Fanconi anemia
| Fanconi anemia | |
|---|---|
| Classification and external resources | |
| Specialty | hematology |
| ICD-10 | D61.0 |
| ICD-9-CM | 284.0 |
| OMIM | 227650 |
| DiseasesDB | 4745 |
| MedlinePlus | 000334 |
| eMedicine | ped/3022 |
| MeSH | D005199 |
| GeneReviews | |
| Orphanet | 84 |
Fanconi anemia (FA) is a very rare genetic disease with an incidence of 1 per 350,000 births, with a higher frequency in Ashkenazi Jews and Afrikaners in South Africa.[1]
FA is the result of a genetic defect in a cluster of proteins responsible for DNA repair. As a result, the majority of FA patients develop cancer, most often acute myelogenous leukemia, and 90% develop bone marrow failure (the inability to produce blood cells) by age 40. About 60–75% of FA patients have congenital defects, commonly short stature, abnormalities of the skin, arms, head, eyes, kidneys, and ears, and developmental disabilities. Around 75% of FA patients have some form of endocrine problem, with varying degrees of severity. Median age of death was 30 years in 2000.[2]
Treatment with androgens and hematopoietic (blood cell) growth factors can help bone marrow failure temporarily, but the long-term treatment is bone marrow transplant if a donor is available.[2]
Because of the genetic defect in DNA repair, cells from people with FA are sensitive to drugs that treat cancer by DNA crosslinking, such as mitomycin C.
The disease is named after the Swiss pediatrician who originally described this disorder, Guido Fanconi.[3][4] It should not be confused with Fanconi syndrome, a kidney disorder also named after Fanconi.
Signs and symptoms
During childhood, short stature and skin pigmentation, including café au lait spots, may become apparent. The first sign of a hematologic problem is usually petechiae and bruises, with later onset of pale appearance, feeling tired, and infections. Because macrocytosis usually precedes a low platelet count, patients with typical congenital anomalies associated with FA should be evaluated for an elevated red blood cell mean corpuscular volume.[5]
Genetics
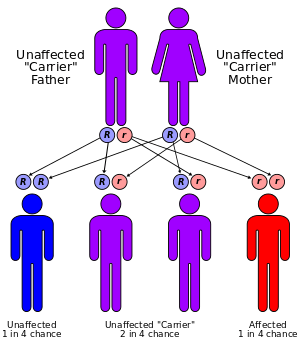
FA is primarily an autosomal recessive genetic disorder. This means that two mutated alleles (one from each parent) are required to cause the disease. There is a 25% risk that each subsequent child will have FA. About 2% of FA cases are X-linked recessive, which means that if the mother carries one mutated Fanconi anemia allele on one X chromosome, there is a 50% chance that male offspring will present with Fanconi anemia.
Scientists have identified 17 FA or FA-like genes: FANCA, FANCB, FANCC, FANCD1 (BRCA2), FANCD2, FANCE, FANCF, FANCG, FANCI, FANCJ (BRIP1), FANCL, FANCM, FANCN (PALB2), FANCP (SLX4), FANCS (BRCA1), RAD51C, and XPF. FANCB is the one exception to FA being autosomal recessive, as this gene is on the X chromosome.
The carrier frequency in the Ashkenazi Jewish population is about 1/90.[6] Genetic counseling and genetic testing is recommended for families that may be carriers of Fanconi anemia.
Because of the failure of hematologic components to develop — white blood cells, red blood cells and platelets — the body's capabilities to fight infection, deliver oxygen, and form clots are all diminished.
Pathogenesis
Clinically, hematological abnormalities are the most serious symptoms in FA. By the age of 40, 98% of FA patients will have developed some type of hematological abnormality. However, there are a few cases in which older patients have died without ever developing them. Symptoms appear progressively, and often lead to complete bone marrow failure. While at birth, blood count is usually normal, macrocytosis/megaloblastic anemia, defined as unusually large red blood cells, is the first detected abnormality, often within the first decade of life (median age of onset is 7 years). Within the next 10 years, over 50% of patients presenting haematological abnormalities will have developed pancytopenia, defined as abnormalities in two or more blood cell lineages. This is in contrast to Diamond–Blackfan anemia, which affects only erythrocytes, and Shwachman–Diamond syndrome, which primarily causes neutropenia.Most commonly, a low platelet count (thrombocytopenia) precedes a low neutrophil count (neutropenia), with both appearing with relative equal frequencies. The deficiencies cause increased risk of hemorrhage and recurrent infections, respectively.
