Deoxycholic acid
 | |
 | |
 | |
| Names | |
|---|---|
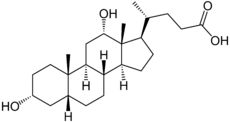
| IUPAC name
(3α,5β,12α,20R)-3,12-Dihydroxycholan-24-oic acid | |
| Other names
Deoxycholic acid Deoxycholate Kybella | |
| Identifiers | |
| 83-44-3 | |
| ChEBI | CHEBI:28834 |
| ChEMBL | ChEMBL406393 |
| ChemSpider | 193196 |
| DrugBank | DB07690 |
| 610 | |
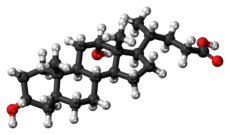
| Jmol interactive 3D | Image |
| PubChem | 222528 |
| UNII | 005990WHZZ |
| |
| |
| Properties | |
| C24H40O4 | |
| Molar mass | 392.58 g·mol−1 |
| Melting point | 174–176 °C (345–349 °F; 447–449 K) |
| 0.024%[1] | |
| Acidity (pKa) | 6.58[2] |
| Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| | |
| Infobox references | |
Deoxycholic acid, also known as deoxycholate, cholanoic acid, and 3α,12α-dihydroxy-5β-cholan-24-oic acid, is a bile acid. Deoxycholic acid is one of the secondary bile acids, which are metabolic byproducts of intestinal bacteria. The two primary bile acids secreted by the liver are cholic acid and chenodeoxycholic acid. Bacteria metabolize chenodeoxycholic acid into the secondary bile acid lithocholic acid, and they metabolize cholic acid into deoxycholic acid. There are additional secondary bile acids, such as ursodeoxycholic acid. Deoxycholic acid is soluble in alcohol and acetic acid. When pure, it comes in a white to off-white crystalline powder form.
Applications
Deoxycholic acid has been used since its discovery in various fields of human medicine. In the human body deoxycholic acid is used in the emulsification of fats for the absorption in the intestine. It has, in some countries (including Switzerland) been licensed as an emulsifier in food industry,[3] but it is no longer common. Outside the body it is used in experimental basis of cholagogues and is also in use to prevent and dissolve gallstones.[4][5]
In research deoxycholic acid is used as a mild detergent for the isolation of membrane associated proteins. The critical micelle concentration for deoxycholic acid is approximately 2.4-4 mM.[6]
Sodium deoxycholate, the sodium salt of deoxycholic acid, is often used as a biological detergent to lyse cells and solubilise cellular and membrane components.[7] Sodium deoxycholate mixed with phosphatidylcholine, is used in mesotherapy injections to produce lipolysis, and has been used as an alternative to surgical excision in the treatment of lipomas.[8]
Deoxycholates and bile acid derivatives in general are actively being studied as structures for incorporation in nanotechnology.[9] They also have found application in microlithography as photoresistant components.[10][11]
In the United States, deoxycholic acid, under the trade name Kybella, is approved by the Food and Drug Administration for reducing moderate-to-severe fat below the chin.[12] When injected into submental fat, deoxycholic acid helps destroy fat cells.[12]
Research in immunology
Its function as a detergent and isolating agent for membrane proteins also suits it for production of outer membrane protein (OMP) vaccines such as MenB, a Norwegian vaccine developed in the early 1990s.[13] The MeNZB vaccine was produced using the same method.[14]
Deoxycholic acid is one of the main components of the traditional Chinese medicine "Niuhuang", which means "Oxen Yellow" and is bilestone of oxen. This has been in use for two millennia in the unproven belief that it treats inflammations and enhances the immune system.[15]
Some publications point towards the effect of deoxycholic acid as an immunostimulant[16][17] of the non-specific immune system, activating its main actors, the macrophages. According to these publications, a sufficient amount of deoxycholic acid in the human body would correspond with a good immune reaction of the non-specific immune system. Clinical studies conducted in the 1970s and 1980s confirm the expectation, that deoxycholic acid is involved in the natural healing processes of local inflammations,[18][19] different types of herpes,[20][21] and possibly cancer.[22][23] Due to the same acronym, DCA, as another potential cancer treatment, deoxycholic acid is often confused with dichloroacetic acid.
Research in cancer
_and_with_tumorigenesis_(B)._Brown_shows_8-oxo-dG.jpg)
Deoxycholate and other secondary bile acids cause DNA damage.[25] Secondary bile acids increase intracellular production of reactive oxygen and reactive nitrogen species resulting in increased oxidative stress and DNA damage.[26][27] As shown in the figure in this section, deoxycholate added to the diet of mice increased the level of 8-oxo-dG, an oxidative DNA damage, in the colonic epithelium of mice. When the level of deoxycholate-induced DNA damage is high, DNA repair enzymes that ordinarily reverse DNA damage may not be able to keep up.
