Cannabinoid
Cannabinoids are a class of diverse chemical compounds that act on cannabinoid receptors in cells that repress neurotransmitter release in the brain. Ligands for these receptor proteins include the endocannabinoids (produced naturally in the body by humans and animals),[1] the phytocannabinoids (found in cannabis and some other plants), and synthetic cannabinoids (manufactured artificially). The most notable cannabinoid is the phytocannabinoid tetrahydrocannabinol (THC), the primary psychoactive compound of cannabis.[2][3] Cannabidiol (CBD) is another major constituent of the plant.[4] There are at least 85 different cannabinoids isolated from cannabis, exhibiting varied effects.[5]
Synthetic cannabinoids encompass a variety of distinct chemical classes: the classical cannabinoids structurally related to THC, the nonclassical cannabinoids (cannabimimetics) including the aminoalkylindoles, 1,5-diarylpyrazoles, quinolines, and arylsulfonamides, as well as eicosanoids related to the endocannabinoids.[2]
Cannabinoid receptors
Before the 1980s, it was often speculated that cannabinoids produced their physiological and behavioral effects via nonspecific interaction with cell membranes, instead of interacting with specific membrane-bound receptors. The discovery of the first cannabinoid receptors in the 1980s helped to resolve this debate.[6] These receptors are common in animals, and have been found in mammals, birds, fish, and reptiles. At present, there are two known types of cannabinoid receptors, termed CB1 and CB2,[1] with mounting evidence of more.[7] The human brain has more cannabinoid receptors than any other G protein-coupled receptor (GPCR) type.[8]
Cannabinoid receptor type 1
CB1 receptors are found primarily in the brain, more specifically in the basal ganglia and in the limbic system, including the hippocampus.[1] They are also found in the cerebellum and in both male and female reproductive systems. CB1 receptors are absent in the medulla oblongata, the part of the brain stem responsible for respiratory and cardiovascular functions.
Cannabinoid receptor type 2
CB2 receptors are predominantly found in the immune system, or immune-derived cells[9] with the greatest density in the spleen. While found only in the peripheral nervous system, a report does indicate that CB2 is expressed by a subpopulation of microglia in the human cerebellum.[10] CB2 receptors appear to be responsible for the anti-inflammatory and possibly other therapeutic effects of cannabis seen in animal models.[9]
Phytocannabinoids
| Type | Skeleton | Cyclization |
|---|---|---|
| Cannabigerol-type CBG |
 |
 |
| Cannabichromene-type CBC |
 |
 |
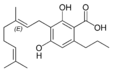
| Cannabidiol-type CBD |
 |
 |
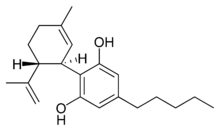
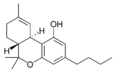
| Tetrahydrocannabinol- and Cannabinol-type THC, CBN |
 |
 |
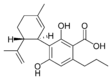
| Cannabielsoin-type CBE |
 |
 |
| iso- Tetrahydrocannabinol- type iso-THC |
 |
 |
| Cannabicyclol-type CBL |
 |
 |
| Cannabicitran-type CBT |
 |
 |
| Main classes of natural cannabinoids | ||

