Coenzyme Q10
 | |
| Names | |
|---|---|
| IUPAC name
2-[(2E,6E,10E,14E,18E,22E,26E,30E,34E)-3,7,11,15,19,23,27,31,35,39-Decamethyltetraconta-2,6,10,14,18,22,26,30,34,38-decaenyl]-5,6-dimethoxy-3-methylcyclohexa-2,5-diene-1,4-dione | |
| Identifiers | |
| 303-98-0 | |
| ChEBI | CHEBI:46245 |
| ChEMBL | ChEMBL454801 |
| ChemSpider | 4445197 |
| Jmol interactive 3D | Image |
| PubChem | 5281915 |
| UNII | EJ27X76M46 |
| |
| |
| Properties | |
| C59H90O4 | |
| Molar mass | 863.37 g·mol−1 |
| Appearance | yellow or orange solid |
| Melting point | 48–52 °C (118–126 °F; 321–325 K) |
| insoluble | |
| Pharmacology | |
| ATC code | C01 |
| Related compounds | |
| Related quinones |
1,4-Benzoquinone Plastoquinone Ubiquinol |
| Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| | |
| Infobox references | |
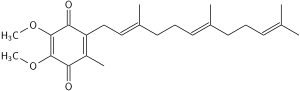
Coenzyme Q10, also known as ubiquinone, ubidecarenone, coenzyme Q, and abbreviated at times to CoQ10 /ˌkoʊ ˌkjuː ˈtɛn/, CoQ, or Q10 is a coenzyme that is ubiquitous in the bodies of most animals. It is a 1,4-benzoquinone, where Q refers to the quinone chemical group and 10 refers to the number of isoprenyl chemical subunits in its tail.
This oil-soluble, vitamin-like substance is present in most eukaryotic cells, primarily in the mitochondria. It is a component of the electron transport chain and participates in aerobic cellular respiration, which generates energy in the form of ATP. Ninety-five percent of the human body’s energy is generated this way.[1][2] Therefore, those organs with the highest energy requirements—such as the heart, liver and kidney—have the highest CoQ10 concentrations.[3][4][5]
There are three redox states of CoQ10: fully oxidized (ubiquinone), semiquinone (ubisemiquinone), and fully reduced (ubiquinol). The capacity of this molecule to exist in a completely oxidized form and a completely reduced form enables it to perform its functions in the electron transport chain, and as an antioxidant, respectively.
Deficiency and toxicity
There are two major factors that lead to deficiency of CoQ10 in humans: reduced biosynthesis, and increased utilization by the body. Biosynthesis is the major source of CoQ10. Biosynthesis requires at least 12 genes, and mutations in many of them cause CoQ deficiency. CoQ10 levels can also be affected by other genetic defects (such as mutations of mitochondrial DNA, ETFDH, APTX, FXN, and BRAF, genes that are not directly related to the CoQ10 biosynthetic process) while the role of statins is controversial.[6] Some chronic disease conditions (cancer, heart disease, etc.) are also thought to reduce the biosynthesis and increase the demand for CoQ10 in the body, but there are no definite data to support these claims.