As FA is now known to affect the DNA repair, and given the current knowledge about dynamic cell division in the bone marrow, it is not surprising to find patients are more likely to develop bone marrow failure, myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML).
Myelodysplastic syndromes
MDS, formerly known as preleukemia, are a group of bone marrow neoplastic diseases that share many of the morphologic features of AML, with some important differences. First, the percentage of undifferentiated progenitor cells, blast cells, is always less than 20%, and there is considerably more dysplasia, defined as cytoplasmic and nuclear morphologic changes in erythroid, granulocytic and megakaryocytic precursors, than what is usually seen in cases of AML. These changes reflect delayed apoptosis or a failure of programmed cell death. When left untreated, MDS can lead to AML in about 30% of cases. Due the nature of the FA pathology, MDS diagnosis cannot be made solely through cytogenetic analysis of the marrow. Indeed, it is only when morphologic analysis of marrow cells is performed, that a diagnosis of MDS can be ascertained. Upon examination, MDS-afflicted FA patients will show many clonal variations, appearing either prior or subsequent to the MDS. Furthermore, cells will show chromosomal aberrations, the most frequent being monosomy 7 and partial trisomies of chromosome 3q 15. Observation of monosomy 7 within the marrow is well correlated with an increased risk of developing AML and with a very poor prognosis, death generally ensuing within 2 years (unless prompt allogeneic hematopoietic progenitor cell transplant is an option).[7]
Acute myeloid leukemia
FA patients are at elevated risk for the development of acute myeloid leukemia (AML), defined as presence of 20% or more of myeloid blasts in the marrow or 5 to 20% myeloid blasts in the blood. All of the subtypes of AML can occur in FA with the exception of promyelocytic. However, myelomonocytic and acute monocytic are the most common subtypes observed. Many MDS patients will evolve into AML if they survive long enough. Furthermore, the risk of developing AML increases with the onset of bone marrow failure.
Although risk of developing either MDS or AML before the age of 20 is only 27%, this risk increases to 43% by the age of 30 and 52% by the age of 40. Historically, even with a marrow transplant, about 1/4 of FA patients diagnosed with MDS/ALS have died from MDS/ALS-related causes within 2 years (Butturini, A et al. 1994. Blood. 84:1650-4), although more recent published evidence suggests that earlier allogeneic hematopoietic progenitor cell transplantation in children with Fanconi anemia is leading to better outcomes over time[8]
Bone marrow failure
The last major haematological complication associated with FA is bone marrow failure, defined as inadequate blood cell production. Several types of failure are observed in FA patients, and generally precede MDS and AML. Detection of decreasing blood count is generally the first sign used to assess necessity of treatment and possible transplant. While most FA patients are initially responsive to androgen therapy and haemopoietic growth factors, these have been shown to promote leukemia, especially in patients with clonal cytogenetic abnormalities, and have severe side effects, including hepatic adenomas and adenocarcinomas. The only treatment left would be bone marrow transplant; however, such an operation has a relatively low success rate in FA patients when the donor is unrelated (30% 5-year survival). It is therefore imperative to transplant from an HLA-identical sibling. Furthermore, due to the increased susceptibility of FA patients to chromosomal damage, pretransplant conditioning cannot include high doses of radiations or immunosuppressants, and thus increase chances of patients developing graft-versus-host disease. If all precautions are taken, and the marrow transplant is performed within the first decade of life, 2-year probability of survival can be as high as 89%. However, if the transplant is performed at ages older than 10, 2-year survival rates drop to 54%.
A recent report by Zhang et al. investigates the mechanism of bone marrow failure in FANCC-/- cells.[9] They hypothesize and successfully demonstrate that continuous cycles of hypoxia-reoxygenation, such as those seen by haemopoietic and progenitor cells as they migrate between hyperoxic blood and hypoxic marrow tissues, leads to premature cellular senescence and therefore inhibition of haemopoietic function. Senescence, together with apoptosis, may constitute a major mechanism of haemopoietic cell depletion occurred in bone marrow failure.