Cannabis-derived cannabinoids

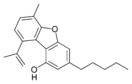
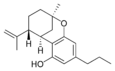
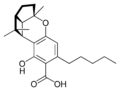
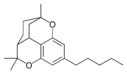
The classical cannabinoids are concentrated in a viscous resin produced in structures known as glandular trichomes. At least 104 different cannabinoids have been isolated from the Cannabis plant[11] To the right, the main classes of cannabinoids from Cannabis are shown. The best studied cannabinoids include tetrahydrocannabinol (THC), cannabidiol (CBD) and cannabinol (CBN).
Types
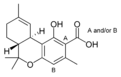
All classes derive from cannabigerol-type compounds and differ mainly in the way this precursor is cyclized.[12] The classical cannabinoids are derived from their respective 2-carboxylic acids (2-COOH) by decarboxylation (catalyzed by heat, light, or alkaline conditions).[13]
- CBG (Cannabigerol)
- CBC (Cannabichromene)
- CBL (Cannabicyclol)
- CBV (Cannabivarin)
- THCV (Tetrahydrocannabivarin)
- CBDV (Cannabidivarin)
- CBCV (Cannabichromevarin)
- CBGV (Cannabigerovarin)
- CBGM (Cannabigerol Monomethyl Ether)
Tetrahydrocannabinol
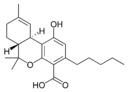
Tetrahydrocannabinol (THC) is the primary psychoactive component of the Cannabis plant. Delta-9-tetrahydrocannabinol (Δ9-THC, THC) and delta-8-tetrahydrocannabinol (Δ8-THC), mimic the action of anandamide, a neurotransmitter produced naturally in the body. These two cannabinoids produce the effects associated with cannabis by binding to the CB1 cannabinoid receptors in the brain.
Cannabidiol
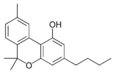
Cannabidiol (CBD) is non-psychotropic. Recent evidence shows that the compound counteracts cognitive impairment associated with the use of cannabis.[14] Cannabidiol has little affinity for CB1 and CB2 receptors but acts as an indirect antagonist of cannabinoid agonists.[15] It was found to be an antagonist at the putative new cannabinoid receptor, GPR55, a GPCR expressed in the caudate nucleus and putamen.[16] Cannabidiol has also been shown to act as a 5-HT1A receptor agonist.[17]
It appears to relieve convulsion, inflammation, anxiety, and nausea in animal studies.[15] CBD has shown antitumor activity on human breast carcinoma by inhibiting cancer cell growth. At slightly higher concentrations it is cytotoxic to normal cells[18] CBD has a greater affinity for the CB2 receptor than for the CB1 receptor.[15]
CBD shares a precursor with THC and is the main cannabinoid in low-THC Cannabis strains. CBD has been shown to play a role in preventing the short-term memory loss associated with THC.[19]
A 2014 Cochrane review concluded that there was insufficient evidence to conclude that cannabidiol has an anti-psychotic effect.[20] A 2015 systematic review found CBD to be effective as an antipsychotic compound, and may lower the risk for developing cannabis-related psychosis. Trials indicated it was safe and well tolerated.[14]
Cannabinol
Cannabinol (CBN) is the primary product of THC degradation, and there is usually little of it in a fresh plant. CBN content increases as THC degrades in storage, and with exposure to light and air. It is only mildly psychoactive. Its affinity to the CB2 receptor is higher than for the CB1 receptor.[21]
Cannabigerol
Cannabigerol (CBG) is non-psychoactive but still affects the overall effects of Cannabis. CBG has been shown to promote apoptosis in cancer cells and inhibit tumor growth in mice.[22] It acts as an α2-adrenergic receptor agonist, 5-HT1A receptor antagonist, and CB1 receptor antagonist.[23] It also binds to the CB2 receptor.[23]
Tetrahydrocannabivarin
Tetrahydrocannabivarin (THCV) is prevalent in certain central Asian and southern African strains of Cannabis.[24][25] It is an antagonist of THC at CB1 receptors and attenuates the psychoactive effects of THC.[26]
Cannabidivarin
Although cannabidivarin (CBDV) is usually a minor constituent of the cannabinoid profile, enhanced levels of CBDV have been reported in feral cannabis plants from the northwest Himalayas, and in hashish from Nepal.[25][27]
Cannabichromene
Cannabichromene (CBC) is non-psychoactive and does not affect the psychoactivity of THC.[28] CBC has shown antitumor effects in breast cancer xenoplants in mice.[29] More common in tropical cannabis varieties.
Biosynthesis
Cannabinoid production starts when an enzyme causes geranyl pyrophosphate and olivetolic acid to combine and form CBGA. Next, CBGA is independently converted to either CBG, THCA, CBDA or CBCA by four separate synthase, FAD-dependent dehydrogenase enzymes. There is no evidence for enzymatic conversion of CBDA or CBD to THCA or THC. For the propyl homologues (THCVA, CBDVA and CBCVA), there is an analogous pathway that is based on CBGVA from divarinolic acid instead of olivetolic acid.
Double bond position
In addition, each of the compounds above may be in different forms depending on the position of the double bond in the alicyclic carbon ring. There is potential for confusion because there are different numbering systems used to describe the position of this double bond. Under the dibenzopyran numbering system widely used today, the major form of THC is called Δ9-THC, while the minor form is called Δ8-THC. Under the alternate terpene numbering system, these same compounds are called Δ1-THC and Δ6-THC, respectively.
Length
Most classical cannabinoids are 21-carbon compounds. However, some do not follow this rule, primarily because of variation in the length of the side-chain attached to the aromatic ring. In THC, CBD, and CBN, this side-chain is a pentyl (5-carbon) chain. In the most common homologue, the pentyl chain is replaced with a propyl (3-carbon) chain. Cannabinoids with the propyl side-chain are named using the suffix varin, and are designated, for example, THCV, CBDV, or CBNV.
Cannabinoids in other plants
Phytocannabinoids are known to occur in several plant species besides cannabis. These include Echinacea purpurea, Echinacea angustifolia, Echinacea pallida, Acmella oleracea, Helichrysum umbraculigerum, and Radula marginata.[30] The best-known cannabinoids that are not derived from Cannabis are the lipophilic alkamides (alkylamides) from Echinacea species, most notably the cis/trans isomers dodeca-2E,4E,8Z,10E/Z-tetraenoic-acid-isobutylamide.[30] At least 25 different alkylamides have been identified, and some of them have shown affinities to the CB2-receptor.[31][32] In Echinacea species, cannabinoids are found throughout the plant structure, but are most concentrated in the roots and flowers.[33][34] Yangonin found in the Kava plant a ligand to the CB1 receptor.[35] Tea (Camellia sinensis) catechins have an affinity for human cannabinoid receptors.[36] A widespread dietary terpene, beta-caryophyllene, a component from the essential oil of cannabis and other medicinal plants, has also been identified as a selective agonist of peripheral CB2-receptors, in vivo.[37] Black truffles contain anandamide.[38]
Most of the phytocannabinoids are nearly insoluble in water but are soluble in lipids, alcohols, and other non-polar organic solvents.
Cannabis plant profile
Cannabis plants can exhibit wide variation in the quantity and type of cannabinoids they produce. The mixture of cannabinoids produced by a plant is known as the plant's cannabinoid profile. Selective breeding has been used to control the genetics of plants and modify the cannabinoid profile. For example, strains that are used as fiber (commonly called hemp) are bred such that they are low in psychoactive chemicals like THC. Strains used in medicine are often bred for high CBD content, and strains used for recreational purposes are usually bred for high THC content or for a specific chemical balance.
Quantitative analysis of a plant's cannabinoid profile is often determined by gas chromatography (GC), or more reliably by gas chromatography combined with mass spectrometry (GC/MS). Liquid chromatography (LC) techniques are also possible and, unlike GC methods, can differentiate between the acid and neutral forms of the cannabinoids. There have been systematic attempts to monitor the cannabinoid profile of cannabis over time, but their accuracy is impeded by the illegal status of the plant in many countries.
Pharmacology
Cannabinoids can be administered by smoking, vaporizing, oral ingestion, transdermal patch, intravenous injection, sublingual absorption, or rectal suppository. Once in the body, most cannabinoids are metabolized in the liver, especially by cytochrome P450 mixed-function oxidases, mainly CYP 2C9. Thus supplementing with CYP 2C9 inhibitors leads to extended intoxication.
Some is also stored in fat in addition to being metabolized in the liver. Δ9-THC is metabolized to 11-hydroxy-Δ9-THC, which is then metabolized to 9-carboxy-THC. Some cannabis metabolites can be detected in the body several weeks after administration. These metabolites are the chemicals recognized by common antibody-based "drug tests"; in the case of THC or others, these loads do not represent intoxication (compare to ethanol breath tests that measure instantaneous blood alcohol levels), but an integration of past consumption over an approximately month-long window. This is because they are fat-soluble, lipophilic molecules that accumulate in fatty tissues.[39]
Separation
Cannabinoids can be separated from the plant by extraction with organic solvents. Hydrocarbons and alcohols are often used as solvents. However, these solvents are flammable and many are toxic. Butane may be used, which evaporates extremely quickly. Supercritical solvent extraction with carbon dioxide is an alternative technique. Although this process requires high pressures (73 atmospheres or more), there is minimal risk of fire or toxicity, solvent removal is simple and efficient, and extract quality can be well controlled. Once extracted, cannabinoid blends can be separated into individual components using wiped film vacuum distillation or other distillation techniques. However, to produce high-purity cannabinoids, chemical synthesis or semisynthesis is generally required.
History
Cannabinoids were first discovered in the 1940s, when CBD and CBN were identified. The structure of THC was first determined in 1964.
Due to molecular similarity and ease of synthetic conversion, CBD was originally believed to be a natural precursor to THC. However, it is now known that CBD and THC are produced independently in the cannabis plant from the precursor CBG.
Endocannabinoids

