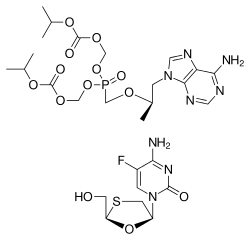
Tenofovir/emtricitabine
 | |
|
| |
| Combination of | |
|---|---|
| Tenofovir disoproxil | Nucleotide analogue reverse transcriptase inhibitor |
| Emtricitabine | Nucleoside reverse transcriptase inhibitor |
| Clinical data | |
| Trade names | Truvada |
| AHFS/Drugs.com | entry |
| Pregnancy category |
|
| Legal status |
|
| Routes of administration | Oral |
| Identifiers | |
| ATC code | J05AR03 |
| PubChem | CID 11954236 |
| NIAID ChemDB | 214126 |
| (verify) | |
Tenofovir disoproxil/emtricitabine (trade name Truvada) is a fixed-dose combination of two antiretroviral drugs used for the treatment of HIV/AIDS. It was developed by Gilead Sciences and consists of 300 milligrams of tenofovir disoproxil fumarate (of which 245 mg is tenofovir disoproxil, equalling 136 mg tenofovir) and 200 milligrams of emtricitabine.
The drug has been approved for pre-exposure prophylaxis against HIV infection. The Food and Drug Administration approved it for prophylactic use on July 16, 2012.[1] In studies, tenofovir reduced the incidence of HIV infection, especially in high-risk individuals, (by 42% in MSM in the iPrEx study) but produced conflicting results in other studies (notably the FEM-PrEP study in heterosexual African women). One study estimated through mathematical modeling that daily intake of Truvada could potentially achieve a 99% of risk reduction of contracting HIV in high risk individuals.[2] Another study, iPrEX OLE, showed overall PrEP effectiveness of 50% rising to 100% when participants took the drug four or more times per week.[3] A Cochrane review found that both tenofovir alone, as well as the tenofovir/emtricitabine combination, decreased the risk of contracting HIV by 51% (RR 0.51; 95% CI 0.30 to 0.86; 8918 participants).[4]
In certain studies, the drug has demonstrated rare side effects including: transient nausea, dizziness, loss of appetite, and loose stools.[5]
Uses
Truvada is used to prevent HIV infection. In combination with other drugs, it may be used to treat HIV.
Available forms
Truvada is a tablet taken by mouth.[6]
Lactation
In pregnancy and lactation, Truvada was shown to be secreted in breast milk.[7]
Clinical studies
The HEAT study (randomized, double-blind, placebo-matched, multicentre) showed that once-daily emtricitabine/tenofovir plus lopinavir/ritonavir or boosted atazanavir or efavirenz were effective in the initial treatment of patients with HIV-1 infection (with screening plasma HIV-1 RNA levels of ≥1,000,000 copies/mL in ACTG 5202).[8]
In other randomized trials, emtricitabine/tenofovir DF 200 mg/300 mg once daily was an effective backbone for boosted protease inhibitor (PI)-based regimens in the initial treatment of HIV-1 infection.[8][9]
Emtricitabine/tenofovir DF in combination with various boosted PIs was generally well tolerated by adults with HIV-1 infection.[8]
Truvada was developed by Gilead Sciences and approved by the United States Food and Drug Administration in 2004.
A combination pill containing Truvada and efavirenz (Sustiva) is also available and is marketed as Atripla.
Contraindications
Truvada should not be taken by patients with an unknown or a positive HIV-1 form of the disease for pre-exposure prophylaxis. Patients who are infected with HIV should use Truvada only in combination with other antiretroviral medications.[10]
Pre-exposure prophylaxis
Currently the FDA recommends pre-exposure prophylactic (PrEP) considerations for the following high risk groups:[11]
- Gay or bisexual men who have either have had anal sex without a condom or been diagnosed with an STD in the past 6 months
- Heterosexual men or women who do not regularly use condoms during sex with partners of unknown HIV status who are substantial risk
- Injection of illicit drugs in the last month with sharing of equipment
- Discordant heterosexual and homosexual partners where one partner is HIV-positive and the other HIV-negative
The consideration of utilizing Truvada as a reduction strategy involves discussion with a health professional who can help the patient navigate the benefits and risks. Patients who start taking Truvada see HIV reduction benefit up to 72 hours after starting, but the medicine must be taken for thirty days after a high-risk sexual event to ensure HIV transmission levels are optimally reduced.[12]
Monitoring Parameters for PrEP:[13]
- HIV-1 negative test confirmation at initiation. Delay initiation by 1 month if viral infection symptoms are present.
- Hepatitis B screening should be considered at initiation. Patient should consider vaccination if not completed.
- Follow up HIV-1 screening tests required every two to three months. Truvada should be discontinued if an HIV diagnosis is confirmed to combat drug resistance.