Toxicity is not usually observed with high doses of CoQ10. A daily dosage up to 3600 mg was found to be tolerated by healthy as well as unhealthy persons.[7] However, some adverse effects, largely gastrointestinal, are reported with very high intakes. The observed safe level (OSL) risk assessment method indicated that the evidence of safety is strong at intakes up to 1200 mg/day, and this level is identified as the OSL.[8]
Clinical assessment
Although CoQ10 can be measured in plasma, these measurements reflect dietary intake rather than tissue status. Currently, most clinical centers measure CoQ10 levels in cultured skin fibroblasts, muscle biopsies, and blood mononuclear cells.[6] Culture fibroblasts can be used also to evaluate the rate of endogenous CoQ10 biosynthesis, by measuring the uptake of 14C-labelled p-hydroxybenzoate.[9]
Inhibition by statins and beta blockers
CoQ10 shares a biosynthetic pathway with cholesterol. The synthesis of an intermediary precursor of CoQ10, mevalonate, is inhibited by some beta blockers, blood pressure-lowering medication,[10] and statins, a class of cholesterol-lowering drugs.[11] Statins can reduce serum levels of CoQ10 by up to 40%.[12]
Supplementation
CoQ10 is not approved by the US Food and Drug Administration (FDA) for the treatment of any medical condition.[13] It is sold as a dietary supplement. In the US, supplements are not regulated as drugs but as foods. How CoQ10 is manufactured is not regulated and different batches and brands may vary significantly.[13]
A 2004 laboratory analysis by ConsumerLab.com found CoQ10 supplements on the market did not all contain the quantity identified on the product label. Amounts varied from "no detectable CoQ10" to 75% of stated dose up to a 75% excess.[14]
CoQ10 is generally well tolerated. The most common side effects are gastrointestinal symptoms (nausea, vomiting, appetite suppression and stomachache), rash and headache.[15]
Heart disease
A 2014 Cochrane Collaboration meta-analysis found "no convincing evidence to support or refute" the use of CoQ10 for the treatment of heart failure.[16] Evidence with respect to preventing heart disease in those who are otherwise healthy is also poor.[17]
A 2009 Cochrane review concluded that studies looking at the effects of CoQ10 on blood pressure were unreliable, and therefore no conclusions could be made regarding its effectiveness in lowering blood pressure.[18]
Huntington's disease
Available evidence suggests that "CoQ10 is likely ineffective in moderately improving" the chorea associated with Huntington's disease.[19]
Male infertility
While CoQ10 can improve some measurements regarding sperm quality, there is no evidence that CoQ10 increases live births or pregnancy rates.[20]
Migraine headaches
Supplementation of CoQ10 has been found to have a beneficial effect on the condition of some sufferers of migraine. This is based on the theory that migraines are a mitochondrial disorder,[21] and that mitochondrial dysfunction can be improved with CoQ10.[22] The Canadian Headache Society guideline for migraine prophylaxis recommends, based on low-quality evidence, that 300 mg of CoQ10 be offered as a choice for prophylaxis.[23]
Statin myopathy
CoQ10 has been routinely used to treat muscle breakdown associated as a side effect of use of statin medications. However, evidence from randomized controlled trials does not appear to support the idea that CoQ10 is an effective treatment for statin myopathy.[24]
Cancer
No large well-designed clinical trials of CoQ10 in cancer treatment have been done.[13] The National Cancer Institute identified issues with the few, small studies that have been done stating, "the way the studies were done and the amount of information reported made it unclear if benefits were caused by the CoQ10 or by something else".[13] The American Cancer Society has concluded, "CoQ10 may reduce the effectiveness of chemo and radiation therapy, so most oncologists would recommend avoiding it during cancer treatment."[25]
Dental disease
A review study has shown that there is no clinical benefit to the use of CoQ10 in the treatment of periodontal disease.[26] Most of the studies suggesting otherwise were outdated, focused on in-vitro tests,[27][28][29] had too few test subjects and/or erroneous statistical methodology and trial set-up,[30][31] or were sponsored by a manufacturer of the product.[32]
Parkinson's disease
A 2011 review by the Cochrane Collaboration suggesting CoQ10 supplementation might benefit people with Parkinson's disease was subsequently withdrawn from publication following a review by independent editors.[33]
Drug interactions
Coenzyme Q10 has potential to inhibit the effects of warfarin (Coumadin), a potent anticoagulant, by reducing the INR. The structure of coenzyme Q10 is very much similar to the structure of vitamin K, which competes with and counteracts warfarin's anticoagulation effects. Coenzyme Q10 should be avoided in patients currently taking warfarin due to the increased risk of clotting.[15]
Chemical properties
The oxidized structure of CoQ10 is shown on the top-right. The various kinds of Coenzyme Q can be distinguished by the number of isoprenoid subunits in their side-chains. The most common Coenzyme Q in human mitochondria is CoQ10. Q refers to the quinone head and 10 refers to the number of isoprene repeats in the tail. The image below has three isoprenoid units and would be called Q3.