Endocannabinoids are substances produced from within the body that activate cannabinoid receptors. After the discovery of the first cannabinoid receptor in 1988, scientists began searching for an endogenous ligand for the receptor.[6][40]
Types of endocannabinoid ligands
Arachidonoylethanolamine (Anandamide or AEA)
In 1992, in Raphael Mechoulam's lab, the first such compound was identified as arachidonoyl ethanolamine and named anandamide, a name derived from the Sanskrit word for bliss and -amide. Anandamide is derived from arachidonic acid. It has a pharmacology similar to THC, although its chemical structure is different. Anandamide binds to the central (CB1) and, to a lesser extent, peripheral (CB2) cannabinoid receptors, where it acts as a partial agonist. Anandamide is about as potent as THC at the CB1 receptor.[41] Anandamide is found in nearly all tissues in a wide range of animals.[42] Anandamide has also been found in plants, including small amounts in chocolate.[43]
Two analogs of anandamide, 7,10,13,16-docosatetraenoylethanolamide and homo-γ-linolenoylethanolamine, have similar pharmacology. All of these are members of a family of signalling lipids called N-acylethanolamines, which also includes the noncannabimimetic palmitoylethanolamide and oleoylethanolamide, which possess anti-inflammatory and orexigenic effects, respectively. Many N-acylethanolamines have also been identified in plant seeds[44] and in molluscs.[45]
2-Arachidonoylglycerol (2-AG)
Another endocannabinoid, 2-arachidonoylglycerol, binds to both the CB1 and CB2 receptors with similar affinity, acting as a full agonist at both.[41] 2-AG is present at significantly higher concentrations in the brain than anandamide,[46] and there is some controversy over whether 2-AG rather than anandamide is chiefly responsible for endocannabinoid signalling in vivo.[1] In particular, one in vitro study suggests that 2-AG is capable of stimulating higher G-protein activation than anandamide, although the physiological implications of this finding are not yet known.[47]
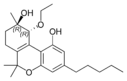
2-Arachidonyl glyceryl ether (noladin ether)
In 2001, a third, ether-type endocannabinoid, 2-arachidonyl glyceryl ether (noladin ether), was isolated from porcine brain.[48] Prior to this discovery, it had been synthesized as a stable analog of 2-AG; indeed, some controversy remains over its classification as an endocannabinoid, as another group failed to detect the substance at "any appreciable amount" in the brains of several different mammalian species.[49] It binds to the CB1 cannabinoid receptor (Ki = 21.2 nmol/L) and causes sedation, hypothermia, intestinal immobility, and mild antinociception in mice. It binds primarily to the CB1 receptor, and only weakly to the CB2 receptor.[41]
N-Arachidonoyl dopamine (NADA)
Discovered in 2000, NADA preferentially binds to the CB1 receptor.[50] Like anandamide, NADA is also an agonist for the vanilloid receptor subtype 1 (TRPV1), a member of the vanilloid receptor family.[51][52]
Virodhamine (OAE)
A fifth endocannabinoid, virodhamine, or O-arachidonoyl-ethanolamine (OAE), was discovered in June 2002. Although it is a full agonist at CB2 and a partial agonist at CB1, it behaves as a CB1 antagonist in vivo. In rats, virodhamine was found to be present at comparable or slightly lower concentrations than anandamide in the brain, but 2- to 9-fold higher concentrations peripherally.[53]
Lysophosphatidylinositol (LPI)
Recent evidence has highlighted lysophosphatidylinositol as the endogenous ligand to novel endocannabinoid receptor GPR55, making it a strong contender as the sixth endocannabinoid.[54]
Function
Endocannabinoids serve as intercellular 'lipid messengers', signaling molecules that are released from one cell and activating the cannabinoid receptors present on other nearby cells. Although in this intercellular signaling role they are similar to the well-known monoamine neurotransmitters, such as acetylcholine and dopamine, endocannabinoids differ in numerous ways from them. For instance, they are used in retrograde signaling between neurons. Furthermore, endocannabinoids are lipophilic molecules that are not very soluble in water. They are not stored in vesicles, and exist as integral constituents of the membrane bilayers that make up cells. They are believed to be synthesized 'on-demand' rather than made and stored for later use. The mechanisms and enzymes underlying the biosynthesis of endocannabinoids remain elusive and continue to be an area of active research.
The endocannabinoid 2-AG has been found in bovine and human maternal milk.[55]
Retrograde signal
Conventional neurotransmitters are released from a ‘presynaptic’ cell and activate appropriate receptors on a ‘postsynaptic’ cell, where presynaptic and postsynaptic designate the sending and receiving sides of a synapse, respectively. Endocannabinoids, on the other hand, are described as retrograde transmitters because they most commonly travel ‘backward’ against the usual synaptic transmitter flow. They are, in effect, released from the postsynaptic cell and act on the presynaptic cell, where the target receptors are densely concentrated on axonal terminals in the zones from which conventional neurotransmitters are released. Activation of cannabinoid receptors temporarily reduces the amount of conventional neurotransmitter released. This endocannabinoid mediated system permits the postsynaptic cell to control its own incoming synaptic traffic. The ultimate effect on the endocannabinoid-releasing cell depends on the nature of the conventional transmitter being controlled. For instance, when the release of the inhibitory transmitter GABA is reduced, the net effect is an increase in the excitability of the endocannabinoid-releasing cell. On the converse, when release of the excitatory neurotransmitter glutamate is reduced, the net effect is a decrease in the excitability of the endocannabinoid-releasing cell.
Range
Endocannabinoids are hydrophobic molecules. They cannot travel unaided for long distances in the aqueous medium surrounding the cells from which they are released, and therefore act locally on nearby target cells. Hence, although emanating diffusely from their source cells, they have much more restricted spheres of influence than do hormones, which can affect cells throughout the body.
Synthetic cannabinoids
Historically, laboratory synthesis of cannabinoids were often based on the structure of herbal cannabinoids, and a large number of analogs have been produced and tested, especially in a group led by Roger Adams as early as 1941 and later in a group led by Raphael Mechoulam. Newer compounds are no longer related to natural cannabinoids or are based on the structure of the endogenous cannabinoids.
Synthetic cannabinoids are particularly useful in experiments to determine the relationship between the structure and activity of cannabinoid compounds, by making systematic, incremental modifications of cannabinoid molecules.
When synthetic cannabinoids are used recreationally, they present significant health dangers to users.[56] In the period of 2012 through 2014, over 10,000 contacts to poison control centers in the United States were related to use of synthetic cannabinoids.[56]
Medications containing natural or synthetic cannabinoids or cannabinoid analogs:
- Dronabinol (Marinol), is Δ9-tetrahydrocannabinol (THC), used as an appetite stimulant, anti-emetic, and analgesic
- Nabilone (Cesamet, Canemes), a synthetic cannabinoid and an analog of Marinol. It is Schedule II unlike Marinol, which is Schedule III
- Rimonabant (SR141716), a selective cannabinoid (CB1) receptor inverse agonist once used as an anti-obesity drug under the proprietary name Acomplia. It was also used for smoking cessation
Other notable synthetic cannabinoids include:
- JWH-018, a potent synthetic cannabinoid agonist discovered by John W. Huffman at Clemson University. It is being increasingly sold in legal smoke blends collectively known as "spice". Several countries and states have moved to ban it legally.
- JWH-073
- CP-55940, produced in 1974, this synthetic cannabinoid receptor agonist is many times more potent than THC.
- Dimethylheptylpyran
- HU-210, about 100 times as potent as THC[57]
- HU-331 a potential anti-cancer drug derived from cannabidiol that specifically inhibits topoisomerase II.
- SR144528, a CB2 receptor antagonist
- WIN 55,212-2, a potent cannabinoid receptor agonist
- JWH-133, a potent selective CB2 receptor agonist
- Levonantradol (Nantrodolum), an anti-emetic and analgesic but not currently in use in medicine
- AM-2201, a potent cannabinoid receptor agonist
Table of plant cannabinoids
| Cannabigerol-type (CBG) | ||||
|---|---|---|---|---|

