Gender disparities in health
| Part of a series on | ||||||||
| Feminism | ||||||||
|---|---|---|---|---|---|---|---|---|
|
History
|
||||||||
|
||||||||
|
Concepts
|
||||||||
|
Lists and categories
|
||||||||
| Feminism portal | ||||||||
Health is the general condition of a person's mind and body, usually indicating the state of being free from illness, injury or pain.[1] The World Health Organization (WHO) has defined health as "a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity."[2] Identified by the 2012 World Development Report as one of two key human capital endowments, health can influence an individual’s ability to reach his or her full potential in society.[3] Yet while gender equality has made the most progress in areas such as education and labor force participation, health inequality between men and women continues to plague many societies today. While both males and females face health disparities, girls and women experience a majority of health disparities. This comes from the fact that many cultural ideologies and practices have structured society in a way whereby women are more vulnerable to abuse and mistreatment, making them more prone to illnesses and early death.[4] Women are also restricted from receiving many opportunities, such as education and paid labor, that can help improve their accessibility to better health care resources.
Definition of health disparity
Health disparity has been defined by the World Health Organization as the differences in health care received by different groups of people that are not only unnecessary and avoidable but also unfair and unjust.[5] The existence of health disparity implies that health equity does not exist in many parts of the world. Equity in health refers to the situation whereby every individual has a fair opportunity to attain their full health potential, and that no one should be denied from achieving this potential.[5] Overall, the term "health disparities," or "health inequalities," is widely understood as the differences in health between people who are situated at different positions in a socioeconomic hierarchy.[6]
Gender as an axis of difference
Predominantly female-bias
The social structures of many of these places perpetuate the marginalization and oppression of women in the form of cultural norms and legal codes. As a result of this unequal social order, women are usually relegated into positions where they are not only more vulnerable to suffering from health problems, but also less able to have access and control over healthcare resources than men. For example, women living in areas with a patriarchal system are often less likely to receive tertiary education or to be employed in the paid labor market due to gender discrimination.[4] As a result, female life expectancy at birth and nutritional well-being, and immunity against communicable and non-communicable diseases, are often lower than those of men.[7][8]
Disparities against males
While a majority of the global health gender disparities is weighted against women, there are situations in which men tend to fare poorer. One such instance is armed conflicts, where men are often the immediate victims. A study of conflicts in 13 countries from 1955 to 2002 found that 81% of all violent war deaths were male.[3] Apart from armed conflicts, areas with high incidence of violence, such as regions controlled by drug cartels, also see men experiencing higher mortality rates. This stems from social beliefs that associate ideals of masculinity with aggressive, confrontational behavior.[9] Lastly, sudden and drastic changes in economic environments and the loss of social safety nets, in particular social subsidies and food stamps, have also been linked to higher levels of alcohol consumption and psychological stress among men, leading to a spike in male mortality rates. This is because such situations often makes it harder for men to provide for their family, a task that has been long regarded as the "essence of masculinity."[10]
In developed countries, overall health outcomes (such as life expectancy) are worse for men than women.
Forms of gender disparities
Male-female sex ratio
|
Countries with more females than males.
Countries with the same number of males and females.
Countries with more males than females.
No data |
At birth, boys outnumber girls with the ratio of 105 or 106 male to 100 female children.[8] However, after conception, biology favors women. Research has shown that if men and women received similar nutrition, medical attention, and general health care, women would live longer than men.[11] This is because women, on a whole, are more resistant to diseases and less prone to debilitating genetic conditions.[12] However, despite medical and scientific research that shows that when given the same care as males, females tend to have better survival rates than males, the ratio of women to men in developing regions such as South Asia, West Asia, and China can be as low as 0.94, or even lower. This deviation from the natural male to female sex ratio has been described by Indian philosopher and economist Amartya Sen as the "missing women" phenomenon.[8] According to the 2012 World Development Report, the number of missing women is estimated to be about 1.5 million women per year, with a majority of the women missing in India and China.[3]
Female mortality
In many developing regions, women experience high levels of mortality.[13] Many of these deaths result from maternal mortality and HIV/AIDS infection. Although only 1,900 maternal deaths were recorded in high-income nations in 2008, India and Sub-Saharan Africa experienced a combined total of 266,000 deaths from pregnancy-related causes. In Somalia and Chad, one in every 14 women die from causes related to child birth.[3] In addition, the HIV/AIDS epidemic also contributes significantly to female mortality. The case is especially true for Sub-Saharan Africa, where women account for 60% of all adult HIV infections.[14]
Health outcome
