Gastroesophageal reflux disease
| Gastroesophageal reflux disease | |
|---|---|
 X-ray showing radiocontrast agent injected into the stomach entering the esophagus due to severe reflux | |
| Classification and external resources | |
| Pronunciation | /gæstroʊɪˌsɑfəˈdʒiəl/ /ˈriflʌks/[1][2][3] |
| Specialty | Gastroenterology |
| ICD-10 | K21 |
| ICD-9-CM | 530.81 |
| OMIM | 109350 |
| DiseasesDB | 23596 |
| MedlinePlus | 000265 |
| eMedicine | med/857 ped/1177 radio/300 |
| MeSH | D005764 |
Gastroesophageal reflux disease (GERD), gastro-oesophageal reflux disease (GORD), gastric reflux disease, acid reflux disease, or reflux (in babies and young children) is a chronic condition of mucosal damage caused by stomach acid coming up from the stomach into the esophagus[4] (chronic reflux). Occasional reflux causes heartburn, but chronic reflux leads to reflux esophagitis, GERD, and sometimes Barrett esophagus.
GERD is usually caused by changes in the junction between the stomach and the esophagus, including abnormal relaxation of the lower esophageal sphincter, which normally holds the top of the stomach closed, impaired expulsion of gastric reflux from the esophagus, or a hiatal hernia. These changes may be permanent or temporary.
Treatment is typically via lifestyle changes and medications such as proton pump inhibitors, H2 receptor blockers or antacids with or without alginic acid.[5] Surgery may be an option in those who do not improve. In the Western world between 10 and 20% of the population is affected.[5]
Signs and symptoms
Adults
The most-common symptoms of GERD in adults are heartburn[6] and regurgitation. Less-common symptoms include pain with swallowing/sore throat, increased salivation (also known as water brash), nausea,[7] chest pain, and coughing.
GERD sometimes causes injury of the esophagus. These injuries may include one or more of the following:
- Reflux esophagitis – necrosis of esophageal epithelium causing ulcers near the junction of the stomach and esophagus
- Esophageal strictures – the persistent narrowing of the esophagus caused by reflux-induced inflammation
- Barrett's esophagus – intestinal metaplasia (changes of the epithelial cells from squamous to intestinal columnar epithelium) of the distal esophagus[8]
- Esophageal adenocarcinoma – a form of cancer[7]
Some people have proposed that symptoms such as sinusitis, recurrent ear infections, and idiopathic pulmonary fibrosis are due to GERD; however, a causative role has not been established.[7]
Children
GERD may be difficult to detect in infants and children, since they cannot describe what they are feeling and indicators must be observed. Symptoms may vary from typical adult symptoms. GERD in children may cause repeated vomiting, effortless spitting up, coughing, and other respiratory problems, such as wheezing. Inconsolable crying, refusing food, crying for food and then pulling off the bottle or breast only to cry for it again, failure to gain adequate weight, bad breath, and burping are also common. Children may have one symptom or many; no single symptom is universal in all children with GERD.
Of the estimated 4 million babies born in the US each year, up to 35% of them may have difficulties with reflux in the first few months of their lives, known as 'spitting up'.[9] One theory for this is the "fourth trimester theory" which notes most animals are born with significant mobility, but humans are relatively helpless at birth, and suggests there may have once been a fourth trimester, but children began to be born earlier, evolutionarily, to accommodate the development of larger heads and brains and allow them to pass through the birth canal and this leaves them with partially undeveloped digestive systems.
Most children will outgrow their reflux by their first birthday. However, a small but significant number of them will not outgrow the condition. This is particularly true when a family history of GERD is present.
Barrett's esophagus
GERD may lead to Barrett's esophagus, a type of intestinal metaplasia,[8] which is in turn a precursor condition for esophageal cancer. The risk of progression from Barrett's to dysplasia is uncertain, but is estimated at about 20% of cases.[10] Due to the risk of chronic heartburn progressing to Barrett's, EGD every five years is recommended for people with chronic heartburn, or who take drugs for chronic GERD.[11]
Causes
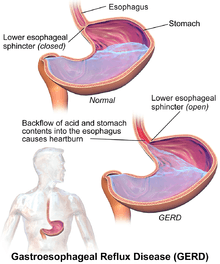
GERD is caused by a failure of the lower esophageal sphincter. In healthy patients, the "Angle of His"—the angle at which the esophagus enters the stomach—creates a valve that prevents duodenal bile, enzymes, and stomach acid from traveling back into the esophagus where they can cause burning and inflammation of sensitive esophageal tissue.