Molecular basis
There are 17 genes responsible for FA, one of them being the breast-cancer susceptibility gene BRCA2. They are involved in the recognition and repair of damaged DNA; genetic defects leave them unable to repair DNA. The FA core complex of 8 proteins is normally activated when DNA stops replicating because of damage. The core complex adds ubiquitin, a small protein that combines with BRCA2 in another cluster to repair DNA. At the end of the process, ubiquitin is removed.[2]
Recent studies have shown that eight of these proteins, FANCA, -B, -C, -E, -F, -G, -L and –M assemble to form a core protein complex in the nucleus. According to current models, the complex moves from the cytoplasm into the nucleus following nuclear localization signals on FANCA and FANCE. Assembly is activated by replicative stress, particularly DNA damage caused by cross-linking agents (such as mitomycin C or cisplatin) or reactive oxygen species (ROS) that is detected by the FANCM protein.[10]
Following assembly, the protein core complex activates FANCL protein which acts as an E3 ubiquitin-ligase and monoubiquitinates FANCD2.[11][12][13][14]
Monoubiquitinated FANCD2, also known as FANCD2-L, then goes on to interact with a BRCA1/BRCA2 complex. Details are not known, but similar complexes are involved in genome surveillance and associated with a variety of proteins implicated in DNA repair and chromosomal stability.[15][16] With a crippling mutation in any FA protein in the complex, DNA repair is much less effective, as shown by its response to damage caused by cross-linking agents such as cisplatin, diepoxybutane[17] and Mitomycin C. Bone marrow is particularly sensitive to this defect.
In another pathway responding to ionizing radiation, FANCD2 is thought to be phosphorylated by protein complex ATM/ATR activated by double-strand DNA breaks, and takes part in S-phase checkpoint control. This pathway was proven by the presence of radioresistant DNA synthesis, the hallmark of a defect in the S phase checkpoint, in patients with FA-D1 or FA-D2. Such a defect readily leads to uncontrollable replication of cells and might also explain the increase frequency of AML in these patients.
Treatment
The first line of therapy is androgens and hematopoietic growth factors, but only 50-75% of patients respond. A more permanent cure is hematopoietic stem cell transplantation.[18] If no potential donors exist, a savior sibling can be conceived by preimplantation genetic diagnosis (PGD) to match the recipient's HLA type.[19][20]
Prognosis
Many patients eventually develop acute myelogenous leukemia (AML). Older patients are extremely likely to develop head and neck, esophageal, gastrointestinal, vulvar and anal cancers.[21] Patients who have had a successful bone marrow transplant and, thus, are cured of the blood problem associated with FA still must have regular examinations to watch for signs of cancer. Many patients do not reach adulthood.
The overarching medical challenge that Fanconi patients face is a failure of their bone marrow to produce blood cells. In addition, Fanconi patients normally are born with a variety of birth defects. A good number of Fanconi patients have kidney problems, trouble with their eyes, developmental retardation and other serious defects, such as microcephaly (small head). [22]
See also
- RecQ Family
- Absent radius
- BRCA2
- PALB2
References
- ↑ Fanconi's Anemia Orphanet Encyclopedia, Ethel Moustacchi, October 2003
- 1 2 3 Schwartz, Robert S.; d'Andrea, Alan D. (May 2010). "Susceptibility pathways in Fanconi's anemia and breast cancer". N. Engl. J. Med. 362 (20): 1909–1919. doi:10.1056/NEJMra0809889. PMC 3069698. PMID 20484397.
- ↑ synd/61 at Who Named It?
- ↑ Fanconi, G. "Familiäre, infantile perniciosähnliche Anämie (perniziöses Blutbild und Konstitution)". Jahrbuch für Kinderheilkunde.
- ↑ Fanconi Anemia~clinical at eMedicine
- ↑ Kutler DI, Auerbach AD (2004). "Fanconi anemia in Ashkenazi Jews". Fam. Cancer 3 (3–4): 241–248. doi:10.1007/s10689-004-9565-8. PMID 15516848.
