Computed tomography of the heart
| Computed tomography of the heart | |
|---|---|
| Intervention | |
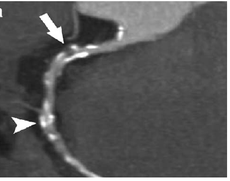 Image of contrast enhanced dual-source coronary CT-angiograph | |
| ICD-9-CM | 87.41 |
| OPS-301 code | 3-224 |
Computed tomography or CT scanning of the heart (CT coronary angiogram) is a procedure used to assess the extent of occlusion in the coronary arteries, usually in order to diagnose coronary artery disease. The patient is injected with an intravenous dye (iodine) and then their heart is scanned using a high speed CT scanner, allowing radiologists to assess the blood flow to their heart muscle.
Medical uses
Computed tomography of the heart is not yet routinely used in clinical practice. It may be useful in the diagnosis of suspected coronary heart disease, for follow-up of a coronary artery bypass, for the evaluation of valvular heart disease and for the evaluation of cardiac masses.
It is uncertain whether this modality will replace invasive coronary catheterization. At present, it appears that the greatest utility of cardiac CT lies in ruling out coronary artery disease rather than ruling it in. This is because the test is highly sensitive (over 90% detection rate), so a negative test result largely rules out coronary artery disease (i.e. the test has a high negative predictive value).[1] The test is not very specific, however, so a positive result is less conclusive and will need to be confirmed by subsequent invasive angiography.
The positive predictive value of cardiac CTA is approximately 82% and the negative predictive value is around 93%. This means for every 100 patients who appear to have coronary artery disease after CT angiography, 18 of them actually won't have it, and that for every 100 patients who have a negative CT angio test result (i.e. the test says they do not have coronary artery disease), 7 will actually have the disease.
In addition to the diagnostic abilities, cardiac CTA beholds important prognostic information. Stenosis severity and extent of coronary artery disease are important prognostic indicators.[2] However, one of the unique features of cardiac CTA is the fact that it enables the visualization of the vessel wall, in a non-invasive manner. Therefore, the technique is able to identify characteristics of coronary artery disease that are associated to the development of acute coronary syndrome.[3][4]
CTA is superior than Coronary Artery Calcium Score (CACS) in Major Adverse Cardiac Events (MACE).[5]
Side effects
Because the heart is effectively imaged more than once (described above), cardiac CT angiography can result in a relatively high radiation exposure (around 12 millisievert), although newer acquisition protocols, have recently been developed which drastically reduce this exposure to around 1 mSv (cfr. Pavone, Fioranelli, Dowe: Computed Tomography or Coronary Arteries, Springer 2009). By comparison, a chest X-ray carries a dose of approximately 0.02-0.2 mSv[6] and natural background radiation exposure is around 0.01 mSv/d. Thus, each cardiac CT scan carried out is equivalent to approximately 100-600 chest X-rays or over 3 years of background radiation. Methods are available to decrease this exposure; however, such as prospectively decreasing radiation output based on the concurrently acquired ECG (i.e. tube current modulation.) This can result in a significant decrease in radiation exposure, at the risk of compromising image quality if there is any arrhythmia during the acquisition.
The significance of radiation doses in the diagnostic imaging range has not been proven, although the possibility of inducing an increased cancer risk across a population is a source of significant concern. This potential risk must be weighed against the competing risk of not performing a test and potentially not diagnosing a significant health problem such as coronary artery disease.
Contraindications
Pregnancy is considered an absolute contraindication. Since an iodine-containing contrast agent is used, contrast agent allergy, hyperthyroidism or renal function impairment are relative contraindications. Cardiac arrhythmias, coronary artery stents and tachycardia may result in a reduced image quality.
Improved resolution
With the advent of subsecond rotation combined with multi-slice CT (up to 320 slices), high resolution and high speed can be obtained at the same time, allowing excellent imaging of the coronary arteries (cardiac CT angiography). Images with an even higher temporal resolution can be formed using retrospective ECG gating. In this technique, each portion of the heart is imaged more than once while an ECG trace is recorded. The ECG is then used to correlate the CT data with their corresponding phases of cardiac contraction. Once this correlation is complete, all data that were recorded while the heart was in motion (systole) can be ignored and images can be made from the remaining data that happened to be acquired while the heart was at rest (diastole). In this way, individual frames in a cardiac CT investigation have a better temporal resolution than the shortest tube rotation time.
Dual Source CT scanners, introduced in 2005, allow higher temporal resolution by acquiring a full CT slice in only half a rotation, thus reducing motion blurring at high heart rates and potentially allowing for shorter breath-hold time. This is particularly useful for ill patients having difficulty holding their breath or unable to take heart-rate lowering medication.
The speed advantages of 64-slice MSCT have rapidly established it as the minimum standard for newly installed CT scanners intended for cardiac scanning. Manufacturers have developed 320-slice and true 'volumetric' scanners, primarily for their improved cardiac scanning performance.
Introduction of a CT scanner with a 160 mm detector in 2014 allows for imaging of the whole heart in a single beat without motion of the coronary arteries, regardless of patient hear rate.
The latest MSCT scanners acquire images only at 70-80% of the R-R interval (late diastole). This prospective gating can reduce effective dose from 10-15 mSv to as little as 1.2 mSv in follow-up patients acquiring at 75% of the R-R interval. Effective dose using MSCT coronary imaging can average less than the dose in conventional coronary angiography.
References
- ↑ Mikolich, JR (May 2012). "Cardiac computed tomographic angiography and the primary care physician.". The Journal of the American Osteopathic Association 112 (5): 267–275. PMID 22582196.
- ↑ Min JK et al. Age- and Sex-Related Differences in All-Cause Mortality Risk Based on Coronary Computed Tomography Angiography Findings. J Am Coll Cardiol. 2011 Aug 16;58(8):849-60. doi: 10.1016/j.jacc.2011.02.074.
- ↑ Motoyama S. et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009 Jun 30;54(1):49-57. doi: 10.1016/j.jacc.2009.02.068.
- ↑ Versteylen MO, et al. Additive value of semi-automated quantification of coronary artery disease using cardiac CT-angiography to predict for future acute coronary syndrome. J Am Coll Cardiol. 2013;():. doi:10.1016/j.jacc.2013.02.065
- ↑ Zhi-hui Hou, MD; Bin Lu, MD; Yang Gao, MD; Shi-liang Jiang, MD; Yang Wang, MD; Wei Li, MD; Matthew J. Budoff, MD. "Prognostic Value of Coronary CT Angiography and Calcium Score for Major Adverse Cardiac Events in Outpatients". Retrieved April 9, 2015.
- ↑ Hart, D; Wall B F (2002). "Radiation exposure of the UK population from Medical and Dental X-ray examinations". NRPB report W-4. Retrieved December 30, 2013.
| ||||||||||||||||||||||||||||