Factors that can contribute to GERD:
- Hiatal hernia, which increases the likelihood of GERD due to mechanical and motility factors.[12][13]
- Obesity: increasing body mass index is associated with more severe GERD.[14] In a large series of 2,000 patients with symptomatic reflux disease, it has been shown that 13% of changes in esophageal acid exposure is attributable to changes in body mass index.[15]
- Zollinger-Ellison syndrome, which can be present with increased gastric acidity due to gastrin production.
- A high blood calcium level, which can increase gastrin production, leading to increased acidity.
- Scleroderma and systemic sclerosis, which can feature esophageal dysmotility.
- The use of medicines such as prednisolone.
- Visceroptosis or Glénard syndrome, in which the stomach has sunk in the abdomen upsetting the motility and acid secretion of the stomach.
GERD has been linked to a variety of respiratory and laryngeal complaints such as laryngitis, chronic cough, pulmonary fibrosis, earache, and asthma, even when not clinically apparent. These atypical manifestations of GERD are commonly referred to as laryngopharyngeal reflux (LPR) or as extraesophageal reflux disease (EERD).
Factors that have been linked with GERD, but not conclusively:
- Obstructive sleep apnea[16][17]
- Gallstones, which can impede the flow of bile into the duodenum, which can affect the ability to neutralize gastric acid
In 1999, a review of existing studies found that, on average, 40% of GERD patients also had H. pylori infection.[18] The eradication of H. pylori can lead to an increase in acid secretion,[19] leading to the question of whether H. pylori-infected GERD patients are any different than non-infected GERD patients. A double-blind study, reported in 2004, found no clinically significant difference between these two types of patients with regard to the subjective or objective measures of disease severity.[20]
Diagnosis

The diagnosis of GERD is usually made when typical symptoms are present.[21] Reflux can be present in people without symptoms and the diagnosis requires both symptoms or complications and reflux of stomach content.[22]
Other investigations may include esophagogastroduodenoscopy (EGD). Barium swallow X-rays should not be used for diagnosis.[21] Esophageal manometry is not recommended for use in diagnosis being recommended only prior to surgery.[21] Ambulatory esophageal pH monitoring may be useful in those who do not improve after PPIs and is not needed in those in whom Barrett's esophagus is seen.[21] Investigations for H. pylori is not usually needed.[21]
The current gold standard for diagnosis of GERD is esophageal pH monitoring. It is the most objective test to diagnose the reflux disease and allows monitoring GERD patients in their response to medical or surgical treatment. One practice for diagnosis of GERD is a short-term treatment with proton-pump inhibitors, with improvement in symptoms suggesting a positive diagnosis. Short-term treatment with proton-pump inhibitors may help predict abnormal 24-hr pH monitoring results among patients with symptoms suggestive of GERD.[23]
Endoscopy
Endoscopy, the looking down into the stomach with a fibre-optic scope, is not routinely needed if the case is typical and responds to treatment.[21] It is recommended when people either do not respond well to treatment or have alarm symptoms, including dysphagia, anemia, blood in the stool (detected chemically), wheezing, weight loss, or voice changes.[21] Some physicians advocate either once-in-a-lifetime or 5- to 10-yearly endoscopy for people with longstanding GERD, to evaluate the possible presence of dysplasia or Barrett's esophagus.[24]
Biopsies performed during gastroscopy may show:
- Edema and basal hyperplasia (nonspecific inflammatory changes)
- Lymphocytic inflammation (nonspecific)
- Neutrophilic inflammation (usually due to reflux or Helicobacter gastritis)
- Eosinophilic inflammation (usually due to reflux): The presence of intraepithelial eosinophils may suggest a diagnosis of eosinophilic esophagitis (EE) if eosinophils are present in high enough numbers. Less than 20 eosinophils per high-power microscopic field in the distal esophagus, in the presence of other histologic features of GERD, is more consistent with GERD than EE.[25]
- Goblet cell intestinal metaplasia or Barrett's esophagus
- Elongation of the papillae
- Thinning of the squamous cell layer
- Dysplasia
- Carcinoma
Reflux changes may not be erosive in nature, leading to "nonerosive reflux disease".