Cannabigerol |

Cannabigerol |

Cannabinerolic acid A |

Cannabigerovarin |
|

Cannabigerolic acid A |

Cannabigerolic acid A |
Cannabigerovarinic acid A |
||
| Cannabichromene-type (CBC) | ||||

(±)-Cannabichromene |

(±)-Cannabichromenic acid A |

(±)-Cannabivarichromene, (±)-Cannabichromevarin |

(±)-Cannabichromevarinic |
|
| Cannabidiol-type (CBD) | ||||
(−)-Cannabidiol |

Cannabidiol |

Cannabidiol-C4 |

(−)-Cannabidivarin |

Cannabidiorcol |

Cannabidiolic acid |
Cannabidivarinic acid |
|||
| Cannabinodiol-type (CBND) | ||||

Cannabinodiol |

Cannabinodivarin |
|||
| Tetrahydrocannabinol-type (THC) | ||||

Δ9-Tetrahydrocannabinol |
Δ9-Tetrahydrocannabinol-C4 |

Δ9-Tetrahydrocannabivarin |

Δ9-Tetrahydrocannabiorcol | |

Δ9-Tetrahydro- |
Δ9-Tetrahydro- |

Δ9-Tetrahydro- |

Δ9-Tetrahydro- |
Δ9-Tetrahydro- |

(−)-Δ8-trans-(6aR,10aR)- |

(−)-Δ8-trans-(6aR,10aR)- |

(−)-(6aS,10aR)-Δ9- |
||
| Cannabinol-type (CBN) | ||||

Cannabinol |
Cannabinol-C4 |

Cannabivarin |

Cannabinol-C2 |

Cannabiorcol |

Cannabinolic acid A |

Cannabinol methyl ether |
|||
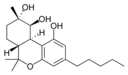
| Cannabitriol-type (CBT) | ||||
-trans-cannabitriol.png)
(−)-(9R,10R)-trans- |
-trans-cannabitriol.png)
(+)-(9S,10S)-Cannabitriol |

(±)-(9R,10S/9S,10R)- |
(−)-(9R,10R)-trans- |
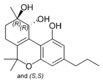
(±)-(9R,10R/9S,10S)- |
-tetrahydrocannabinol.png)
8,9-Dihydroxy-Δ6a(10a)- |

Cannabidiolic acid A |
(−)-(6aR,9S,10S,10aR)- |

(−)-6a,7,10a-Trihydroxy- |
-tetrahydrocannabinol.png)
10-Oxo-Δ6a(10a)- |
| Cannabielsoin-type (CBE) | ||||