Women tend to have poorer health outcomes than men for several reasons ranging from sustaining greater risk to diseases to experiencing higher mortality rates. In the Population Studies Center Research Report by Rachel Snow that compares the disability-adjusted life years (DALY) of both male and females, the global DALYs lost to females for sexually transmitted diseases such as gonorrhea and chlamydia are more than ten times greater than those of the males.[15] Moreover, the female DALYs to male DALYs ratio for malnutrition-related diseases such as Iron-Deficiency Anemia are often close to 1.5, suggesting that poor nutrition impacts women at a much higher level than men.[15] Additionally, in terms of mental illnesses, women are also two to three times more likely than men to be diagnosed with depression.[16] With regards to suicidal rates, up to 80% of those who committed suicide or attempted suicide in Iran are women.[17]
In developed countries with more social and legal gender equality, overall health outcomes can disfavor men. For example, in the United States, as of 2001, men's life expectancy is 5 years lower than women's (down from 1 year in 1920), and men die at higher rates from all top 10 causes of death, especially heart disease and stroke.[18] Men die from suicide more frequently, though women more frequently have suicidal thoughts and the suicide attempt rate is the same for men and women (see Gender differences in suicide). Men may suffer from undiagnosed depression more frequently, due to gender differences in the expression of emotion.[19] American men are more likely to consume alcohol, smoke, engage in risky behaviors, and defer medical care.[20]
Incidence of melanoma has strong gender-related differences which vary by age.[21]
Access to healthcare
Women tend to have poorer access to health care resources than men. In certain regions of Africa, many women often lack access to malaria treatment as well as access to resources that could protect them against Anopheles mosquitoes during pregnancy. As a result of this, pregnant women who are residing in areas with low levels of malaria transmission are still placed at two to three times higher risk than men in terms of contracting a severe malaria infection.[22] These disparities in access to healthcare are often compounded by cultural norms and expectations imposed on women. For example, certain societies forbid women from leaving their homes unaccompanied by a male relative, making it harder for women to receive healthcare services and resources when they need it most.[4]
Gender factors, such as women’s status and empowerment (i.e., in education, employment, intimate partner relationships, and reproductive health), are linked with women’s capacity to access and use maternal health services, a critical component of maternal health.[23] Still, family planning is typically viewed as the responsibility of women, with programs targeting women and overlooking the role of men—even though men’s dominance in decision making, including contraceptive use, has significant implications for family planning [24] and access to reproductive health services.[25][26]
In order to promote equity in access to reproductive health care, health programs and services should conduct analyses to identify gender inequalities and barriers to health, and determine the programmatic implications. The analyses will help inform decisions about how to design, implement, and scale up health programs that meet the differential needs of women and men.[26][27]
Causes
Cultural norms and practices
Cultural norms and practices are two of the main reasons why gender disparities in health exist and continue to persist. These cultural norms and practices often influence the roles and behaviors that men and women adopt in society. It is these gender differences between men and women, which are regarded and valued differently, that give rise to gender inequalities as they work to systematically empower one group and oppress the other. Both gender differences and gender inequalities can lead to disparities in health outcomes and access to health care. Some of the examples provided by the World Health Organization of how cultural norms can result in gender disparities in health include a woman's inability to travel alone, which can prevent them from receiving the necessary health care that they need.[28] Another societal standard is a woman's inability to insist on condom use by her spouse or sex partners, leading to a higher risk of contracting HIV.[28]
Son preference
One of the better documented cultural norms that augment gender disparities in health is the preference for sons.[29][30] In India, for instance, the 2001 census recorded only 93 girls per 100 boys. This is a sharp decline from 1961, when the number of girls per 100 boys was nearly 98.[4] In certain parts of India, such as Kangra and Rohtak the number of girls for every 100 boys can be as low as in the 70s.[31] Additionally, low female to male numbers have also been recorded in other Asian countries – most notably in China where, according to a survey in 2005, only 84 girls were born for every 100 boys. Although this was a slight increase from 81 during 2001–2004, it is still much lower than the 93 girls per 100 boys in the late 1980s.[4] The increasing number of unborn girls in the late 20th century has been attributed to technological advances that made pre-birth sex determination, also known as prenatal sex discernment, such as the ultrasound test more affordable and accessible to a wider population. This allowed parents who prefer a son to determine the sex of their unborn child during the early stages of pregnancy. By having early identification of their unborn child's sex, parents could practice sex-selective abortion, where they would abort the fetus if it was not the preferred sex, which in most cases is that of the female.[3]
Additionally, the culture of son preference also extends beyond birth in the form of preferential treatment of boys.[32] This preferential care can be manifested in many ways, such as through differential provision of food resources, attention, and medical care. Data from household surveys over the past 20 years has indicated that the female disadvantage has persisted in India and may have even worsened in some other countries such as Nepal and Pakistan.[3]
Female genital mutilation
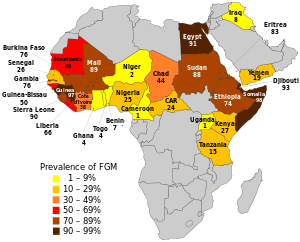
Harmful cultural practices such as female genital mutilation (FGM) also cause girls and women to face health risks. Millions of females are estimated to have undergone FGM, which involves partial or total removal of the external female genitalia for non-medical reasons. It is estimated that 92.5 million females over 10 years of age in Africa are living with the consequences of FGM. Of these, 12.5 million are girls between 10 and 14 years of age. Each year, about three million girls in Africa are subjected to FGM.[28]