Differential diagnosis
Other causes of chest pain such as heart disease should be ruled out before making the diagnosis.[21] Another kind of acid reflux, which causes respiratory and laryngeal signs and symptoms, is called laryngopharyngeal reflux (LPR) or "extraesophageal reflux disease" (EERD). Unlike GERD, LPR rarely produces heartburn, and is sometimes called silent reflux.
Treatment
The treatments for GERD include lifestyle modifications, medications, and possibly surgery. Initial treatment is frequently with a proton-pump inhibitor such as omeprazole.[21]
Lifestyle
Certain foods and lifestyle are considered to promote gastroesophageal reflux, but most dietary interventions have little supporting evidence.[26] Avoidance of specific foods and of eating before lying down should be recommended only to those in which they are associated with the symptoms.[22] Foods that have been implicated include coffee, alcohol, chocolate, fatty foods, acidic foods, and spicy foods.[22] Weight loss and elevating the head of the bed are generally useful.[27] Moderate exercise improves symptoms; however in those with GERD vigorous exercise may worsen them.[26] Stopping smoking and not drinking alcohol do not appear to result in significant improvement in symptoms.[27]
Medications
The primary medications used for GERD are proton-pump inhibitors, H2 receptor blockers and antacids with or without alginic acid.[5]
Proton-pump inhibitors (PPIs), such as omeprazole, are the most effective, followed by H2 receptor blockers, such as ranitidine.[22] If a once daily PPI is only partially effective they may be used twice a day.[22] They should be taken one half to one hour before a meal.[21] There is no significant difference between agents in this class.[21] When these medications are used long term, the lowest effective dose should be taken.[22] They may also be taken only when symptoms occur in those with frequent problems.[21] H2 receptor blockers lead to roughly a 40% improvement.[28]
The evidence for antacids is weaker with a benefit of about 10% (NNT=13) while a combination of an antacid and alginic acid (such as Gaviscon) may improve symptoms 60% (NNT=4).[28] Metoclopramide (a prokinetic) is not recommended either alone or in combination with other treatments due to concerns around adverse effects.[5][22] The benefit of the prokinetic mosapride is modest.[5]
Sucralfate has a similar effectiveness to H2 receptor blockers; however, sucralfate needs to be taken multiple times a day, thus limiting its use.[5] Baclofen, an agonist of the GABAB receptor, while effective, has similar issues of needing frequent dosing in addition to greater adverse effects compared to other medications.[5]
Surgery
The standard surgical treatment for severe GERD is the Nissen fundoplication. In this procedure, the upper part of the stomach is wrapped around the lower esophageal sphincter to strengthen the sphincter and prevent acid reflux and to repair a hiatal hernia.[29] It is recommended only for those who do not improve with PPIs.[21] Benefits are equal to medical treatment in those with chronic symptoms.[21] In addition, in the short and medium term, laparoscopic fundoplication improves quality of life compared to medical management.[30] When comparing different fundoplication techniques, partial posterior fundoplication surgery is more effective than partial anterior fundoplication surgery.[31]
In 2012 the FDA approved a device called the LINX, which consists of a series of metal beads with magnetic cores that are placed surgically around the lower esophageal sphincter, for those with severe symptoms that do not respond to other treatments. Improvement of GERD symptoms are similar to those of the Nissen fundoplication, although there is no data regarding long-term effects. Compared to Nissen fundoplication procedures, the procedure has shown a reduction in complications such as gas bloat syndrome that commonly occur.[32] Adverse responses include difficulty swallowing, chest pain, vomiting, and nausea. Contraindications that would advise against use of the device are patients who are or may be allergic to titanium, stainless steel, nickel, or ferrous iron materials. A warning advises that the device should not be used by patients who could be exposed to, or undergo, magnetic resonance imaging (MRI) because of serious injury to the patient and damage to the device.[33]
Pregnancy
In pregnancy, dietary modifications and lifestyle changes may be attempted, but often have little effect. Calcium-based antacids are recommended if these changes are not effective. Aluminum- and magnesium-based antacids are also safe, as is ranitidine[34] and PPIs.[21]
Infants
Infants may see relief with changes in feeding techniques, such as smaller, more frequent feedings, changes in position during feedings, or more frequent burping during feedings.[35] They may also be treated with medicines such as ranitidine or proton pump inhibitors.[36] Proton pump inhibitors however have not been found to be effective in this population and there is a lack of evidence for safety.[37]
Overtreatment
The use of acid suppression therapy is a common response to GERD symptoms and many patients get more of this kind of treatment than their individual case merits.[38] The overuse of this treatment is a problem because of the side effects and costs which the patient will have from undergoing unnecessary therapy, and patients should not take more treatment than they need.[38]
In some cases, a person with GERD symptoms can manage them by taking over-the-counter drugs and making lifestyle changes.[39] This is often safer and less expensive than taking prescription drugs.[39] Some guidelines recommend trying to treat symptoms with an H2 antagonist before using a proton-pump inhibitor because of cost and safety concerns.[39]
Epidemiology
In Western populations GERD affects approximately 10% to 20% of the population and 0.4% newly develop the condition.[5] For instance, an estimated 3.4 million to 6.8 million Canadians are GERD sufferers. The prevalence rate of GERD in developed nations is also tightly linked with age, with adults aged 60 to 70 being the most commonly affected.[40] In the United States 20% of people have symptoms in a given week and 7% every day.[5] No data support sex predominance with regard to GERD.