DNA damage has frequently been proposed as a major cause of cancer.[28][29][30] DNA damage can give rise to cancer by causing mutations.
When deoxycholate was added to the food of mice so that their feces contained deoxycholate at about the same level present in feces of human on a high fat diet, 45% to 56% of the mice developed colon cancer over the next 10 months.[24][31] Thus, exposure of the colon to deoxycholate can cause cancer.
In humans, higher levels of colonic deoxycholate are associated with higher frequencies of colon cancer. As an example, the fecal deoxycholate concentrations in African Americans (who eat a relatively high fat diet) is more than five times higher than fecal deoxycholate of Native Africans in South Africa (who eat a low fat diet).[32] Male African Americans have a high incidence of colon cancer of 72 per 100,000,[33] while Native Africans in South Africa have a low incidence rate of colon cancer of less than 1 per 100,000,[34] a more than 72-fold difference in rates of colon cancer.
Factors affecting deoxycholate levels
A number of factors, including diet, obesity, and exercise, affect the level of deoxycholate in the human colon. When humans were switched from their usual diet to a meat, egg and cheese based diet for five days, deoxycholate in their feces increased by factors of 2 to 10 fold.[35] Rats, fed diets with either 30% beef tallow (high fat) or 5% beef tallow (low fat) had almost 2-fold more deoxycholate in their feces on the high fat compared to the low fat diet.[36] In this study,[36] adding the further dietary elements of curcumin or caffeic acid to the rats' high fat (30% beef tallow) diet reduced the deoxycholate in their feces to levels comparable to levels seen in the rats on a low fat diet. Curcumin is a component of the spice turmeric, and caffeic acid is a component high in some fruits and spices.[37] Caffeic acid is also a digestive break-down product of chlorogenic acid, high in coffee and some fruits and vegetables.[38]
In addition to fats, the type or amount of protein in the diet may also affect bile acid levels. Switching from a diet with protein provided by casein to a diet with protein provided by salmon protein hydrolysate led to as much as a 6-fold increase in levels of bile acids in the blood plasma of rats.[39] In humans, adding high protein to a high fat diet raised the level of deoxycholate in the plasma by almost 50%.[40]
Obesity has been linked to cancer,[41] and this link is in part through deoxycholate.[42][43][44] In obese people, the relative proportion of Firmicutes (Gram-positive bacteria) in gut microbiota is increased resulting in greater conversion of the non-genotoxic primary bile acid, cholic acid, to carcinogenic deoxycholate.[42]
Exercise decreases deoxycholate in the colon. Humans whose level of physical activity placed them in the top third had a 17% decrease in fecal bile acid concentration compared to those whose level of physical activity placed them in the lowest third.[45] Rats provided with an exercise wheel had a lower ratio of secondary bile acids to primary bile acids than sedentary rats in their feces.[46] There is a positive association of exercise and physical activity with cancer prevention, tolerance to cancer-directed therapies (radiation and chemotherapy), reduction in recurrence, and improvement in survival.[47]
See also
- Ursodiol (ursodeoxycholic acid)
- Bile acids
References
- ↑ Product information sheet from Sigma Aldrich: http://www.sigmaaldrich.com/etc/medialib/docs/Sigma/Product_Information_Sheet/d2510pis.Par.0001.File.tmp/d2510pis.pdf
- ↑ Lide, David R. (1998). Handbook of Chemistry and Physics (87 ed.). Boca Raton, FL: CRC Press. p. 1287. ISBN 0-8493-0594-2
- ↑ Streuli, H. et al.: SLMB - Schweizer Lebensmittelbuch, 1992, chapter 58, 4/3
- ↑ Combichole, Trout Medical Inc., Houston, US
- ↑ Cholecysmon, Riemser Arzneimittel AG, Riems, Germany
- ↑ J.M. Neugebauer, Detergents: An Overview, in: M.P. Deutscher, Guide to Protein Purification (Methods in Enzymology Vol. 182), Academic Press, San Diego 1990
- ↑ Sodium deoxycholate
- ↑ Duncan D, Rotunda AM (2011). "Injectable therapies for localized fat loss: state of the art". Clin Plast Surg 38 (3): 489–501, vii. doi:10.1016/j.cps.2011.02.005. PMID 21824545.
- ↑ Molecules, 2001, 6, 21.
- ↑ Polym. Mat. Sci. Eng., 1997, 77, 445.
- ↑ Chemistry Letters, 2000, 414.
- 1 2 "FDA approves treatment for fat below the chin". Food and Drug Administration. April 29, 2015.
- ↑ Fredriksen JH, Rosenqvist E, Wedege E; et al. (December 1991). "Production, characterization and control of MenB-vaccine "Folkehelsa": an outer membrane vesicle vaccine against group B meningococcal disease". NIPH Ann 14 (2): 67–79; discussion 79–80. PMID 1812438.
