Gut–brain axis
The gut–brain axis refers to the biochemical signaling taking place between the gastrointestinal tract and the nervous system, often involving intestinal microbiota,[1] which have been shown to play an important role in healthy brain function.[2][3]
The gut microbiota communicates with the central nervous system through different pathways (neural, immune and endocrine) and influences the brain, more specifically its function and its behaviour. Several studies have shown that the gut microbiota is involved in the regulation of anxiety, pain, cognition and mood. These studies used germ free animals compared to normal animals, which were later exposed to pathogenic bacterial infections, probiotic bacteria and antibiotic drugs. The gut-brain axis is an emerging concept that could be helpful for developing new therapeutic strategies for complex central nervous system disorders by modifying the gut microbiota.[4]
Brain function

Research suggests that the gut–brain axis, a bidirectional neurohumoral communication system in the human body, functions as a pathway for the gut microbiota to modulate brain function of its host. The postnatal microbial colonization of the gastrointestinal tract results in a long-lasting impact on the neural processing of sensory information regarding the hypothalamic-pituitary-adrenal axis stress response. Early postnatal bacterial colonization in germ free (GF) mice contribute the development of central nervous system. A recent study showed that mice whose diets were supplemented with the Bifidobacterium breve show elevated concentrations of fatty acids in the brain, including arachidonic acid and docosahexaenoic acid, which are known to play important roles in neurodevelopmental processes, including neurogenesis.[5] The c-Fos activation in the paraventricular nucleus was rapidly induced by the inoculation of Bifidobacterium infantis. Tryptophan metabolism was modulated by B. infantis, suggesting that the normal gut microbiota can influence the precursor pool for serotonin, which is correlated to neurophysiological behavior. Anxiety-like behavior and central neurochemical changes were relieved in GF mice compared with specific pathogen free (SPF) mice.
In addition, organisms from the bacterial genus Clostridium were found at an elevated level in the stools of children with autism compared to the stools of the children without.[6]
Brain development and behavior
It has been shown that colonization by gut microbiota impacts mammalian brain development by initiating signaling mechanisms that affect neuronal circuits involved in motor control and anxiety behavior. Using measures of motor activity and anxiety-like behavior, scientists demonstrate that GF mice display increased motor activity and reduced anxiety, compared with SPF mice with a normal gut microbiota. This behavioral phenotype is associated with altered expression of genes known to be involved in second messenger pathways and synaptic long-term potentiation in brain regions implicated in motor control and anxiety-like behavior. [7]
Behavioral phenotype
During birth, the microbial colonization contributes to the development of epithelial barrier function, gut homeostasis, angiogenesis, innate adaptive immune function, and common neuro-developmental disorders (autism, schizophrenia). Compared to the SPF mice, the GF mice illustrated increased motor activity, reduced anxiety-like behavior, altered expression of synaptic plasticity-related genes, elevated noradrenaline, dopamine, and 5-hydroxytryptamine turnover in the striatum (The striate nucleus is part of the cerebrum of the brain and is involved in a number of different cognitive processes). When SPF mice are exposed to antibiotics, gastrointestinal infections and stress, sharp changes in diet, the gut homeostasis and the central nervous system becomes imbalanced, therefore antibiotic drugs suggest a role for the gut microbiota in the regulation of anxiety, mood, cognition and pain.