History
An obsolete treatment is vagotomy ("highly selective vagotomy"), the surgical removal of vagus nerve branches that innervate the stomach lining. This treatment has been largely replaced by medication.
Research
A number of endoscopic devices have been tested to treat chronic heartburn.
- Endocinch, puts stitches in the lower esophogeal sphincter (LES) to create small pleats to help strengthen the muscle. However, long-term results were disappointing, and the device is no longer sold by Bard.[41]
- Stretta procedure, uses electrodes to apply radio-frequency energy to the LES. A 2015 systematic review and meta-analysis in response to the systematic review (no meta-analysis) conducted by SAGES did not support the claims that Stretta was an effective treatment for GERD.[42] A 2012 systematic review found that it improves GERD symptoms.[43]
- NDO Surgical Plicator creates a plication, or fold, of tissue near the gastroesophageal junction, and fixates the plication with a suture-based implant. The company ceased operations in mid-2008, and the device is no longer on the market.
- Transoral incisionless fundoplication, which uses a device called Esophyx, may be effective.[44]
References
- ↑ http://www.collinsdictionary.com/dictionary/american/gastro-
- ↑ http://www.collinsdictionary.com/dictionary/american/esophagus
- ↑ http://www.oxfordlearnersdictionaries.com/definition/american_english/reflux
- ↑ DeVault KR, Castell DO (1999). "Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. The Practice Parameters Committee of the American College of Gastroenterology". Am J Gastroenterol 94 (6): 1434–42. doi:10.1111/j.1572-0241.1999.1123_a.x. PMID 10364004.
- 1 2 3 4 5 6 7 8 9 Hershcovici T, Fass R (April 2011). "Pharmacological management of GERD: where does it stand now?". Trends in pharmacological sciences 32 (4): 258–64. doi:10.1016/j.tips.2011.02.007. PMID 21429600.
- ↑ Zajac P, Holbrook A, Super ME, Vogt M (March–April 2013). "An overview: Current clinical guidelines for the evaluation, diagnosis, treatment, and management of dyspepsia". Osteopathic Family Physician 5 (2): 79–85. doi:10.1016/j.osfp.2012.10.005.
- 1 2 3 Kahrilas PJ (2008). "Gastroesophageal Reflux Disease". The New England Journal of Medicine 359 (16): 1700–7. doi:10.1056/NEJMcp0804684. PMC 3058591. PMID 18923172.
- 1 2 Wang KK, Sampliner RE (March 2008). "Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett's esophagus" (PDF). Am J Gastroenterol 103 (3): 788–97. doi:10.1111/j.1572-0241.2008.01835.x. PMID 18341497.
- ↑ "Spitting Up in Babies". familydoctor.org.
- ↑ and Barrett's Esophagus. Retrieved on 2009-02-01.
- ↑ "Patient information: Barrett's esophagus (Beyond the Basics)". June 2009.
- ↑ Sontag SJ (1999). "Defining GERD". Yale J Biol Med 72 (2–3): 69–80. PMC 2579007. PMID 10780568.
- ↑ Piesman M, Hwang I, Maydonovitch C, Wong RK (2007). "Nocturnal reflux episodes following the administration of a standardized meal. Does timing matter?". Am J Gastroenterol 102 (10): 2128–34. doi:10.1111/j.1572-0241.2007.01348.x. PMID 17573791.