- ↑ e.g., see PR from NZ immunology group, http://www.scoop.co.nz/stories/GE0506/S00048.htm
- ↑ Chen, Xin; Mellon, Richard Daniel; Yang, Lu; Dong, Huifang; Oppenheim, Joost J; Howard, Ola Mae Zack (February 2002). "Regulatory effects of deoxycholic acid, a component of the anti-inflammatory traditional Chinese medicine Niuhuang, on human leukocyte response to chemoattractants". Biochemical Pharmacology 63 (3): 533–541. doi:10.1016/S0006-2952(01)00917-0. PMID 11853704.
- ↑ Vlček B.: Potentiation of the immune response with DCA (Czech), Prakt.Lekar 52, 326-330 (1972)
- ↑ Chyle M., Chyle P.: Regulation of the immune response with DCA (Czech, engl. summary), Sbornik lek. 84, 212-218 (1982)
- ↑ Vlček B.: Deoxycholic acid as a potential cancerostatic and antiviral factor, Advances in Antimicrobial and Antineoplastic Chemotherapy, Vol. II/1, p.145-147 (Urban & Schwarzenberg, München 1972
- ↑ Chyle M., Chyle P., Dolezal V. (Inst. f. hygiene and epidemiology, Prag): Deoxycholic acid – Therapy of viral infections and a toxicological inquiry 2nd Symp. on Prevention and Treatment of Viral Infections, Bechyne Castle 1988, p. 56f.
- ↑ Chyle M. (Universität Prag), Chyle P.: Deoxycholic acid in therapy of herpes labialis (Czech, engl. summary), Cas. Lek. ces. 114, 1226–1229 (1975)
- ↑ Bradna J. (Poliklinik, Kutna Hora): Treatment of herpes zoster with deoxycholic acid (Czech, engl. summary), Rehabilitacia (Bratislava) 16, 77-86 (1983)
- ↑ Vlček B., Reif A., Budsky F. (Inst. f. Strahlenhygiene, Prag): Toxicity of deoxycholate at pH below 7,3 as a potential cancerostatic property, Experientia 26, 776-778 (1970)
- ↑ Vlček B., Reif A., Seidlova B.: Evidence of the participation of deoxycholate in cancer immunity, Z.Naturforsch. 26 b, 419-424 (1971)
- 1 2 Prasad AR, Prasad S, Nguyen H, Facista A, Lewis C, Zaitlin B, Bernstein H, Bernstein C (2014). "Novel diet-related mouse model of colon cancer parallels human colon cancer". World J Gastrointest Oncol 6 (7): 225–43. doi:10.4251/wjgo.v6.i7.225. PMC 4092339. PMID 25024814.
- ↑ Bernstein H, Bernstein C, Payne CM, Dvorakova K, Garewal H. Bile acids as carcinogens in human gastrointestinal cancers. Mutat Res. 2005 Jan;589(1):47-65. Review. PMID 15652226
- ↑ Tsuei J, Chau T, Mills D, Wan YJ. Bile acid dysregulation, gut dysbiosis, and gastrointestinal cancer. Exp Biol Med (Maywood). 2014 Nov;239(11):1489-504. doi: 10.1177/1535370214538743. PMID 24951470
- ↑ Ajouz H, Mukherji D, Shamseddine A. Secondary bile acids: an underrecognized cause of colon cancer. World J Surg Oncol. 2014 May 24;12:164. doi: 10.1186/1477-7819-12-164. Review. PMID 24884764
- ↑ Ames BN (1979). "Identifying environmental chemicals causing mutations and cancer". Science 204 (4393): 587–93. doi:10.1126/science.373122. PMID 373122.
- ↑ Tudek B, Winczura A, Janik J, Siomek A, Foksinski M, Oliński R. Involvement of oxidatively damaged DNA and repair in cancer development and aging. Am J Transl Res. 2010 May 15;2(3):254-84. PMID 20589166
- ↑ Bernstein C, Prasad AR, Nfonsam V, Bernstein H. (2013). DNA Damage, DNA Repair and Cancer, New Research Directions in DNA Repair, Prof. Clark Chen (Ed.), ISBN 978-953-51-1114-6, InTech, http://www.intechopen.com/books/new-research-directions-in-dna-repair/dna-damage-dna-repair-and-cancer
- ↑ Bernstein C, Holubec H, Bhattacharyya AK, Nguyen H, Payne CM, Zaitlin B, Bernstein H. (2011). Carcinogenicity of deoxycholate, a secondary bile acid. Arch Toxicol 85(8):863-71. doi: 10.1007/s00204-011-0648-7. PMID 21267546 http://www.ncbi.nlm.nih.gov/pubmed/?term=Bernstein+C%2C+Holubec+H%2C+Bhattacharyya+AK%2C+Nguyen+H
- ↑ Ou J, DeLany JP, Zhang M, Sharma S, O'Keefe SJ (2012). "Association between low colonic short-chain fatty acids and high bile acids in high colon cancer risk populations". Nutr Cancer 64 (1): 34–40. doi:10.1080/01635581.2012.630164. PMID 22136517.