Often performed by traditional practitioners using unsterile techniques and devices, FGM can have both immediate and late complications.[33][34] These include excessive bleeding, urinary tract infections, wound infection, and in the case of unsterile and reused instruments, hepatitis and HIV.[33] In the long run, scars and keloids can form, which can obstruct and damage the urinary and genital tracts. According to a 2005 UNICEF report on FGM, it is unknown how many girls and women die from the procedure because of poor record keeping and a failure to report fatalities.[35] FGM may also complicate pregnancy and place women at a higher risk for obstetrical problems, such as prolonged labor.[33] According to a 2006 study by the WHO involving 28,393 women, neonatal mortality increases when women have experienced FGM; an additional ten to twenty babies were estimated to die per 1,000 deliveries.[36]
Psychological complications are related to cultural context. Women who undergo FGM might be emotionally affected when they move outside their traditional circles and are confronted with the view that mutilation is not the norm.[33]
Violence and abuse

Violence against women is a widespread global occurrence with serious public health implications. This is a result of social and gender bias.[37] Many societies in developing nations function on a patriarchal framework, where women are often viewed as a form of property and as socially inferior to men. This unequal standing in the social hierarchy has led women to be physically, emotionally, and sexually abused by men, both as children and adults. These abuses usually constitute some form of violence. Although children of both sexes do suffer from physical maltreatment, sexual abuse, and other forms of exploitation and violence, studies have indicated that young girls are far more likely than boys to experience sexual abuse. In a 2004 study on child abuse, 25.3% of all girls surveyed experienced some form of sexual abuse, a percentage that is three times higher than that of boys (8.7%).[38]
Such violence against women, especially sexual abuse, is increasingly being documented in areas experiencing armed conflicts. Presently, women and girls bear the brunt of social turmoil worldwide, making up an estimated 65% of the millions who are displaced and affected.[39] Some of these places which are facing such problems include Rwanda, Kosovo, and the Democratic Republic of the Congo.[39] This comes as a result of both the general instability around the region, as well as a tactic of warfare to intimidate enemies. Often being placed in emergency and refugee settings, girls and women alike are highly vulnerable to abuse and exploitation by military combatants, security forces, and members of rival communities.[38]
The sexual violence and abuse of both young and adult women have both short and long-term consequences, contributing significantly to a myriad of health issues into adulthood. These range from debilitating physical injuries, reproductive health issues, substance abuse, and psychological trauma. Examples of the above categories include depression and post-traumatic stress disorder, alcohol and drug use and dependence, sexually transmitted diseases, and suicide attempts.[39]
Abused women often have higher rates of unplanned and problematic pregnancies, abortions, neonatal and infant health issues, sexually transmitted infections (including HIV), and mental disorders (such as depression, anxiety disorders, sleep disorders and eating disorders) as compared to their non-abused peers.[3] During peacetime, most violence against women is perpetrated by either male individuals whom them know or intimate male partners. An eleven-country study conducted by WHO between 2000 and 2003 found that, depending on the country, between 15% and 71% of women have experienced physical or sexual violence by a husband or partner in their lifetime, and 4% to 54% within the previous year.[40] Partner violence may also be fatal. Studies from Australia, Canada, Israel, South Africa and the United States show that between 40% and 70% of female murders were carried out by intimate partners.[41]
Other forms of violence against women include sexual harassment and abuse by authority figures (such as teachers, police officers or employers), trafficking for forced labour or sex, and traditional practices such as forced child marriages and dowry-related violence. At its most extreme, violence against women can result in female infanticide and violent death. Despite the size of the problem, many women do not report their experience of abuse and do not seek help. As a result, violence against women remains a hidden problem with great human and health-care costs.[37]
Poverty
Poverty is another factor that facilitates the continual existence of gender disparities in health.[3] Poverty often works in tandem with various cultural norms to indirectly impact women's health. While many communities and households are not opposed to helping women attain better health through education, better nutrition, and financial stability, poverty often act as a form of barrier against gender equity in health for women. Oftentimes, due to financial constraints and limited capital, only a select few are able to receive opportunities, like education and employment, that might help them attain better health outcomes. However, cultural norms would often prioritized men in receiving these opportunities. This prioritization of males stems from the societal perception that the potential returns to both the household and the community is higher for men than women.[42]
Healthcare system
The World Health Organization defines health systems as "all the activities whose primary purpose is to promote, restore, or maintain health".[43] However, factors outside of healthcare systems can influence the impact healthcare systems have on the health of different demographics within a population. This is because healthcare systems are known to be influenced by social, cultural and economic frameworks. As a result, health systems are regarded as not only "producers of health and health care", but also as "purveyors of a wider set of societal norms and values," many of which are biased against women[44]