- ↑ Ayazi S; Crookes PF; Peyre CG; et al. (2007). "Objective documentation of the link between gastroesophageal reflux disease and obesity". Am J Gastroenterol 102 (S2): 138–9. doi:10.1111/j.1572-0241.2007.01491_1.x.
- ↑ Ayazi S, Hagen JA, Chan LS, DeMeester SR, Lin MW, Ayazi A, Leers JM, Oezcelik A, Banki F, Lipham JC, DeMeester TR, Crookes PF (August 2009). "Obesity and Gastroesophageal Reflux: Quantifying the Association Between Body Mass Index, Esophageal Acid Exposure, and Lower Esophageal Sphincter Status in a Large Series of Patients with Reflux Symptoms". J. Gastrointest. Surg. 13 (8): 1440–7. doi:10.1007/s11605-009-0930-7. PMC 2710497. PMID 19475461.
- ↑ Morse CA, Quan SF, Mays MZ, Green C, Stephen G, Fass R (2004). "Is there a relationship between obstructive sleep apnea and gastroesophageal reflux disease?". Clin. Gastroenterol. Hepatol. 2 (9): 761–8. doi:10.1016/S1542-3565(04)00347-7. PMID 15354276.
- ↑ Kasasbeh A, Kasasbeh E, Krishnaswamy G (2007). "Potential mechanisms connecting asthma, esophageal reflux, and obesity/sleep apnea complex—a hypothetical review". Sleep Med Rev 11 (1): 47–58. doi:10.1016/j.smrv.2006.05.001. PMID 17198758.
- ↑ O'Connor HJ (Feb 1999). "Helicobacter pylori and gastro-oesophageal reflux disease-clinical implications and management". Aliment Pharmacol Ther 13 (2): 117–27. doi:10.1046/j.1365-2036.1999.00460.x. PMID 10102940.
- ↑ El-Omar EM, Oien K, El-Nujumi A, Gillen D, Wirz A, Dahill S, Williams C, Ardill JE, McColl KE (1997). "Helicobacter pylori infection and chronic gastric acid hyposecretion". Gastroenterology 113 (1): 15–24. doi:10.1016/S0016-5085(97)70075-1. PMID 9207257.
- ↑ Fallone CA, Barkun AN, Mayrand S, Wakil G, Friedman G, Szilagyi A, Wheeler C, Ross D (2004). "There is no difference in the disease severity of gastro-oesophageal reflux disease between patients infected and not infected with Helicobacter pylori". Aliment Pharmacol Ther 20 (7): 761–8. doi:10.1111/j.1365-2036.2004.02171.x. PMID 15379836.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Katz PO, Gerson LB, Vela MF (March 2012). "Guidelines for the diagnosis and management of gastroesophageal reflux disease.". The American journal of gastroenterology 108 (3): 308–28. doi:10.1038/ajg.2012.444. PMID 23419381.
- 1 2 3 4 5 6 7 Kahrilas PJ, Shaheen NJ, Vaezi MF, Hiltz SW, Black E, Modlin IM, Johnson SP, Allen J, Brill JV (October 2008). "American Gastroenterological Association Medical Position Statement on the management of gastroesophageal reflux disease". Gastroenterology 135 (4): 1383–1391, 1391.e1–5. doi:10.1053/j.gastro.2008.08.045. PMID 18789939.
- ↑ Numans ME, Lau J, de Wit NJ, Bonis PA (April 2004). "Short-term treatment with proton-pump inhibitors as a test for gastroesophageal reflux disease: a meta-analysis of diagnostic test characteristics" (PDF). Annals of internal medicine 140 (7): 518–27. doi:10.7326/0003-4819-140-7-200404060-00011. PMID 15068979.
- ↑ Patient information: Barrett's esophagus
- ↑ Mills, S (ed.) 2009.Sternberg's Diagnostic Pathology. 5th Edition. ISBN 978-0-7817-7942-5
- 1 2 Festi D, Scaioli E, Baldi F, Vestito A, Pasqui F, Di Biase AR, Colecchia A (Apr 14, 2009). "Body weight, lifestyle, dietary habits and gastroesophageal reflux disease". World journal of gastroenterology : WJG 15 (14): 1690–701. doi:10.3748/wjg.15.1690. PMC 2668774. PMID 19360912.