(5aS,6S,9R,9aR)- |
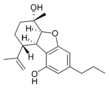
(5aS,6S,9R,9aR)- |
|||
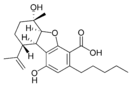
(5aS,6S,9R,9aR)- |

(5aS,6S,9R,9aR)- |

(5aS,6S,9R,9aR)- |
||

Cannabiglendol-C3 |
Dehydrocannabifuran |

Cannabifuran |
||
| Isocannabinoids | ||||

(−)-Δ7-trans-(1R,3R,6R)- |

(±)-Δ7-1,2-cis- |
(−)-Δ7-trans-(1R,3R,6R)- |
||
| Cannabicyclol-type (CBL) | ||||

(±)-(1aS,3aR,8bR,8cR)- |
(±)-(1aS,3aR,8bR,8cR)- |

(±)-(1aS,3aR,8bR,8cR)- |
||
| Cannabicitran-type (CBT) | ||||
Cannabicitran |
||||
| Cannabichromanone-type (CBCN) | ||||
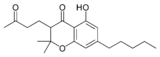
Cannabichromanone |
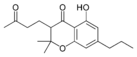
Cannabichromanone-C3 |

Cannabicoumaronone |
||
See also
- Cannabinoid receptor antagonist
- Endocannabinoid enhancer
- Endocannabinoid reuptake inhibitor
- Cancer and nausea § Cannabinoids
References
- 1 2 3 4 Pacher, P.; Bátkai, S; Kunos, G (2006). "The Endocannabinoid System as an Emerging Target of Pharmacotherapy". Pharmacological Reviews 58 (3): 389–462. doi:10.1124/pr.58.3.2. PMC 2241751. PMID 16968947.
- 1 2 Lambert, Didier M.; Fowler, Christopher J. (2005). "The Endocannabinoid System: Drug Targets, Lead Compounds, and Potential Therapeutic Applications". Journal of Medicinal Chemistry 48 (16): 5059–87. doi:10.1021/jm058183t. PMID 16078824.
- ↑ Pertwee, Roger, ed. (2005). Cannabinoids. Springer-Verlag. p. 2. ISBN 3-540-22565-X.
- ↑ "Bulletin on Narcotics – 1962 Issue 3 – 004". UNODC (United Nations Office of Drugs and Crime). 1962-01-01. Retrieved 2014-01-15.
- ↑ El-Alfy, Abir T.; Ivey, Kelly; Robinson, Keisha; Ahmed, Safwat; Radwan, Mohamed; Slade, Desmond; Khan, Ikhlas; Elsohly, Mahmoud; Ross, Samir (2010). "Antidepressant-like effect of Δ9-tetrahydrocannabinol and other cannabinoids isolated from Cannabis sativa L". Pharmacology Biochemistry and Behavior 95 (4): 434–42. doi:10.1016/j.pbb.2010.03.004. PMC 2866040. PMID 20332000.
- 1 2 Devane, WA; Dysarz, FA 3rd; Johnson, MR; Melvin, LS; Howlett, AC (1988). "Determination and characterization of a cannabinoid receptor in rat brain". Mol Pharmacol 34 (5): 605–13. PMID 2848184. Retrieved 6 June 2015.
- ↑ Begg, Malcolm; Pacher, Pál; Batkai, Sándor; Oseihyiaman, Douglas; Offertaler, László; Mo, Fong Ming; Liu, Jie; Kunos, George (2005). "Evidence for novel cannabinoid receptors". Pharmacology & Therapeutics 106 (2): 133–45. doi:10.1016/j.pharmthera.2004.11.005. PMID 15866316.
- ↑ Boron, Walter F.; Boulpaep, Emile L., eds. (2009). Medical Physiology: A Cellular and Molecular Approach. Saunders. p. 331. ISBN 978-1-4160-3115-4.
- 1 2 Pacher, P.; Mechoulam, R. (2011). "Is lipid signaling through cannabinoid 2 receptors part of a protective system?". Progress in Lipid Research 50 (2): 193–211. doi:10.1016/j.plipres.2011.01.001. PMC 3062638. PMID 21295074.
- ↑ Núñez, Estefanía; Benito, Cristina; Pazos, M. Ruth; Barbachano, Antonio; Fajardo, Otto; González, Sara; Tolón, Rosa M.; Romero, Julián (2004). "Cannabinoid CB2 receptors are expressed by perivascular microglial cells in the human brain: An immunohistochemical study". Synapse 53 (4): 208–13. doi:10.1002/syn.20050. PMID 15266552.
- ↑ ElSohly, M. A.; Gul, W. In Handbook of Cannabis; Pertwee, R. G., Ed.; Oxford University Press: Oxford, UK, 2014; Chapter 1, pp 3−22.
- ↑ Fellermeier, Monika; Eisenreich, Wolfgang; Bacher, Adelbert; Zenk, Meinhart H. (2001). "Biosynthesis of cannabinoids". European Journal of Biochemistry 268 (6): 1596–1604. doi:10.1046/j.1432-1327.2001.02030.x. ISSN 0014-2956. PMID 11248677.
- ↑ Patentdocs. Patent application title: Controlled cannabis decarboxylation. US Patent application number: 20120046352. Retrieved 28 December 2013
- 1 2 Iseger, TA; Bossong, MG (March 2015). "A systematic review of the antipsychotic properties of cannabidiol in humans.". Schizophrenia Research 162 (1-3): 153–61. doi:10.1016/j.schres.2015.01.033. PMID 25667194.
- 1 2 3 Mechoulam, Raphael; Peters, Maximilian; Murillo-Rodriguez, Eric; Hanuš, Lumír O. (2007). "Cannabidiol – Recent Advances". Chemistry & Biodiversity 4 (8): 1678–92. doi:10.1002/cbdv.200790147. PMID 17712814.
- ↑ Ryberg, E; Larsson, N; Sjögren, S; Hjorth, S; Hermansson, N-O; Leonova, J; Elebring, T; Nilsson, K; Drmota, T; Greasley, P J (2009). "The orphan receptor GPR55 is a novel cannabinoid receptor". British Journal of Pharmacology 152 (7): 1092–101. doi:10.1038/sj.bjp.0707460. PMC 2095107. PMID 17876302.