Biochemical role
CoQ10 is found in the membranes of many organelles. Since its primary function in cells is in generating energy, the highest concentration is found on the inner membrane of the mitochondrion. Some other organelles that contain CoQ10 include endoplasmic reticulum, peroxisomes, lysosomes, and vesicles.
CoQ10 and electron transport chain
CoQ10 is fat-soluble and is therefore mobile in cellular membranes; it plays a unique role in the electron transport chain (ETC). In the inner mitochondrial membrane, electrons from NADH and succinate pass through the ETC to oxygen, which is reduced to water. The transfer of electrons through ETC results in the pumping of H+ across the membrane creating a proton gradient across the membrane, which is used by ATP synthase (located on the membrane) to generate ATP. CoQ10 functions as an electron carrier from enzyme complex I and enzyme complex II to complex III in this process. This is crucial in the process, since no other molecule can perform this function (Note: recent research now establishes that Vitamin K2 co-performs this role with CoQ10[34]). Thus, CoQ10 functions in every cell of the body to synthesize energy.
Antioxidant (reductant) function of CoQ10
The antioxidant nature of CoQ10 derives from its energy carrier function. As an energy carrier, the CoQ10 molecule continuously goes through an oxidation–reduction cycle. As it accepts electrons, it becomes reduced. As it gives up electrons, it becomes oxidized. In its reduced form, the CoQ10 molecule holds electrons rather loosely, so this CoQ molecule will quite easily give up one or both electrons and, thus, act as an antioxidant.[35] CoQ10 inhibits lipid peroxidation by preventing the production of lipid peroxyl radicals (LOO). Moreover, CoQH2 reduces the initial perferryl radical and singlet oxygen, with concomitant formation of ubisemiquinone and H2O2. This quenching of the initiating perferryl radicals, which prevent propagation of lipid peroxidation, protects not only lipids but also proteins from oxidation. In addition, the reduced form of CoQ effectively regenerates vitamin E from the a-tocopheroxyl radical, thereby interfering with the propagation step. Furthermore, during oxidative stress, interaction of H2O2 with metal ions bound to DNA generates hydroxyl radicals, and CoQ efficiently prevents the oxidation of bases, in particular, in mitochondrial DNA.[35] In contrast to other antioxidants, this compound inhibits both the initiation and the propagation of lipid and protein oxidation. It also regenerates other antioxidants such as vitamin E. The circulating CoQ10 in LDL prevents oxidation of LDL, which may provide benefit in cardiovascular diseases.
Biosynthesis
Biosynthesis occurs in most human tissue. There are three major steps:
- Creation of the benzoquinone structure (using phenylalanine or tyrosine)
- Creation of the isoprene side chain (using acetyl-CoA)
- The joining or condensation of the above two structures
The initial two reactions occur in mitochondria, endoplasmic reticulum and peroxisomes, indicating multiple sites of synthesis in animal cells.[36]
An important enzyme in this pathway is HMG-CoA reductase, usually a target for intervention in cardiovascular complications. The "statin" family of cholesterol-reducing medications inhibits HMG-CoA reductase. One side effect of statins is decreased production of CoQ-10, which leads to myopathy and rhabdomyolysis.
Genes involved include PDSS1, PDSS2, COQ2, and ADCK3(COQ8,CABC1).[37]
Increasing the endogenous biosynthesis of CoQ10 has gained attention in recent years as a strategy to fight CoQ10 deficiency.