- ↑ Mehta PA, et al. (2010). "Numerical chromosomal changes and risk of development of myelodysplastic syndrome-acute myeloid leukemia in patients with Fanconi anemia". Cancer Genetics 203 (2): 180-186. doi:10.1016/j.cancergencyto.2010.07.127.
- ↑ de Latour RP, et al. (2013). "Allogeneic hematopoietic stem cell transplantation in Fanconi anemia: the EBMT experience". Blood. published online before print, doi: 10.1182/blood-2013-01-479733.
- ↑ Zhang X, Li J, Sejas DP, Pang Q (2005). "Hypoxia-reoxygenation induces premature senescence in FA bone marrow hematopoietic cells". Blood 106 (1): 75–85. doi:10.1182/blood-2004-08-3033. PMID 15769896.
- ↑ Deans AJ, West SC (December 2009). "FANCM connects the genome instability disorders Bloom's Syndrome and Fanconi Anemia". Mol. Cell 36 (6): 943–53. doi:10.1016/j.molcel.2009.12.006. PMID 20064461.
- ↑ Vandenberg CJ; Gergely F; Ong CY; et al. (2003). "BRCA1-independent ubiquitination of FANCD2". Mol. Cell 12 (1): 247–254. doi:10.1016/S1097-2765(03)00281-8. PMID 12887909.
- ↑ Garcia-Higuera I; Taniguchi T; Ganesan S; et al. (2001). "Interaction of the Fanconi anemia proteins and BRCA1 in a common pathway". Mol. Cell 7 (2): 249–262. doi:10.1016/S1097-2765(01)00173-3. PMID 11239454.
- ↑ Wang Y, Cortez D, Yazdi P, Neff N, Elledge SJ, Qin J (2000). "BASC, a super complex of BRCA1-associated proteins involved in the recognition and repair of aberrant DNA structures". Genes Dev. 14 (8): 927–39. doi:10.1101/gad.14.8.927. PMC 316544. PMID 10783165.
- ↑ Cortez D, Wang Y, Qin J, Elledge SJ (1999). "Requirement of ATM-dependent phosphorylation of brca1 in the DNA damage response to double-strand breaks". Science 286 (5442): 1162–1166. doi:10.1126/science.286.5442.1162. PMID 10550055.
- ↑ Howlett NG; Taniguchi T; Olson S; et al. (2002). "Biallelic inactivation of BRCA2 in Fanconi anemia". Science 297 (5581): 606–609. doi:10.1126/science.1073834. PMID 12065746.
- ↑ Connor F; Bertwistle D; Mee PJ; et al. (1997). "Tumorigenesis and a DNA repair defect in mice with a truncating Brca2 mutation". Nat. Genet. 17 (4): 423–430. doi:10.1038/ng1297-423. PMID 9398843.
- ↑ Auerbach AD, Rogatko A, Schroeder-Kurth TM (1989). "International Fanconi Anemia Registry: relation of clinical symptoms to diepoxybutane sensitivity". Blood 73 (2): 391–6. doi:10.1007/978-3-642-74179-1_1. PMID 2917181.
- ↑ Fanconi Anemia~treatment at eMedicine
- ↑ Page 29 in Moore, Pete (2007). The Debate About Genetic Engineering (Ethical Debates). New York, NY: Rosen Central. ISBN 1-4042-3754-2.
- ↑ Verlinsky, Y; Rechitsky, S; Schoolcraft, W; Strom, C; Kuliev, A (2001). ", Preimplantation diagnosis for Fanconi anemia combined with HLA matching". JAMA 285 (24): 3130–3133. doi:10.1001/jama.285.24.3130. PMID 11427142.
- ↑ Institut Biologia Fonamental de Barcelona, "Constitutional chromosomal instability: a case with three primary and sequential cancers", USUJ 2009. Retrieved 2010-04-13
- ↑ http://icmmt.alere.com/kbase/nord/nord84.htm
External links
- Fanconi Anemia Research Fund
- GeneReviews/NCBI/NIH/UW entry on Fanconi Anemia
- OMIM entries on Fanconi Anemia
- Fanconi anemia at DMOZ
- Fanconi Hope Charitable Trust - based in the UK, with Eu and International Links
- Fanconi Anaemia FAmily Support - based in the UK
- Fanconi's Anaemia on patient.info
| ||||||||||||||||||||||||