- 1 2 Kaltenbach T, Crockett S, Gerson LB (2006). "Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach". Arch. Intern. Med. 166 (9): 965–71. doi:10.1001/archinte.166.9.965. PMID 16682569.
- 1 2 Tran T, Lowry AM, El-Serag HB (2007). "Meta-analysis: the efficacy of over-the-counter gastro-oesophageal reflux disease drugs". Aliment Pharmacol Ther 25 (2): 143–53. doi:10.1111/j.1365-2036.2006.03135.x. PMID 17229239.
- ↑ Abbas AE, Deschamps C, Cassivi SD, Allen MS, Nichols FC, Miller DL, Pairolero PC (2004). "The role of laparoscopic fundoplication in Barrett's esophagus". Annals of Thoracic Surgery 77 (2): 393–6. doi:10.1016/S0003-4975(03)01352-3. PMID 14759403.
- ↑ Wileman SM, McCann S, Grant AM, Krukowski ZH, Bruce J (2010). Wileman, Samantha M, ed. "Medical versus surgical management for gastro-oesophageal reflux disease (GORD) in adults". Cochrane database of systematic reviews (Online) 3 (3): CD003243. doi:10.1002/14651858.CD003243.pub2. PMID 20238321.
- ↑ Kurian AA, Bhayani N, Sharata A, Reavis K, Dunst CM, Swanström LL (January 2013). "Partial anterior vs partial posterior fundoplication following transabdominal esophagocardiomyotomy for achalasia of the esophagus: meta-regression of objective postoperative gastroesophageal reflux and dysphagia". JAMA Surg 148 (1): 85–90. doi:10.1001/jamasurgery.2013.409. PMID 23324843.
- ↑ Badillo, Raul (2014). "Diagnosis and treatment of gastroesophageal reflux disease". World Journal of Gastrointestinal Pharmacology and Therapeutics 5 (3): 105. doi:10.4292/wjgpt.v5.i3.105.
- ↑ Medical Device Approvals: LINX™ Reflux Management System - P100049, U.S. Food and Drug Administration, U.S. Department of Health and Human Services, Update of 01/17/2014
- ↑ Mahadevan U, Kane S (July 2006). "American gastroenterological association institute medical position statement on the use of gastrointestinal medications in pregnancy". Gastroenterology 131 (1): 278–82. doi:10.1053/j.gastro.2006.04.048. PMID 16831610.
- ↑ Infant acid reflux. MayoClinic.com (2013-03-28). Retrieved on 2013-09-27.
- ↑ Tighe MP, Afzal NA, Bevan A, Beattie RM (2009). "Current pharmacological management of gastro-esophageal reflux in children: an evidence-based systematic review". Paediatr Drugs 11 (3): 185–202. doi:10.2165/00148581-200911030-00004. PMID 19445547.
- ↑ van der Pol RJ, Smits MJ, van Wijk MP, Omari TI, Tabbers MM, Benninga MA (May 2011). "Efficacy of proton-pump inhibitors in children with gastroesophageal reflux disease: a systematic review". Pediatrics 127 (5): 925–35. doi:10.1542/peds.2010-2719. PMID 21464183.
- 1 2 Here is a plain English explanation, followed by specific studies.
- Consumer Reports; Drug Effectiveness Review Project (May 2010), "Drugs to Treat Heartburn and Stomach Acid Reflux: The Proton Pump Inhibitors - Comparing Effectiveness, Safety, and Price" (PDF), Best Buy Drugs (Consumer Reports), p. 6, retrieved 27 March 2013
- Gupta R, Marshall J, Munoz JC, Kottoor R, Jamal MM, Vega KJ (2013). "Decreased acid suppression therapy overuse after education and medication reconciliation". International Journal of Clinical Practice 67 (1): 60–65. doi:10.1111/ijcp.12046. PMID 23241049.
- Nardino RJ, Vender RJ, Herbert PN (2000). "Overuse of acid-suppressive therapy in hospitalized patients1". The American Journal of Gastroenterology 95 (11): 3118–3122. doi:10.1111/j.1572-0241.2000.03259.x. PMID 11095327.