In the Women and Gender Equity Knowledge Network's Final Report to the WHO Commission on Social Determinants of Health in 2007, health systems in many countries were noted to have been unable to deliver adequately on gender equity in health. One explanation for this issue is that many healthcare systems tend to neglect the fact that men and women’s health needs can be very different.[45] In the report, studies have found evidence that the healthcare system can promote gender disparities in health through the lack of gender equity in terms of the way women are regarded - as both consumers (users) and producers (carers) of health care services.[45] For instance, healthcare systems tend to regard women as objects rather than subjects, where services are often provided to women as a means of something else rather on the well-being of women.[45] In the case of reproductive health services, these services are often provided as a form of fertility control rather than as care for women's well-being.[46] Additionally, although the majority of the workforce in health care systems are female, many of the working conditions remain discriminatory towards women. Many studies have shown that women are often expected to conform to male work models that ignore their special needs, such as childcare or protection from violence.[47] This significantly reduces the ability and efficiency of female caregivers providing care to patients, particularly female ones.[48][49]
Structural gender oppression
Structural gender inequalities in the allocation of resources, such as income, education, health care, nutrition and political voice, are strongly associated with poor health and reduced well-being. Very often, such structural gender discrimination of women in many other areas has an indirect impact on women's health. For example, because women in many developing nations are less likely to be part of the formal labor market, they often lack access to job security and the benefits of social protection, including access to health care. Additionally, within the formal workforce, women often face challenges related to their lower status, where they suffer workplace discrimination and sexual harassment. Studies have shown that this expectation of having to balance the demands of paid work and work at home often give rise to work-related fatigue, infections, mental ill-health and other problems, which results in women faring poorer in health.[50]
Women’s health is also put at a higher level of risk as a result of being confined to certain traditional responsibilities, such as cooking and water collection. Being confined to unpaid domestic labor not only reduces women's opportunities to education and formal job employment (both of which can indirectly contribute to better health in the long run), but also potentially expose women to higher risk of health issues. For instance, in developing regions where solid fuels are used for cooking, women are exposed to a higher level of indoor air pollution due to extended periods of cooking and preparing meals for the family. Breathing air tainted by the burning of solid fuels is estimated to be responsible for 641,000 of the 1.3 million deaths of women worldwide each year due to chronic obstructive pulmonary disorder (COPD).[51]
In some settings, structural gender inequity is associated with particular forms of violence, marginalization, and oppression against females. This includes violent assault by men, child sexual abuse, strict regulation of women's behavior and movement, female genital mutilation, and exploitative, forced labor.[4] Women and girls are also vulnerable to less well-documented forms of abuse or exploitation, such as human trafficking or "honor killings" for perceived behavioral transgressions and deviation of their social roles. These acts are associated with a wide range of health problems in women such as physical injuries, unwanted pregnancies, abortions, mental disorders such as depression, and anxiety, substance abuse, and sexually transmitted infections, all of which can potentially lead to premature death.[52][53]
The ability of women to utilize health care is also heavily influenced by other forms of structural gender inequalities. These include unequal restriction on one’s mobility and behavior, as well as unequal control over financial resources. Many of these social gender inequalities can impact the way women’s health is regarded, which can in turn determine the level of access women have to healthcare services and the extent by which households and the larger community are willing to invest in women’s health issues.[45]
Other axes of oppression

Apart from gender discrimination, other axes of oppression also exist in society to further marginalize certain groups of women, especially those who are living in poverty or of minority status in which they live.[4]
Race and ethnicity
Race is a well known axis of oppression, where people of color tend to suffer more from structural violence. For people of color, race can serve as a factor, in addition to gender, that can further influence one's health negatively.[54] Studies have shown that in both high-income and low-income countries, levels of maternal mortality may be up to three times higher among women of disadvantaged ethnic groups than among white women. In a study on race and mother-death within the USA, the maternal mortality rate for African Americans is close to four times higher than that of white women. Similarly in South Africa, the maternal mortality rate for black/African women and women of color is approximately 10 and 5 times greater respectively than that of white/European women.[55]
Socioeconomic status
Although women around the world share many similarities in terms of the health-impacting challenges, there are also many distinct differences that arise from their varying states of socioeconomic conditions. The type of living conditions in which women live is largely associated with not only their own socioeconomic status, but also that of their nation.[4]