- ↑ Russo, Ethan B.; Burnett, Andrea; Hall, Brian; Parker, Keith K. (2005). "Agonistic Properties of Cannabidiol at 5-HT1a Receptors". Neurochemical Research 30 (8): 1037–43. doi:10.1007/s11064-005-6978-1. PMID 16258853.
- ↑ Ligresti A, Moriello AS, Starowicz K, Matias I, Pisanti S, De Petrocellis L, Laezza C, Portella G, Bifulco M, Di Marzo V (2006). "Antitumor activity of plant cannabinoids with emphasis on the effect of cannabidiol on human breast carcinoma". The Journal of Pharmacology and Experimental Therapeutics 318 (3): 1375–87. doi:10.1124/jpet.106.105247. PMID 16728591.
- ↑ Frood, Arron. "Key ingredient staves off marijuana memory loss". Nature. Retrieved 6 October 2015.
- ↑ McLoughlin BC, Pushpa-Rajah JA, Gillies D, Rathbone J, Variend H, Kalakouti E, Kyprianou K (2014). "Cannabis and schizophrenia". Cochrane Database Syst Rev 10: CD004837. doi:10.1002/14651858.CD004837.pub3. PMID 25314586.
- ↑ Mahadevan, Anu; Siegel, Craig; Martin, Billy R.; Abood, Mary E.; Beletskaya, Irina; Razdan, Raj K. (2000). "Novel Cannabinol Probes for CB1 and CB2 Cannabinoid Receptors". Journal of Medicinal Chemistry 43 (20): 3778–85. doi:10.1021/jm0001572. PMID 11020293.
- ↑ Borrelli F, Pagano E, Romano B, Panzera S, Maiello F, Coppola D, De Petrocellis L, Buono L, Orlando P, Izzo AA (2014). "Colon carcinogenesis is inhibited by the TRPM8 antagonist cannabigerol, a Cannabis-derived non-psychotropic cannabinoid". Carcinogenesis 35 (12): 2787–97. doi:10.1093/carcin/bgu205. PMID 25269802.
- 1 2 Cascio, MG; Gauson, LA; Stevenson, LA; Ross, RA; Pertwee, RG (2010). "Evidence that the plant cannabinoid cannabigerol is a highly potent α2-adrenoceptor agonist and moderately potent 5HT1A receptor antagonist". British Journal of Pharmacology 159 (1): 129–41. doi:10.1111/j.1476-5381.2009.00515.x. PMC 2823359. PMID 20002104.
- ↑ Baker, PB; Gough, TA; Taylor, BJ (1980). "Illicitly imported Cannabis products: Some physical and chemical features indicative of their origin". Bulletin on narcotics 32 (2): 31–40. PMID 6907024.
- 1 2 Hillig, K. W.; Mahlberg, P. G. (2004). "A chemotaxonomic analysis of cannabinoid variation in Cannabis (Cannabaceae)". American Journal of Botany 91 (6): 966–75. doi:10.3732/ajb.91.6.966. PMID 21653452.
- ↑ Thomas, Adèle; Stevenson, Lesley A; Wease, Kerrie N; Price, Martin R; Baillie, Gemma; Ross, Ruth A; Pertwee, Roger G (2005). "Evidence that the plant cannabinoid Δ9-tetrahydrocannabivarin is a cannabinoid CB1and CB2receptor antagonist". British Journal of Pharmacology 146 (7): 917–26. doi:10.1038/sj.bjp.0706414. PMC 1751228. PMID 16205722.
- ↑ Merkus, Frans W. H. M. (1971). "Cannabivarin and Tetrahydrocannabivarin, Two New Constituents of Hashish". Nature 232 (5312): 579–80. doi:10.1038/232579a0. PMID 4937510.
- ↑ Ilan, A. B.; Gevins, A.; Coleman, M.; Elsohly, M. A.; De Wit, H. (2005). "Neurophysiological and subjective profile of marijuana with varying concentrations of cannabinoids". Behavioural Pharmacology 16 (5–6): 487–96. doi:10.1097/00008877-200509000-00023. PMID 16148455.
- ↑ http://jpet.aspetjournals.org/content/318/3/1375.long
- 1 2 Bauer, Rudolf; Salo-Ahen, Karin; Bauer, Outi (2008). "CB Receptor Ligands from Plants". Current Topics in Medicinal Chemistry 8 (3): 173–86. doi:10.2174/156802608783498023. PMID 18289087.
- ↑ Bauer, R.; Remiger, P. (2007). "TLC and HPLC Analysis of Alkamides in Echinacea Drugs1,2". Planta Medica 55 (4): 367–71. doi:10.1055/s-2006-962030. PMID 17262436.
- ↑ Raduner, S; Majewska, A; Chen, J; Xie, X; Hamon, J; Faller, B; Altmann, K; Gertsch, J (2006). "Alkylamides from Echinacea Are a New Class of Cannabinomimetics: CANNABINOID TYPE 2 RECEPTOR-DEPENDENT AND -INDEPENDENT IMMUNOMODULATORY EFFECTS" (PDF). J. Biol. Chem. 281 (20): 14192–14206. doi:10.1074/jbc.M601074200. PMID 16547349.
- ↑ Perry, Nigel; Van Klink, John; Burgess, Elaine; Parmenter, Graeme (2007). "Alkamide Levels inEchinacea purpurea: A Rapid Analytical Method Revealing Differences among Roots, Rhizomes, Stems, Leaves and Flowers". Planta Medica 63 (1): 58–62. doi:10.1055/s-2006-957605. PMID 17252329.
- ↑ He, X; Lin, L; Bernart, MW; Lian, L (1998). "Analysis of alkamides in roots and achenes of Echinacea purpurea by liquid chromatography–electrospray mass spectrometry". Journal of Chromatography A 815 (2): 205–11. doi:10.1016/S0021-9673(98)00447-6.
- ↑ Ligresti, A.; Villano, R.; Allarà, M.; Ujváry, I. N.; Di Marzo, V. (2012). "Kavalactones and the endocannabinoid system: The plant-derived yangonin is a novel CB1 receptor ligand". Pharmacological Research 66 (2): 163–169. doi:10.1016/j.phrs.2012.04.003. PMID 22525682.
