaly as a rare disorder by affecting fewer than 1 in 250,000 in the United States.[8]
Prognosis
There is no standard treatment for hydranencephaly. Treatment is symptomatic and supportive. Hydrocephalus may be treated with surgical treatment of a shunt, which often grants a much better prognosis and greater quality of life.[9]
The prognosis for children with hydranencephaly is generally quite poor. Death often occurs in the first year of life,[10] but other children may live several years. The oldest known person living with hydranencephaly is 33 years old (as of August 2013).[11]
Medical text identifies that hydranencephalic children simply have only their brain stem function remaining, thus leaving formal treatment options as symptomatic and supportive.[6] Severe hydrocephalus causing macrocephaly, a larger than average head circumference, can easily be managed by placement of a shunt[4] and often displays a misdiagnosis of another lesser variation of cephalic condition due to the blanketing nature of hydrocephalus.[6] Plagiocephaly, the asymmetrical distortion of the skull, is another typical associated condition that is easily managed through positioning and strengthening exercises to prevent torticollis, a constant spasm or extreme tightening of the neck muscles.
References
- ↑ Kandel, Eric R. (2013). Principles of neural science (5. ed.). Appleton and Lange: McGraw Hill. p. 1020. ISBN 978-0-07-139011-8.
- ↑ http://www.disabled-world.com/health/neurology/hydranencephaly.php
- 1 2 3 National Organization for Rare Disorders. "Hydranencephaly". Rare Diseases Information.
- 1 2 National Institute of Neurological Conditions and Stroke, NINDS. "Hydranencephaly Information Page". Disorders.
- ↑ Ulmer S, Moeller F, Brockmann MA, Kuhtz-Buschbeck JP, Stephani U, Jansen O (2005). "Living a normal life with the nondominant hemisphere: magnetic resonance imaging findings and clinical outcome for a patient with left-hemispheric hydranencephaly". Pediatrics 116 (1): 242–5. doi:10.1542/peds.2004-0425. PMID 15995064.
- 1 2 3 4 5 Kurtz & Johnson, Alfred & Pamela. "Case Number 7: Hydranencephaly". Radiology, 210, 419-422.
- 1 2 Dubey, AK Lt Col. "Is it Hydranencephaly-A Variant?" (PDF). MJAFI 2002; 58:338-339. Retrieved 2011.
- ↑ Rare Disease Day: February 28. "What is a Rare Disease?". Rare Disease. Retrieved 2011.
- ↑ "Everything Guide to Children with Hydranencephaly" by Brayden Alexander Global Foundation for Hydranencephaly, Incorporated.
- ↑ McAbee GN, Chan A, Erde EL (2000). "Prolonged survival with hydranencephaly: report of two patients and literature review". Pediatr. Neurol. 23 (1): 80–4. doi:10.1016/S0887-8994(00)00154-5. PMID 10963978.
- ↑ Global Hydranencephaly Foundation Family-to-Family Resource Network database
See also
External links
- Brayden Alexander Global Foundation for Hydranencephaly, Incorporated; dba Global Hydranencephaly Foundation
- Journey of the Bees: Global Hydranencephaly Foundation
- International Hydranencephaly Support Group
- Hydranencephaly at NINDS
| ||||||||||||||||||||||