- Heidelbaugh JJ, Kim AH, Chang R, Walker PC (2012). "Overutilization of proton-pump inhibitors: What the clinician needs to know". Therapeutic Advances in Gastroenterology 5 (4): 219–232. doi:10.1177/1756283X12437358. PMC 3388523. PMID 22778788.
- Forgacs I, Loganayagam A (2008). "Overprescribing proton pump inhibitors". BMJ 336 (7634): 2–3. doi:10.1136/bmj.39406.449456.BE. PMC 2174763. PMID 18174564.
- McKay AB, Wall D (2008). "Overprescribing PPIs: An old problem". BMJ 336 (7636): 109. doi:10.1136/bmj.39458.462338.3A. PMC 2206261. PMID 18202040.
- 1 2 3
- Consumer Reports; Drug Effectiveness Review Project (May 2010), "Drugs to Treat Heartburn and Stomach Acid Reflux: The Proton Pump Inhibitors - Comparing Effectiveness, Safety, and Price" (PDF), Best Buy Drugs (Consumer Reports), p. 6, retrieved 27 March 2013
- Forgacs I, Loganayagam A (2008). "Overprescribing proton pump inhibitors". BMJ 336 (7634): 2–3. doi:10.1136/bmj.39406.449456.BE. PMC 2174763. PMID 18174564.
- Heidelbaugh JJ, Kim AH, Chang R, Walker PC (2012). "Overutilization of proton-pump inhibitors: What the clinician needs to know". Therapeutic Advances in Gastroenterology 5 (4): 219–232. doi:10.1177/1756283X12437358. PMC 3388523. PMID 22778788.
- ↑ Fedorak RN, Veldhuyzen van Zanten S, Bridges R (July 2010). "Canadian Digestive Health Foundation Public Impact Series: Gastroesophageal reflux disease in Canada: Incidence, prevalence, and direct and indirect economic impact". Canadian Journal of Gastroenterology 24 (7): 431–4. PMC 2918483. PMID 20652158. Lay summary.
- ↑ Jafri SM, Arora G, Triadafilopoulos G (July 2009). "What is left of the endoscopic antireflux devices?". Current Opinion in Gastroenterology 25 (4): 352–7. doi:10.1097/MOG.0b013e32832ad8b4. PMID 19342950.
- ↑ Lipka, S; Kumar, A; Richter, JE (June 2015). "No evidence for efficacy of radiofrequency ablation for treatment of gastroesophageal reflux disease: a systematic review and meta-analysis.". Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association 13 (6): 1058–67.e1. doi:10.1016/j.cgh.2014.10.013. PMID 25459556.
- ↑ Perry, KA; Banerjee, A; Melvin, WS (August 2012). "Radiofrequency energy delivery to the lower esophageal sphincter reduces esophageal acid exposure and improves GERD symptoms: a systematic review and meta-analysis.". Surgical laparoscopy, endoscopy & percutaneous techniques 22 (4): 283–8. doi:10.1097/sle.0b013e3182582e92. PMID 22874675.
- ↑ Testoni PA, Vailati C (August 2012). "Transoral incisionless fundoplication with EsophyX® for treatment of gastro-oesphageal reflux disease". Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver 44 (8): 631–5. doi:10.1016/j.dld.2012.03.019. PMID 22622203.
Further reading
- Kahrilas PJ, Shaheen NJ, Vaezi MF, Hiltz SW, Black E, Modlin IM, Johnson SP, Allen J, Brill JV (October 2008). "American Gastroenterological Association Medical Position Statement on the management of gastroesophageal reflux disease". Gastroenterology 135 (4): 1383–91, 1391.e1–5. doi:10.1053/j.gastro.2008.08.045. PMID 18789939. Lay summary.
- Lichtenstein DR, Cash BD, Davila R, Baron TH, Adler DG, Anderson MA, Dominitz JA, Gan SI, Harrison ME, Ikenberry SO, Qureshi WA, Rajan E, Shen B, Zuckerman MJ, Fanelli RD, VanGuilder T (August 2007). "Role of endoscopy in the management of GERD". Gastrointestinal Endoscopy 66 (2): 219–24. doi:10.1016/j.gie.2007.05.027. PMID 17643692. Lay summary.
- Hirano I, Richter JE (March 2007). "ACG practice guidelines: esophageal reflux testing" (PDF). Am J Gastroenterol 102 (3): 668–85. doi:10.1111/j.1572-0241.2006.00936.x. PMID 17335450.