Visceral pain
Visceral pain can happen in the gut because of gastrointestinal disorders, such as Irritable Bowel Syndrome (IBS).[8] The perception of visceral pain involves sensory nerves on a peripheral sensitization and cortical and sub-cortical pathways on a central level. In addition, there is substantial overlap in the brain areas underlying visceral pain and those that are involved in the processing of psychological stress. Imaging studies in humans with IBS [9][10] and in animal models [11][12] have shown increased activation of the same brain area. Clinically, it has been shown that visceral pain perception can be affected by intestinal microbiota. For example, Lactobacilli and Bifidobacteria can reduce visceral pain induced by stress and IBS,[13][14][15] in humans and mice, and many different probiotics have been shown to have beneficial effects in humans with abdominal pain.[16][17]
Stress
Some probiotics can apparently help reduce anxiety, stress, and mood of patients with IBS and chronic fatigue, but the mechanisms of action of such effects currently remain unclear and may involve a combination of neural, immune and endocrine effects. Lactobacillus reuteri, probiotic, is known to modulate the immune system, decrease anxiety, and reduce the stress-induced increase of corticosterone. Other probiotics can lower inflammatory cytokines, decrease oxidative stress, and improve nutritional status.[6]
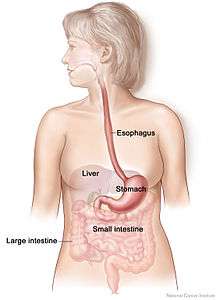
Gut–brain–liver axis
The liver plays a dominant role in blood glucose homeostasis by maintaining a balance between the uptake and storage of glucose through the metabolic pathways of glycogenesis and gluconeogenesis. In recent studies, it is illustrated that intestinal lipids regulate glucose homeostasis involving a gut-brain-liver axis. The direct administration of lipids into the upper intestine increases the long chain fatty acyl-coenzyme A (LCFA-CoA) levels in the upper intestines and suppresses glucose production even under sub diaphragmatic vagotomy or gut vagal deafferentation. This interrupts the neural connection between the brain and the gut and blocks the upper intestinal lipids’ ability to inhibit glucose production. The gut-brain-liver axis and gut microbiota composition can regulate the glucose homeostasis in the liver and provide potential therapeutic methods to treat obesity and diabetes.[6]
See also
References
- ↑ Montiel-Castro, A. J.; González-Cervantes, R. M.; Bravo-Ruiseco, G.; Pacheco-López, G. (2013). "The microbiota-gut-brain axis: Neurobehavioral correlates, health and sociality". Frontiers in Integrative Neuroscience 7. doi:10.3389/fnint.2013.00070.
- ↑ Foster, J. A.; McVey Neufeld, K. A. (2013). "Gut–brain axis: How the microbiome influences anxiety and depression". Trends in Neurosciences 36 (5): 305–312. doi:10.1016/j.tins.2013.01.005. PMID 23384445.
- ↑ Cryan, J. F.; Dinan, T. G. (2012). "Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour". Nature Reviews Neuroscience 13 (10): 701–712. doi:10.1038/nrn3346. PMID 22968153.
- ↑ Cryan, John F.; Dinan, Timothy G. (2012). "Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour". Nature Reviews Neuroscience 13: 701–12. doi:10.1038/nrn3346. PMID 22968153.
- ↑ Innis, S. M. (2007). "Dietary (n-3) fatty acids and brain development". J. Nutr 137: 855–859.
- 1 2 3 "The role of gut microbiota in the gut-brain axis: current challenges and perspectives.". Protein Cell 4: 403–14. Jun 2013. doi:10.1007/s13238-013-3017-x. PMID 23686721.
- ↑ Rochellys diaz Heijtz,Shugui Wang, Sven Patterson "Normal gut microbiota modulates brain development and behavior" PNAS (2011): PMCID: PMC3041077
- ↑ John F. Cryan and Timothy G. Dinan, "Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour" Nature Reviews Neuroscience (2012) : 10.1038/nrn3346
- ↑ Mayer, E. A.; et al. (2008). "Functional gastrointestinal disorders: from animal models to drug development". Gut 57: 384–404. doi:10.1136/gut.2006.101675.
- ↑ Mertz, H. et al. Regional cerebral activation in irritable bowel syndrome and control subjects with painful and nonpainful rectal distention. 842–848 (2000)
- ↑ Gibney, S. M.; Gosselin, R. D.; Dinan, T. G.; Cryan, J. F. (2010). "Colorectal distension-induced prefrontal cortex activation in the Wistar–Kyoto rat: implications for irritable bowel syndrome". Neuroscience 165: 675–683. doi:10.1016/j.neuroscience.2009.08.076.
- ↑ Wang, Z.; et al. (2008). "Regional brain activation in conscious, nonrestrained rats in response to noxiousstimulation". Pain 138: 233–243. doi:10.1016/j.pain.2008.04.018.