- ↑ American Cancer Society. Cancer Facts and Figures 2009. http://www.cancer.org/Research/CancerFactsFigures/cancer-facts-figures-2009
- ↑ O'Keefe SJ, Kidd M, Espitalier-Noel G, Owira P (May 1999). "Rarity of colon cancer in Africans is associated with low animal product consumption, not fiber". Am. J. Gastroenterol. 94 (5): 1373–80. doi:10.1111/j.1572-0241.1999.01089.x. PMID 10235221.
- ↑ David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA, Biddinger SB, Dutton RJ, Turnbaugh PJ. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014 Jan 23;505(7484):559-63. doi: 10.1038/nature12820. PMID 24336217
- 1 2 Han Y, Haraguchi T, Iwanaga S, Tomotake H, Okazaki Y, Mineo S, Moriyama A, Inoue J, Kato N. Consumption of some polyphenols reduces fecal deoxycholic acid and lithocholic acid, the secondary bile acids of risk factors of colon cancer. J Agric Food Chem. 2009 Sep 23;57(18):8587-90. doi: 10.1021/jf900393k. PMID 19711910
- ↑ http://phenol-explorer.eu/contents/polyphenol/457
- ↑ Clifford M. (1999) Chlorogenic acids and other cinnamates—nature, occurrence and dietary burden. J. Sci. Food Agric., 79, 362–372.
- ↑ Liaset B, Hao Q, Jørgensen H, Hallenborg P, Du ZY, Ma T, Marschall HU, Kruhøffer M, Li R, Li Q, Yde CC, Criales G, Bertram HC, Mellgren G, Ofjord ES, Lock EJ, Espe M, Frøyland L, Madsen L, Kristiansen K. Nutritional regulation of bile acid metabolism is associated with improved pathological characteristics of the metabolic syndrome. J Biol Chem. 2011 Aug 12;286(32):28382-95. doi: 10.1074/jbc.M111.234732. PMID 21680746
- ↑ Bortolotti M, Kreis R, Debard C, Cariou B, Faeh D, Chetiveaux M, Ith M, Vermathen P, Stefanoni N, Lê KA, Schneiter P, Krempf M, Vidal H, Boesch C, Tappy L (2009). "High protein intake reduces intrahepatocellular lipid deposition in humans". Am. J. Clin. Nutr. 90 (4): 1002–10. doi:10.3945/ajcn.2008.27296. PMID 19710199.
- ↑ Ungefroren H, Gieseler F, Fliedner S, Lehnert H. Obesity and cancer. Horm Mol Biol Clin Investig. 2015 Jan 1;21(1):5-15. doi: 10.1515/hmbci-2014-0046. PMID 25719336
- 1 2 Bradlow HL. Obesity and the gut microbiome: pathophysiological aspects. Horm Mol Biol Clin Investig. 2014 Jan;17(1):53-61. doi: 10.1515/hmbci-2013-0063. PMID 25372730
- ↑ Devkota S, Turnbaugh PJ. Cancer: An acidic link. Nature. 2013 Jul 4;499(7456):37-8. doi: 10.1038/nature12404. PMID 23803768
- ↑ Ohtani N, Yoshimoto S, Hara E. Obesity and cancer: a gut microbial connection. Cancer Res. 2014 Apr 1;74(7):1885-9. doi: 10.1158/0008-5472.CAN-13-3501. Review. PMID 24638983
- ↑ Wertheim BC, Martínez ME, Ashbeck EL, Roe DJ, Jacobs ET, Alberts DS, Thompson PA. Physical activity as a determinant of fecal bile acid levels. Cancer Epidemiol Biomarkers Prev. 2009 May;18(5):1591-8. doi: 10.1158/1055-9965.EPI-08-1187. PMID 19383885
- ↑ Hagio M, Matsumoto M, Yajima T, Hara H, Ishizuka S. Voluntary wheel running exercise and dietary lactose concomitantly reduce proportion of secondary bile acids in rat feces. J Appl Physiol (1985). 2010 Sep;109(3):663-8. doi: 10.1152/japplphysiol.00777.2009. PMID 20616226
- ↑ Jeon JY, Meyerhardt JA. Exercise after cancer diagnosis: time to get moving. Oncology (Williston Park). 2013 Jun;27(6):585-6, 588. PMID 23909074
|