- Screening for other sexually transmitted infections every 3 to 6 months that have shown to facilitate HIV infection, such as gonorrhea and chlamydia.
- Periodic renal function tests should be performed throughout therapy.
PrEP Counseling:[13]
Medication adherence is a significant peril of prophylactic treatment and should be assessed and counseled at every visit. Truvada only works when it is taken regularly. Patients should understand that Truvada is a reduction strategy and should be combined with other risk reduction and safer sex strategies
Adverse reactions
Truvada is generally well-tolerated in patients. Some of its side effects include:[14]
- Rare: lactic acidosis, liver dysfunction, worsening of Hepatitis B infection
- Common: headache, abdominal pain, and decreased weight, nausea, diarrhea
Drug interactions
The tenofovir component of Truvada interacts with the following drugs: didanosine, atazanavir, and lopinavir/ritonavir.
When tenofovir is coadministered with didanosine, the concentration of didanosine increases, and may lead to didanosine toxicity which may result in complications such as pancreatitis and neuropathy. If authorised, the dose of didanosine may be reduced or discontinued completely.
The coadministration of tenofovir and atazanavir results in decreased concentrations of atazanavir and increased concentrations of tenofovir. Atazanavir may be taken with Truvada only with ritonavir and must be monitored for tenofovir toxicity.
The coadministration of tenofovir and lopinavir/ritonavir increases the concentration of tenofovir and must be monitored for tenofovir toxicity.[15]
Other drugs with adverse reactions include adefovir, dabigatran etexilate, lamivudine, and vincristine.
Adefovir: May reduce the therapeutic effect of tenofovir.
Dabigatran Etexilate: Avoid using dabigatran with p-glycoprotein inducers. If dabigatran and p-glycoprotein inducers are used concurrently, monitor for decreased levels/effects of dabigatran.
Lamivudine: May increase the adverse/toxic effect of emtricitabine.
Vincristine (Liposomal): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of vincristine.[16]
Cost
As of 2014, the median wholesale cost per tablet, worldwide, was US $.2028.[6]
References
- ↑ "FDA approves first pill to help prevent HIV". Seattle Times. 16 July 2012.
- ↑ "PK Modeling of Daily TDF/FTC (Truvada) Provides Close to 100% Protection Against HIV Infection". April 2012.
- ↑ "Overall PrEP effectiveness in iPrEx OLE study 50%, but 100% in those taking four or more doses a week". July 2014.
- ↑ Okwundu CI, Uthman OA, Okoromah CAN (2012). Okwundu, Charles I, ed. "Antiretroviral pre-exposure prophylaxis (PrEP) for preventing HIV in high-risk individuals". Cochrane Database Syst Rev 7 (7): CD007189. doi:10.1002/14651858.CD007189.pub3. PMID 22786505.
- ↑ MedicineNet.com. http://www.medicinenet.com/emtricitabine-tenofovir-oral/article.htm
- 1 2 "Tenofovir DF+Emtricitabine". International Drug Price Indicator Guide. Management Sciences for Health and World Health Organization. 2014. Retrieved 2015-08-01.
- ↑ "Recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States" (PDF). http://nih.gov. National Institutes of Health. Retrieved 21 October 2014. External link in
|website=(help) - 1 2 3 Perry CM (2009). "Emtricitabine/tenofovir disoproxil fumarate: in combination with a protease inhibitor in HIV-1 infection". Drugs 69 (7): 843–57. doi:10.2165/00003495-200969070-00005. PMID 19441871.
- ↑ Cohen J (December 2010). "HIV/AIDS clinical trials. A powerful and perplexing new HIV prevention tool". Science 330 (6009): 1298–9. doi:10.1126/science.330.6009.1298. PMID 21127220.
- ↑ Truvada 2012, p. 1.
- ↑ "CDC - Pre-Exposure Prophylaxis (PrEP) - Research - Prevention Research - HIV/AIDS". Retrieved 4 June 2015.
- ↑ "Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HIV and Recommendations for Postexposure Prophylaxis". Retrieved 4 June 2015. line feed character in
|title=at position 55 (help) - 1 2 "TRUVADA for a PrEP Indication - Checklist for Prescribers". Retrieved 4 June 2015.
- ↑ "TRUVADA® Side Effects". Retrieved 4 June 2015.
- ↑ Truvada 2012, p. 2.
- ↑ Ramanathan, S; Shen, G; Cheng, A; Kearney, P (2007). "Pharmacokinetics of emtricitabine, tenofovir, and GS-9137 following coadministration of emtricitabine/tenofovir disoproxil fumarate, and ritonavir-boosted GS-9137.". J Acquir Immune Defic Syndr 3 (45): 277.
- Truvada [package insert]. Foster City, CA: Gilead Sciences, Inc.; 2012.
External links
- Truvada website, run by Gilead Sciences
- Global iPrEx study website