- ↑ Verdu, E. F.; et al. (2006). "Specific probiotic therapy attenuatesantibiotic induced visceral hypersensitivity in mice". Gut 55: 182–190. doi:10.1136/gut.2005.066100.
- ↑ Gareau, M. G.; Jury, J.; MacQueen, G.; Sherman, P. M.; Perdue, M. H. (2007). "Probiotic treatment of rat pups normalises corticosterone release and ameliorates colonic dysfunction induced by maternal separation". Gut 56: 1522–1528. doi:10.1136/gut.2006.117176.
- ↑ McKernan, D. P.; Fitzgerald, P.; Dinan, T. G.; Cryan, J. F. (2010). "The probiotic Bifidobacterium infantis 35624 displays visceral antinociceptive effects in the rat". Neurogastroenterol. Motil 22: 1029–1035. doi:10.1111/j.1365-2982.2010.01520.x.
- ↑ Bercik, P.; Collins, S. M.; Verdu, E. F. (2012). "Microbes and the gut–brain axis". Neurogastroenterol. Motil 24: 405–413. doi:10.1111/j.1365-2982.2012.01906.x.
- ↑ Clarke, G.; Cryan, J. F.; Dinan, T. G.; Quigley, E. M. (2012). "Review article: probiotics for the treatment of irritable bowel syndrome — focus on lactic acid bacteria". Aliment. Pharmacol. Ther 35: 403–413. doi:10.1111/j.1365-2036.2011.04965.x.
- "Immune adaptations that maintain homeostasis with the intestinal microbiota.". Nat Rev Immunol 10: 159–69. Mar 2010. doi:10.1038/nri2710. PMID 20182457..
- "Commensal host-bacterial relationships in the gut". Science 292: 1115–8. May 2001. doi:10.1126/science.1058709. PMID 11352068..
- "Temperature gradient gel electrophoresis analysis of 16S rRNA from human fecal samples reveals stable and host-specific communities of active bacteria.". Appl Environ Microbiol 64: 3854–9. Oct 1998. PMID 9758810..
- "Review article: the current pharmacological therapies for hepatic encephalopathy.". Aliment Pharmacol Ther. 25 Suppl 1: 23–31. Feb 2007. doi:10.1111/j.1746-6342.2006.03218.x. PMID 17295849..
- Rochellys diaz Heijtz,Shugui Wang, Sven Patterson "Normal gut microbiota modulates brain development and behavior" PNAS (2011): PMCID: PMC3041077.
- "Differences between the gut microflora of children with autistic spectrum disorders and that of healthy children.". J Med Microbiol 54: 987–91. Oct 2005. doi:10.1099/jmm.0.46101-0. PMID 16157555..
- Sandler, RH; Finegold, SM; Bolte, ER; et al. (2000). "Short-term benefit from oral vancomycin treatment of regressive-onset autism". J Child Neurol 15: 429–35. doi:10.1177/088307380001500701. PMID 10921511.
- "Antibiotic-induced psychosis: a link to D-alanine?". Med Hypotheses 75: 676–7. Dec 2010. doi:10.1016/j.mehy.2010.07.021. PMID 20691544..
- "Immune-mediated neural dysfunction in a murine model of chronic Helicobacter pylori infection.". Gastroenterology 123: 1205–15. Oct 2002. doi:10.1053/gast.2002.36024. PMID 12360482..
- "Role of gut-brain axis in persistent abnormal feeding behavior in mice following eradication of Helicobacter pylori infection.". Am J Physiol Regul Integr Comp Physiol 296: R587–94. Mar 2009. doi:10.1152/ajpregu.90752.2008. PMID 19129375..
- Chen, X; D'Souza, R; Hong, ST (2013). "The role of gut microbiota in the gut-brain axis: current challenges and perspectives". Protein & Cell 4 (6): 403–14. doi:10.1007/s13238-013-3017-x. PMID 23686721.
- "Impact of the gut microbiota on the development of obesity and type 2 diabetes mellitus.". Front Microbiol 5: 190. 2014. doi:10.3389/fmicb.2014.00190. PMID 24808896..