- ↑ Korte, G.; Dreiseitel, A.; Schreier, P.; Oehme, A.; Locher, S.; Geiger, S.; Heilmann, J.; Sand, P.G. (2010). "Tea catechins' affinity for human cannabinoid receptors". Phytomedicine 17 (1): 19–22. doi:10.1016/j.phymed.2009.10.001. PMID 19897346.
- ↑ Gertsch, J; Leonti, M; Raduner, S; Racz, I; Chen, J; Xie, X; Altmann, K; Karsak, M; Zimmer, A (2008). "Beta-caryophyllene is a dietary terpene". PNAS 105 (26): 9099–9104. doi:10.1073/pnas.0803601105. PMC 2449371. PMID 18574142.
- ↑ Truffles contain endocannabinoid metabolic enzymes and anandamide Phytochemistry, Available online 26 November 2014.
- ↑ Ashton CH (February 2001). "Pharmacology and effects of cannabis: a brief review". Br J Psychiatry 178 (2): 101–106. doi:10.1192/bjp.178.2.101. PMID 11157422.
Because they are extremely lipid soluble, cannabinoids accumulate in fatty tissues, reaching peak concentrations in 4-5 days. They are then slowly released back into other body compartments, including the brain. They are then slowly released back into other body compartments, including the brain. Because of the sequestration in fat, the tissue elimination half-life of THC is about 7 days, and complete elimination of a single dose may take up to 30 days.
- ↑ Katona I, Freund TF (2012). "Multiple functions of endocannabinoid signaling in the brain". Annual Review of Neuroscience 35: 529–58. doi:10.1146/annurev-neuro-062111-150420. PMC 4273654. PMID 22524785.
- 1 2 3 Grotenhermen, Franjo (2005). "Cannabinoids". Current Drug Target -CNS & Neurological Disorders 4 (5): 507–530. doi:10.2174/156800705774322111.
- ↑ Martin, B.R.; Mechoulam, R.; Razdan, R.K. (1999). "Discovery and characterization of endogenous cannabinoids". Life Sciences 65 (6–7): 573–595. doi:10.1016/S0024-3205(99)00281-7.
- ↑ Di Tomaso, Emmanuelle; Beltramo, Massimiliano; Piomelli, Daniele (1996). "Brain cannabinoids in chocolate". Nature 382 (6593): 677–8. doi:10.1038/382677a0. PMID 8751435.
- ↑ Chapman, K. D.; Venables, B; Markovic, R; Blair Jr, RW; Bettinger, C (1999). "N-Acylethanolamines in Seeds. Quantification of Molecular Species and Their Degradation upon Imbibition". Plant Physiology 120 (4): 1157–64. doi:10.1104/pp.120.4.1157. PMC 59349. PMID 10444099.
- ↑ Sepe, Nunzio; De Petrocellis, Luciano; Montanaro, Francesca; Cimino, Guido; Di Marzo, Vincenzo (1998). "Bioactive long chain N-acylethanolamines in five species of edible bivalve molluscs". Biochimica et Biophysica Acta (BBA) - Lipids and Lipid Metabolism 1389 (2): 101–11. doi:10.1016/S0005-2760(97)00132-X. PMID 9461251.
- ↑ Piomelli, Daniele; Schweitzer, Nephi; Piomelli, Paul (1997). "A second endogenous cannabinoid that modulates long-term potentiation". Nature 388 (6644): 773–8. doi:10.1038/42015. PMID 9285589.
- ↑ Savinainen, Juha R; Järvinen, Tomi; Laine, Krista; Laitinen, Jarmo T (2001). "Despite substantial degradation, 2-arachidonoylglycerol is a potent full efficacy agonist mediating CB1receptor-dependent G-protein activation in rat cerebellar membranes". British Journal of Pharmacology 134 (3): 664–72. doi:10.1038/sj.bjp.0704297. PMC 1572991. PMID 11588122.
- ↑ Hanuš, Lumír; Abu-Lafi, Saleh; Fride, Ester; Breuer, Aviva; Vogel, Zvi; Shalev, Deborah E.; Kustanovich, Irina; Mechoulam, Raphael (2001). "2-Arachidonyl glyceryl ether, an endogenous agonist of the cannabinoid CB1 receptor". Proceedings of the National Academy of Sciences 98 (7): 3662–5. doi:10.1073/pnas.061029898. PMC 31108. PMID 11259648.
- ↑ Oka, Saori; Tsuchie, Akiko; Tokumura, Akira; Muramatsu, Mayumi; Suhara, Yoshitomo; Takayama, Hiroaki; Waku, Keizo; Sugiura, Takayuki (2003). "Ether-linked analogue of 2-arachidonoylglycerol (noladin ether) was not detected in the brains of various mammalian species". Journal of Neurochemistry 85 (6): 1374–81. doi:10.1046/j.1471-4159.2003.01804.x. PMID 12787057.
- ↑ Bisogno, Tiziana; Melck, Dominique; Bobrov, Mikhail Yu.; Gretskaya, Natalia M.; Bezuglov, Vladimir V.; De Petrocellis, Luciano; Di Marzo, Vincenzo (2000). "N-acyl-dopamines: Novel synthetic CB1 cannabinoid-receptor ligands and inhibitors of anandamide inactivation with cannabimimetic activity in vitro and in vivo". Biochemical Journal 351 (3): 817–24. doi:10.1042/0264-6021:3510817. PMC 1221424. PMID 11042139.
- ↑ Bisogno, T; Ligresti, A; Dimarzo, V (2005). "The endocannabinoid signalling system: Biochemical aspects". Pharmacology Biochemistry and Behavior 81 (2): 224–38. doi:10.1016/j.pbb.2005.01.027. PMID 15935454.
