Echinocandin
Echinocandins are antifungal drugs that inhibit the synthesis of glucan in the cell wall, via noncompetitive inhibition of the enzyme 1,3-β glucan synthase[1][2] and are thus called "penicillin of antifungals"[3] (a property shared with papulacandins) as penicillin has a similar mechanism against bacteria but not fungi. Beta glucans are carbohydrate polymers that are cross-linked with other fungal cell wall components (The bacterial equivalent is peptidoglycan). Caspofungin, micafungin, and anidulafungin are semisynthetic echinocandin derivatives with clinical use due to their solubility, antifungal spectrum, and pharmacokinetic properties.[4]
Medical uses
Drugs and drug candidates in this class are fungicidal against some yeasts (most species of Candida, but not against Cryptococcus, Trichosporon, and Rhodotorula). Echinocandins also have displayed activity against Candida biofilms, especially in synergistic activity with amphotericin B and additive activity with fluconazole. Echinocandins are fungistatic against some molds (Aspergillus, but not Fusarium and Rhizopus), and modestly or minimally active against dimorphic fungi (Blastomyces and Histoplasma). These have some activity against the spores of the fungus Pneumocystis carinii. Caspofungin is used in the treatment of febrile neutropenia and as salvage therapy for the treatment of invasive aspergillosis.[5] Micafungin is used as prophylaxis against Candida infections in hematopoietic stem cell transplantation patients.[5]
Side effects
Echinocandin toxicity is uncommon. Its use has been associated with elevated aminotransferases and alkaline phosphatase levels.[6]
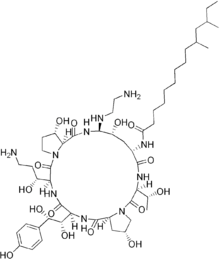
Chemistry
The present-day clinically used echinocandins are semisynthetic pneumocandins, which are chemically lipopeptide in nature, consisting of large cyclic (hexa)peptoid. Caspofungin, micafungin, and anidulafungin are similar cyclic hexapeptide antibiotics linked to long modified N-linked acyle fatty acid chains. The chains act as anchors on the fungal cell membrane to help facilitate antifungal activity.[7] Due to their limited oral bioavailability, echinocandins are administered through intravenous infusion.
Mechanism of action
Echinocandins noncompetitively inhibit beta-1,3-D-glucan synthase enzyme complex in susceptible fungi to disturb fungal cell glucan synthesis.[8] Beta-glucan destruction prevents resistance against osmotic forces, which leads to cell lysis.[9] They have fungistatic activity against Aspergillus species. and fungicidal activity against most Candida spp., including strains that are fluconazole-resistant.[5] In vitro and mouse models show echinocandins may also enhance host immune responses by exposing highly antigenic beta-glucan epitopes that can accelerating host cellular recognition and inflammatory responses.[10]
Resistance
Echinocandin resistance is rare. However, cases studies have shown some resistance in C. albicans, C. glabrata, C. lusitaniae, C. tropicalis, and C. parapsilosis. Resistances include alterations in the glucan synthase (Fks1-Fks2 complex) and overexpression of efflux pumps, as well as alterations and/or overexpressions in Erg3 and Erg11.
Pharmacokinetics
Due to the large molecular weight of echinocandins, they have poor oral bioavailability and are administered by intravenous infusion. In addition, their large structures limit penetration into cerebrospinal fluid, urine, and eyes. In plasma, echinocandins have a high affinity to serum proteins. Echinocandins do not have primary interactions with CYP450 or P-glycoprotein pumps. Caspofungin has triphasic nonlinear pharmacokinetics, while micafungin (hepatically metabolized by arylsulfatase, catechol O-methyltransferase, and hydroxylation) and anidulafungin (degraded spontaneously in the system and excreted mostly as a metabolite in the urine) have linear elimination.[6][11][12] Younger patients exhibit a faster rate of elimination of micafungin and caspofungin.[13]
Interference
Caspofungin has some interference with ciclosporin metabolism, and micafungin has some interference with sirolimus (rapamycin), but anidulafungin needs no dose adjustments when given with ciclosporin, tacrolimus, or voriconazole.[14]
Advantages
Advantages of echinocandins:
- broad range (especially against all Candida), thus can be given empirically in febrile neutropenia and stem cell transplant
- can be used in case of azole-resistant Candida or use as a second-line agent for refractory aspergillosis
- long half-life (polyphasic elimination: alpha phase 1–2 hours + beta phase 9–11 hours + gamma phase 40–50 hours)
- low toxicity: only histamine release (3%), fever (2.9%), nausea and vomiting (2.9%), and phlebitis at the injection site (2.9%), very rarely allergy and anaphylaxis
- not an inhibitor, inducer, or substrate of the cytochrome P450 system, or P-glycoprotein, thus minimal drug interactions
- lack of interference from renal failure and hemodialysis
- no dose adjustment is necessary based on age, gender, race
- better (or no less effective) than amphotericin B and fluconazole against yeast infections
Disadvantages
Disadvantages of echinocandins:
- embryotoxic[15] (category C) thus should be avoided if possible in pregnancy
- needs dose adjustment in liver disease
- poor ocular penetration in fungal endophthalmitis[16]
Examples
List of echinocandins:
- Pneumocandins (cyclic hexapeptides linked to a long-chain fatty acid)
- Echinocandin B not clinically used, risk of hemolysis
- Cilofungin withdrawn from trials due to solvent toxicity
- Caspofungin (trade name Cancidas, by Merck)
- Micafungin (FK463) (trade name Mycamine, by Astellas Pharma.)