At every single age category, women in high income countries tend to live longer and are less likely to suffer from ill health than and premature mortality than those in low income countries. Death rates in high-income countries are also very low among children and younger women, where most deaths occur after the age of 60 years. In low-income countries however, the death rates at young ages are much higher, with most death occurring among girls, adolescents, and younger adult women. Data from 66 developing countries show that child mortality rates among the poorest 20% of the population are almost double those in the top 20%. [56] The most striking health outcome difference between rich and poor countries is maternal mortality. Presently, an overwhelming proportion of maternal mortality is concentrated within the nations that are suffering from poverty or some other form of humanitarian crises, where 99% of the more than half a million maternal deaths every year occur. This comes from the fact that institutional structures which could protect women's health and well-being are either lacking or poorly developed in these places.[4]
The situation is similar within countries as well, where the health of both girls and women is critically affected by social and economic factors. Those who are living in poverty or of lower socioeconomic status tend to perform poorly in terms of health outcomes. In almost all countries, girls and women living in wealthier households experience lower levels of mortality and higher usage of health-care services than those living in the poorer households. Such socioeconomic status-related health disparities is present in every nation around the world, including developed regions.[4]
Management
The Fourth World Conference on Women asserts that men and women share the same right to the enjoyment of the highest attainable standard of physical and mental health.[57] However, women are disadvantaged due to social, cultural, political and economic factors that directly influence their health and impede their access to health-related information and care.[4] In the 2008 World Health Report, the World Health Organization stressed that strategies to improve women’s health must take full account of the underlying determinants of health, particularly gender inequality. Additionally, specific socioeconomic and cultural barriers that hamper women in protecting and improving their health must also be addressed.[58]
Gender mainstreaming

Gender mainstreaming was established as a major global strategy for the promotion of gender equality in the Beijing Platform for Action from the Fourth United Nations World Conference on Women in Beijing in 1995.[59] Gender mainstreaming is defined by the United Nations Economic and Social Council in 1997 as follows:
“Mainstreaming a gender perspective is the process of assessing the implications for women and men of any planned action, including legislation, policies or programmes, in all areas and at all levels. It is a strategy for making women’s as well as men’s concerns and experiences an integral dimension of the design, implementation, monitoring and evaluation of policies and programmes in all political, economic and societal spheres so that women and men benefit equally and inequality is not perpetuated. The ultimate aim is to achieve gender equality.”[59]
Over the past few years, "gender mainstreaming" has become a preferred approach for achieving greater health parity between men and women. It stems from the recognition that while technical strategies are necessary, they are not sufficient in alleviating gender disparities in health unless the gender discrimination, bias and inequality that in organizational structures of governments and organizations – including health systems - are being challenged and addressed.[4] The gender mainstreaming approach is a response to the realisation that gender concerns must be dealt with in every aspect of policy development and programming, through systematic gender analyses and the implementation of actions that address the balance of power and the distribution of resources between women and men.[60] In order to address gender health disparities, gender mainstreaming in health employs a dual focus. First, it seeks to identify and address gender-based differences and inequalities in all health initiatives; and second, it works to implement initiatives that address women’s specific health needs that are a result either of biological differences between women and men (e.g. maternal health) or of gender-based discrimination in society (e.g. gender-based violence; poor access to health services).[61]
Sweden’s new public health policy, which came into force in 2003, has been identified as an key example of mainstreaming gender in health policies. According to the World Health Organization, Sweden’s public health policy is designed to address not only the broader social determinants of health, but also the way in which gender is woven into the public health strategy.[61][62][63] The policy specifically highlights its commitment to address and reduce gender-based inequalities in health.[64]
Female Empowerment
The United Nations has identified the enhancement of women's involvement as way to achieve gender equality in the realm of education, work, and health.[65] This is because women play critical roles as caregivers, formally and informally, in both the household and the larger community. Within the United States, an estimated 66% of all caregivers are female, with one-third of all female caregivers taking care of two or more people[66] According to the World Health Organization, it is important that approaches and frameworks that are being implemented to address gender disparities in health acknowledge the fact that majority of the care work is provided by women.[4] A meta-analysis of 40 different women's empowerment projects found that increased female participation have led to a broad range of quality of life improvements. These improvements include increases in women's advocacy demands and organization strengths, women-centered policy and governmental changes, and improved economic conditions for lower class women.[67]
In Nepal, a community-based participatory intervention to identify local birthing problems and formulating strategies has been shown to be effective in reducing both neonatal and maternal mortality in a rural population.[68] Community-based programs in Malaysia and Sri Lanka that used well-trained midwives as front-line health workers also produced rapid declines in maternal mortality.[69]
References
- ↑ "Health - Definition and More from the Free Merriam-Webster Dictionary". Merriam Webster. Retrieved 7 Apr 2013.