Absorption and metabolism
Absorption
CoQ10 is a crystalline powder insoluble in water. Absorption follows the same process as that of lipids; the uptake mechanism appears to be similar to that of vitamin E, another lipid-soluble nutrient. This process in the human body involves secretion into the small intestines of pancreatic enzymes and bile, which facilitate emulsification and micelle formation required for absorption of lipophilic substances.[38] Food intake (and the presence of lipids) stimulates bodily biliary excretion of bile acids and greatly enhances absorption of CoQ10. Exogenous CoQ10 is absorbed from the small intestine and is best absorbed if taken with a meal. Serum concentration of CoQ10 in fed condition is higher than in fasting conditions.[39][40]
Metabolism
Data on the metabolism of CoQ10 in animals and humans are limited.[41] A study with 14C-labeled CoQ10 in rats showed most of the radioactivity in the liver 2 hours after oral administration when the peak plasma radioactivity was observed, but it should be noted that CoQ9 (with only 9 isoprenyl units) is the predominant form of coenzyme Q in rats.[42] It appears that CoQ10 is metabolised in all tissues, while a major route for its elimination is biliary and fecal excretion. After the withdrawal of CoQ10 supplementation, the levels return to normal within a few days, irrespective of the type of formulation used.[43]
Pharmacokinetics
Some reports have been published on the pharmacokinetics of CoQ10. The plasma peak can be observed 2–6 hours after oral administration, depending mainly on the design of the study. In some studies, a second plasma peak was also observed at about 24 hours after administration, probably due to both enterohepatic recycling and redistribution from the liver to circulation.[38] Tomono et al. used deuterium-labelled crystalline CoQ10 to investigate pharmacokinetics in humans and determined an elimination half-time of 33 hours.[44]
Improving the bioavailability of CoQ10
The importance of how drugs are formulated for bioavailability is well-known. In order to find a principle to boost the bioavailability of CoQ10 after oral administration, several new approaches have been taken; different formulations and forms have been developed and tested on animals and humans.[41]
Reduction of particle size
An obvious strategy is reduction of particle size to as low as the micro- and nano-scale. Nanoparticles have been explored as a delivery system for various drugs; an improvement of the oral bioavailability of drugs with poor absorption characteristics has been reported;[45] pathways of absorption and efficiency were affected by reduction of particle size. This protocol has so far not proved to be very successful with CoQ10, although reports have differed widely.[46][47] The use of aqueous suspension of finely powdered CoQ10 in pure water also reveals only a minor effect.[43]
Soft-gel capsules with CoQ10 in oil suspension
A successful approach was to use the emulsion system to facilitate absorption from the gastrointestinal tract and to improve bioavailability. Emulsions of soybean oil (lipid microspheres) could be stabilised very effectively by lecithin and were utilised in the preparation of soft gelatine capsules. In one of the first such attempts, Ozawa et al. performed a pharmacokinetic study on beagle dogs in which the emulsion of CoQ10 in soybean oil was investigated; about two times higher plasma CoQ10 level than that of the control tablet preparation was determined during administration of a lipid microsphere.[43] Although an almost negligible improvement of bioavailability was observed by Kommuru et al. with oil-based soft-gel capsules in a later study on dogs,[48] the significantly increased bioavailability of CoQ10 was confirmed for several oil-based formulations in most other studies.[49]
Novel forms of CoQ10 with increased water-solubility
Facilitating drug absorption by increasing its solubility in water is a common pharmaceutical strategy and has also been shown to be successful for CoQ10. Various approaches have been developed to achieve this goal, with many of them producing significantly better results over oil-based soft-gel capsules in spite of the many attempts to optimize their composition.[41] Examples of such approaches are use of the aqueous dispersion of solid CoQ10 with tyloxapol polymer,[50] formulations based on various solubilising agents, i.e., hydrogenated lecithin,[51] and complexation with cyclodextrins; among the latter, complex with β-cyclodextrin has been found to have highly increased bioavailability.[52][53] and is also used in pharmaceutical and food industries for CoQ10-fortification.[41] Also some other novel carrier systems like liposomes, nanoparticles, dendrimers, etc. can be used to increase the bioavailability of CoQ10.