- Anidulafungin (VER-002, V-echinocandin, LY303366) (trade name Eraxis, by Pfizer)
History
Discovery of echinocandins stemmed from studies on papulacandins isolated from a strain of Papularia sphaerosperma (Pers.), which were liposaccharide - i.e., fatty acid derivatives of a disaccharide that also blocked the same target, 1,3-β glucan synthase - and had action only on Candida spp. (narrow spectrum). Screening of natural products of fungal fermentation in the 1970s led to the discovery of echinocandins, a new group of antifungals with broad-range activity against Candida spp. One of the first echinocandins of the pneumocandin type, discovered in 1974, echinocandin B, could not be used clinically due to risk of high degree of hemolysis. Screening semisynthetic analogs of the echinocandins gave rise to cilofungin, the first echinofungin analog to enter clinical trials, in 1980, which, it is presumed, was later withdrawn for a toxicity due to the solvent system needed for systemic administration. The semisynthetic pneumocandin analogs of echinocandins were later found to have the same kind of antifungal activity, but low toxicity. The first approved of these newer echinocandins was caspofungin, and later micafungin and anidulafungin were also approved. All these preparations so far have low oral bioavailability, so must be given intravenously only. Echinocandins have now become one of the first-line treatments for Candida before the species are identified, and even as antifungal prophylaxis in hematopoietic stem cell transplant patients.
See also
References
- ↑ Morris MI, Villmann M (September 2006). "Echinocandins in the management of invasive fungal infections, part 1". Am J Health Syst Pharm 63 (18): 1693–703. doi:10.2146/ajhp050464.p1. PMID 16960253.
- ↑ Morris MI, Villmann M (October 2006). "Echinocandins in the management of invasive fungal infections, Part 2". Am J Health Syst Pharm 63 (19): 1813–20. doi:10.2146/ajhp050464.p2. PMID 16990627.
- ↑ http://www.clevelandclinicmeded.com/medicalpubs/pharmacy/mayjune2003/antifungal.htm.
- ↑ Debono, M; Gordee, RS (1994). "Antibiotics that inhibit fungal cell wall development". Annu Rev Microbiol 48: 471–497. doi:10.1146/annurev.mi.48.100194.002351.
- 1 2 3 Sucher, AJ; Chahine, EB; Balcer, HE (Oct 2009). "Echinocandins: the newest class of antifungals". Ann Pharmacother 43 (10): 1647–57. doi:10.1345/aph.1M237.
- 1 2 Cancidas. Prescribing information-(caspofungin acetate) for injection. Merck & Co Inc, Whitehouse Station, NJ 2008.
- ↑ Denning, DW (2003). "Echinocandin antifungal drugs". Lancet 362: 1142–1151. doi:10.1016/s0140-6736(03)14472-8.
- ↑ Douglas, CM (2001). "Fungal beta(1,3)-D-glucan synthesis". Med Mycol 39 (Suppl 1): 55–66. doi:10.1080/mmy.39.1.55.66.
- ↑ Beauvais, A; Latgé, JP (2001). "Membrane and cell wall targets in Aspergillus fumigatus". Drug Resist Updat 4: 38–49. doi:10.1054/drup.2001.0185.
- ↑ Wheeler, RT; Fink, GR (2006). "A drug-sensitive genetic network masks fungi from the immune system". PLoS Pathog 2: e35. doi:10.1371/journal.ppat.0020035.
- ↑ Dodds Ashley, ES; Lewis, R; Lewis, JS; et al. (2006). "Pharmacology of Systemic Antifungal Agents". Clin Infect Dis 43 (Suppl 1): S28. doi:10.1086/504492.
- ↑ Boucher, HW; Groll, AH; Chiou, CC; Walsh, TJ (2004). "Newer systemic antifungal agents : pharmacokinetics, safety and efficacy". Drugs 64: 1997–2020. doi:10.2165/00003495-200464180-00001.
- ↑ Lehrnbecher, T; Groll, AH (2010). "Micafungin: a brief review of pharmacology, safety, and antifungal efficacy in pediatric patients". Pediatr Blood Cancer 55: 229–232. doi:10.1002/pbc.22449.
- ↑ Harroison's Principle of Internal Medicine
- ↑ "Pharmacotherapy Update - New Antifungal Agents: Additions to the Existing Armamentarium (Part 1)".
- ↑ Gauthier GM, Nork TM, Prince R, Andes D (August 2005). "Subtherapeutic ocular penetration of caspofungin and associated treatment failure in Candida albicans endophthalmitis". Clin. Infect. Dis. 41 (3): e27–8. doi:10.1086/431761. PMID 16007519.