- ↑ World Health Organization (2006). Constitution of the World Health Organization - Basic Documents, Forty-fifth edition (PDF) (Report). Retrieved 7 Apr 2013.
- 1 2 3 4 5 6 7 8 The World Bank (2012). World Development Report 2012: Gender Equality and Development (Report). Washington, DC: The World Bank.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 World Health Organization (2009). Women & Health: Today's Evidence, Tomorrow's Agenda (PDF) (Report). WHO Press. Retrieved 18 Mar 2013.
- 1 2 Whitehead, M (1990). The Concepts and Principles of Equity in Health. (PDF) (Report). Copenhagen:
WHO, Reg. Off. Eur. p. 29. Retrieved 18 Mar 2013. line feed character in
|publisher=at position 12 (help) - ↑ Braveman, P. (2006). "Health Disparities and Health Equity: Concepts and Measurement". Annual Review of Public Health 27: 167–194. doi:10.1146/annurev.publhealth.27.021405.102103. PMID 16533114.
- ↑ Vlassoff, C (March 2007). "Gender differences in determinants and consequences of health and illness.". Journal of health, population, and nutrition 25 (1): 47–61. PMID 17615903.
- 1 2 3 Sen, Amartya (1990). "More Than 100 Million Women Are Missing". New York Review of Books.
- ↑ Márquez, Patricia (1999). The Street Is My Home: Youth and Violence in Caracas. Stanford, CA: Stanford University Press.
- ↑ Brainerd, Elizabeth; Cutler, David (2005). "Autopsy on an Empire: Understanding Mortality in Russia and the Former Soviet Union". Ann Arbor, MI: William Davidson Institute.
- ↑ Dennerstein, L; Feldman, S; Murdaugh, C; Rossouw, J; Tennstedt, S (1977). 1997 World Congress of Gerontology: Ageing Beyond 2000 : One World One Future. Adelaide: International Association of Gerontology.
- ↑ Huang, Audrey. "X chromosomes key to sex differences in health". JAMA and Archives Journals. Retrieved 25 April 2013.
- ↑ Prata, Ndola; Passano, Paige; Sreenivas, Amita; Gerdts, Caitlin Elisabeth (1 March 2010). "Maternal mortality in developing countries: challenges in scaling-up priority interventions". Women's Health 6 (2): 311–327. doi:10.2217/WHE.10.8.
- ↑ UNAIDS (2010). "Women, Girls, and HIV" UNAIDS Factsheet 10 (Report). Geneva: UNAIDS.
- 1 2 Rachel Snow (2007). Population Studies Center Research Report 07-628: Sex, Gender and Vulnerability (PDF) (Report). Population Studies Center, University of Michigan, Institute for Social Research.
- ↑ Usten, T; Ayuso-Mateos, J; Chatterji, S; Mathers, C; Murray, C (2004). "Global burden of depressive disorders in the year 2000". Br J Psychiatry 184: 386–92. doi:10.1192/bjp.184.5.386.
- ↑ Mohammadi, M. R.; Ghanizadeh, A.; Rahgozart, M.; Noorbala, A. A.; Malekafzali, H.; Davidian, H.; Naghavi, H.; Soori, H.; Yazdi, S. A. (2005). "Suicidal Attempt and Psychiatric Disorders in Iran". Suicide and Life-Threatening Behavior 35 (3): 309–316. doi:10.1521/suli.2005.35.3.309. PMID 16156491.
- ↑ http://www.webmd.com/men/features/mens-top-5-health-concerns
- ↑ http://www.webmd.com/men/features/mens-top-5-health-concerns?page=3
- ↑ https://www.nlm.nih.gov/medlineplus/menshealth.html
- ↑ https://www.aad.org/media/stats/conditions/skin-cancer
- ↑ WHO/UNICEF (2003). The Africa Malaria Report 2003 (Report). Geneva: WHO/UNICEF.
- ↑ Gill, R, DE Stewart. 2011. “Relevance of gender-sensitive policies and general health indicators to compare the status of South Asian women’s health” Women’s Health Issues 21(1): 12–18, DOI: 10.1016/j.whi.2010.10.003.
- ↑ Schuler, S., E. Rottach, and P. Mukiri. 2011. “Gender Norms and Family Planning Decision-Making in Tanzania: A Qualitative Study”. Journal of Public Health in Africa 2(2).