- ↑ Ralevic, Vera (2003). "Cannabinoid modulation of peripheral autonomic and sensory neurotransmission". European Journal of Pharmacology 472 (1–2): 1–21. doi:10.1016/S0014-2999(03)01813-2. PMID 12860468.
- ↑ Porter, A. C.; Sauer, JM; Knierman, MD; Becker, GW; Berna, MJ; Bao, J; Nomikos, GG; Carter, P; Bymaster, FP; Leese, AB; Felder, CC (2002). "Characterization of a Novel Endocannabinoid, Virodhamine, with Antagonist Activity at the CB1 Receptor". Journal of Pharmacology and Experimental Therapeutics 301 (3): 1020–4. doi:10.1124/jpet.301.3.1020. PMID 12023533.
- ↑ Piñeiro, Roberto; Falasca, Marco (2012). "Lysophosphatidylinositol signalling: New wine from an old bottle". Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids 1821 (4): 694–705. doi:10.1016/j.bbalip.2012.01.009. PMID 22285325.
- ↑ Fride, E; Bregman, T; Kirkham, TC (2005). "Endocannabinoids and food intake: Newborn suckling and appetite regulation in adulthood". Experimental biology and medicine 230 (4): 225–34. PMID 15792943.
- 1 2 "N-(1-amino-3-methyl-1-oxobutan-2-yl)-1-(cyclohexylmethyl)-1H-indazole-3-carboxamide(AB-CHMINACA), N-(1-amino-3-methyl-1-oxobutan-2-yl)-1-pentyl-1H-indazole-3-carboxamide (AB-PINACA)and[1-(5-fluoropentyl)-1H-indazol-3-yl](naphthalen-1-yl)methanone(THJ-2201)" (PDF). Drug and Chemical Evaluation Section, Office of Diversion Control, Drug Enforcement Administration. December 2014.
- ↑ "More medicinal uses for marijuana". Marijuana.org. October 18, 2005. Archived from the original on 2005-12-21. Retrieved 2014-01-15.
Further reading
- De Meijer, EP; Bagatta, M; Carboni, A; Crucitti, P; Moliterni, VM; Ranalli, P; et al. (2003). "The inheritance of chemical phenotype in Cannabis sativa L". Genetics 163 (1): 335–46. PMC 1462421. PMID 12586720.
- Devane, W.; Hanus, L; Breuer, A; Pertwee, R.; Stevenson, L.; Griffin, G; et al. (1992). "Isolation and structure of a brain constituent that binds to the cannabinoid receptor". Science 258 (5090): 1946–9. Bibcode:1992Sci...258.1946D. doi:10.1126/science.1470919. PMID 1470919.
- Elsohly, Mahmoud A.; Slade, Desmond (2005). "Chemical constituents of marijuana: The complex mixture of natural cannabinoids". Life Sciences 78 (5): 539–48. doi:10.1016/j.lfs.2005.09.011. PMID 16199061.
- Hanus, Lumir; Gopher, Asher; Almog, Shlomo; Mechoulam, Raphael (1993). "Two new unsaturated fatty acid ethanolamides in brain that bind to the cannabinoid receptor". Journal of Medicinal Chemistry 36 (20): 3032–4. doi:10.1021/jm00072a026. PMID 8411021.
- Hanus, L (1987). "Biogenesis of cannabinoid substances in the plant". Acta Universitatis Palackianae Olomucensis Facultatis Medicae 116: 47–53. PMID 2962461.
- Hanuš, L.; Krejčí, Z. (1975). "Isolation of two new cannabinoid acids from Cannabis sativa L. of Czechoslovak origin". Acta Univ. Olomuc., Fac. Med 74: 161–166.
- Hanuš, L.; Krejčí, Z.; Hruban, L. (1975). "Isolation of cannabidiolic acid from Turkish variety of cannabis cultivated for fibre". Acta Univ. Olomuc., Fac. Med 74: 167–172.
- Köfalvi, Attila, ed. (2008). "Cannabinoids and the Brain". doi:10.1007/978-0-387-74349-3. ISBN 978-0-387-74348-6.
- Mechoulam, Raphael; Ben-Shabat, Shimon; Hanus, Lumir; Ligumsky, Moshe; Kaminski, Norbert E.; Schatz, Anthony R.; et al. (1995). "Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors". Biochemical Pharmacology 50 (1): 83–90. doi:10.1016/0006-2952(95)00109-D. PMID 7605349.
- Nicoll, Roger A.; Alger, Bradley E. (2004). "The Brain's Own Marijuana". Scientific American 291 (6): 68–75. doi:10.1038/scientificamerican1204-68. PMID 15597982.
- Racz, I.; Nadal, X.; Alferink, J.; Baños, J. E.; Rehnelt, J.; Martín, M.; et al. (2008). "Interferon- is a Critical Modulator of CB2 Cannabinoid Receptor Signaling during Neuropathic Pain". Journal of Neuroscience 28 (46): 12136–45. doi:10.1523/JNEUROSCI.3402-08.2008. PMC 3844840. PMID 19005078.
- Racz, I.; Nadal, X.; Alferink, J.; Baños, J. E.; Rehnelt, J.; Martín, M.; et al. (2008). "Crucial Role of CB2 Cannabinoid Receptor in the Regulation of Central Immune Responses during Neuropathic Pain". Journal of Neuroscience 28 (46): 12125–35. doi:10.1523/JNEUROSCI.3400-08.2008. PMC 3844839. PMID 19005077.
- Turner, C. E.; Mole, M. L.; Hanus, L.; Elsohly, H. N. (1981). "Constituents of Cannabis sativa. XIX. Isolation and Structure Elucidation of Cannabiglendol, A Novel Cannabinoid from an Indian Variant". Journal of Natural Products 44 (1): 27–33. doi:10.1021/np50013a005.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