- ↑ Hou, X., and N. Ma. 2011. “Empowering Women: The Effect of Women's Decision-Making Power on Reproductive Health Services Uptake—Evidence from Pakistan.” World Bank Policy Research Working Paper No. 5543.
- 1 2 Rottach, E., K. Hardee, R. Jolivet, and R. Kiesel. 2012. “Integrating Gender into the Scale-Up of Family Planning and Maternal, Neonatal, and Child Health Programs.” Washington, DC: Futures Group, Health Policy Project.
- ↑ Rottach, E. 2013. “Approach for Promoting and Measuring Gender Equality in the Scale-Up of Family Planning and Maternal, Neonatal, and Child Health Programs.” Washington, DC: Futures Group, Health Policy Project.
- 1 2 3 "Gender, Women, and Health". WHO. Retrieved 17 March 2013.
- ↑ Edlund, Lena (1 December 1999). "Son Preference, Sex Ratios, and Marriage Patterns". Journal of Political Economy 107 (6, Part 1): 1275. doi:10.1086/250097.
- ↑ Das Gupta, Monica; Zhenghua, Jiang; Bohua, Li; Zhenming, Xie; Chung, Woojin; Hwa-Ok, Bae (1 December 2003). "Why is Son preference so persistent in East and South Asia? a cross-country study of China, India and the Republic of Korea". Journal of Development Studies 40 (2): 153–187. doi:10.1080/00220380412331293807.
- ↑ John, Mary E.; Kaur, Ravinder; Palriwala, Rajni; Raju, Saraswati; Sagar, Alpana (2008). Disappearing Daughters (PDF) (Report). London, UK: ActionAid. Retrieved 25 Apr 2013.
- ↑ Arnold, Fred; Choe, Minja Kim; Roy, T.K. (1 November 1998). "Son Preference, the Family-building Process and Child Mortality in India". Population Studies 52 (3): 301–315. doi:10.1080/0032472031000150486.
- 1 2 3 4 Abdulcadir, J; Margairaz, C; Boulvain, M; Irion, O (6 January 2011). "Care of women with female genital mutilation/cutting". Swiss Medical Weekly. doi:10.4414/smw.2011.13137.
- ↑ Kelly, Elizabeth; Hillard, Paula J Adams (1 October 2005). "Female genital mutilation". Current Opinion in Obstetrics and Gynecology 17 (5): 490–494. doi:10.1097/01.gco.0000183528.18728.57.
- ↑ UNICEF (2005). Changing a Harmful Social Convention: Female Genital Mutilation/Cutting (Report). Florence, Italy: Innocenti Digest/UNICEF.
- ↑ "Female genital mutilation and obstetric outcome: WHO collaborative prospective study in six African countries". The Lancet 367 (9525): 1835–1841. 1 June 2006. doi:10.1016/S0140-6736(06)68805-3. PMID 16753486.
- 1 2 "Violence and injuries to/against women". WHO. Retrieved 1 April 2013.
- 1 2 Ezzati, M; Lopez, A; Rodgers, A; Murray, C (2004). "Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors". Geneva: World Health Organization.
- 1 2 3 Garcia-Moreno, C; Reis, C (2005). "Overview on women’s health in crises" (PDF). Health in emergencies (Geneva: World Health Organization) (20).
- ↑ Garcia-Moreno, C.; Jansen, H. A. M.; Ellsberg, M.; Heise, L.; Watts, C. H. (2006). "Prevalence of intimate partner violence: Findings from the WHO multi-country study on women's health and domestic violence". The Lancet 368 (9543): 1260–1269. doi:10.1016/S0140-6736(06)69523-8.
- ↑ Krug, E (2002). World report on violence and health (Report). Geneva: World Health Organization.
- ↑ Nussbaum, M. C. (2004). "Women's Education: A Global Challenge". Signs: Journal of Women in Culture and Society 29 (2): 325–355. doi:10.1086/378571.
- ↑ World Health Organization (2001). World Health Report 2001 (PDF) (Report). Geneva.
- 1 2 3 4 Sen, Gita; Östlin, Piroska (2007). Unequal, Unfair, Ineffective and Inefficient Gender Inequity in Health: Why it exists and how we can change it; Final Report to the WHO Commission on Social Determinants of Health (PDF) (Report). Women and Gender Equity Knowledge Network.
- ↑ Cook, R; Dickens, B; Fathalla, M (2003). Reproductive health and human rights - Integrating medicine, ethics and law. Oxford University Press.
- ↑ George, A (2007). "Human Resources for Health: a gender analysis". Women and Gender Equity Knowledge Network.
- ↑ Ogden, J; Esim, S; Grown, C (2006). "Expanding the care continuum for HIV/AIDS: bringing carers into focus". Health Policy Plan 21: 333–42. doi:10.1093/heapol/czl025.
- ↑ World Health Organization (2006). World Health Report 2006 (PDF) (Report). Geneva.
- ↑ Wamala, S; Lynch, J (2002). Gender and socioeconomic inequalities in health. Lund, Studentlitteratur.
- ↑ World Health Organization (2008). The global burden of disease: 2004 update (PDF) (Report). Geneva.
- ↑ Campbell, J. C. (2002). "Health consequences of intimate partner violence". The Lancet 359 (9314): 1331–1336. doi:10.1016/S0140-6736(02)08336-8.
- ↑ Plichta, S. B.; Falik, M. (2001). "Prevalence of violence and its implications for women's health". Women's Health Issues 11 (3): 244–258. doi:10.1016/S1049-3867(01)00085-8.
- ↑ Farmer, Paul (2005). Pathologies of Power: Health, Human Rights, and the New War On the Poor. California: University of California Press.
- ↑ Seager, Roni (2009). The Penguin Atlas of Women in the World, 4th Edition. New York, New York: The Penguin Group.
- ↑ World Health Organization (2009). World health statistics 2009 (Report). Geneva: World Health Organization, 2009.
- ↑ United Nations (1996). Report of the Fourth World Conference on Women, Beijing 4–15 September 1995 (PDF) (Report). New York: United Nations. Retrieved 9 Apr 2013.
- ↑ World Health Organization (2008). The World Health Report 2008, Primary Health Care: Now more than ever (PDF) (Report). Geneva: World Health Organization. Retrieved 9 Apr 2013.
- 1 2 United Nations (2002). Gender Mainstreaming: An Overview (PDF) (Report). New York: United Nations. Retrieved 4 Apr 2013.
- ↑ Ravindran, T.K.S.; Kelkar-Khambete, A. (1 April 2008). "Gender mainstreaming in health: looking back, looking forward". Global Public Health 3 (sup1): 121–142. doi:10.1080/17441690801900761.
- 1 2 Ravindran, TKS; Kelkar-Khambete, A (2007). Women’s health policies and programmes and gender mainstreaming in health policies, programmes and within the health sector institutions. Background paper prepared for the Women and Gender Equity Knowledge Network of the WHO Commission on Social Determinants of Health, 2007 (PDF) (Report). Retrieved 9 April 2013.
- ↑ Ostlin, P; Diderichsen, F (2003). "Equity-oriented national strategy for public health in Sweden: A case study" (PDF). European Centre for Health Policy. Retrieved 9 April 2013.
- ↑ Linell, A.; Richardson, M. X.; Wamala, S. (22 January 2013). "The Swedish National Public Health Policy Report 2010". Scandinavian Journal of Public Health 41 (10 Suppl): 3–56. doi:10.1177/1403494812466989.
- ↑ Agren, G (2003). Sweden’s new public health policy: National public health objectives for Sweden (Report). Stockholm: Swedish National Institute of Public Health.
- ↑ Division for Advancement of Women, United Nations (2005). Enhancing Participation of Women in Development through an Enabling Environment for Achieving Gender Equality and the Advancement of Women, Expert Group Meeting, Bangkok, Thailand, 8 - 11 November 2005 (Report). Retrieved 9 Apr 2013.
- ↑ National Alliance for Caregiving in collaboration with AARP (2009). Caregiving in the U.S. 2009 (PDF) (Report). Retrieved 9 Apr 2013.
- ↑ Wallerstein, N (2006). What is the evidence on effectiveness of empowerment to improve health? Health Evidence Network Report (PDF) (Report). Copenhagen: Europe, World Health Organisation. Retrieved 9 Apr 2013.
- ↑ Manandhar, Dharma S; Osrin, David; Shrestha, Bhim Prasad; Mesko, Natasha; Morrison, Joanna; Tumbahangphe, Kirti Man; Tamang, Suresh; Thapa, Sushma; Shrestha, Dej; Thapa, Bidur; Shrestha, Jyoti Raj; Wade, Angie; Borghi, Josephine; Standing, Hilary; Manandhar, Madan; de L Costello, Anthony M (1 September 2004). "Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster-randomised controlled trial". The Lancet 364 (9438): 970–979. doi:10.1016/S0140-6736(04)17021-9.
- ↑ Pathmanathan, Indra; Liljestrand, Jerker; Martins first3=Jo. M.; Rajapaksa, Lalini C.; Lissner, Craig; de Silva, Amala; Selvaraju, Swarna; Singh first8=PrabhaJoginder (2003). "Investing in maternal health : learning from Malaysia and Sri Lanka". The World Bank, Human Development Network. Health, Nutrition, and Population Series.