History
CoQ10 was first discovered by Professor Fredrick L. Crane and colleagues at the University of Wisconsin–Madison Enzyme Institute in 1957.[54][55] In 1958, its chemical structure was reported by Dr. Karl Folkers and coworkers at Merck. In 1961 Peter Mitchell proposed the electron transport chain (which includes the vital protonmotive role of CoQ10) and he received a Nobel prize for the same in 1978. In 1972, Gian Paolo Littarru and Karl Folkers separately demonstrated a deficiency of CoQ10 in human heart disease. The 1980s witnessed a steep rise in the number of clinical trials due to the availability of large quantities of pure CoQ10 and methods to measure plasma and blood CoQ10 concentrations. The redox functions of CoQ in cellular energy production and antioxidant protection are based on the ability to exchange two electrons in a redox cycle between ubiquinol (reduced CoQ) and ubiquinone (oxidized CoQ).[56][57] The antioxidant role of the molecule as a free radical scavenger was widely studied by Lars Ernster. Numerous scientists around the globe started studies on this molecule since then in relation to various diseases including cardiovascular diseases and cancer.
Dietary concentrations
Detailed reviews on occurrence of CoQ10 and dietary intake were published in 2010.[58] Besides endogenous synthesis, CoQ10 is also supplied to the organism by various foods. However, despite the scientific community’s great interest in this compound, a very limited number of studies have been performed to determine the contents of CoQ10 in dietary components. The first reports on this issue were published in 1959, but the sensitivity and selectivity of the analytical methods at that time did not allow reliable analyses, especially for products with low concentrations.[58] Developments in analytical chemistry have since enabled a more reliable determination of CoQ10 concentrations in various foods (table below).
| Food | CoQ10 concentration [mg/kg] |
|---|---|
| Beef | |
| heart | 113 |
| liver | 39–50 |
| muscle | 26–40 |
| Pork | |
| heart | 11.8–128.2 |
| liver | 22.7–54.0 |
| muscle | 13.8–45.0 |
| Chicken | |
| heart | 116.2–132.2 |
| Fish | |
| sardine | 5–64 |
| mackerel | |
| red flesh | 43–67 |
| white flesh | 11–16 |
| salmon | 4–8 |
| tuna | 5 |
| Oils | |
| soybean | 54–280 |
| olive | 4–160 |
| grapeseed | 64–73 |
| sunflower | 4–15 |
| rice bran | / |
| coconut | |
| canola | 64-73 |
| Nuts | |
| peanuts | 27 |
| walnuts | 19 |
| sesame seeds | 18–23 |
| pistachio nuts | 20 |
| hazelnuts | 17 |
| almond | 5–14 |
| Vegetables | |
| parsley | 8–26 |
| broccoli | 6–9 |
| cauliflower | 2–7 |
| spinach | up to 10 |
| grape | 6–7 |
| Chinese cabbage | 2–5 |
| Fruit | |
| avocado | 10 |
| blackcurrant | 3 |
| strawberry | 1 |
| orange | 1–2 |
| grapefruit | 1 |
| apple | 1 |
| banana | 1 |
Meat and fish are the richest source of dietary CoQ10; levels over 50 mg/kg can be found in beef, pork, chicken heart and chicken liver. Dairy products are much poorer sources of CoQ10 compared to animal tissues. Vegetable oils are also quite rich in CoQ10. Within vegetables, parsley and perilla are the richest CoQ10 sources, but significant differences in their CoQ10 levels can be found in the literature. Broccoli, grape, and cauliflower are modest sources of CoQ10. Most fruit and berries represent a poor to very poor source of CoQ10, with the exception of avocado, with a relatively high CoQ10 content.[58]
Intake
In the developed world, the estimated daily intake of CoQ10 has been determined at 3–6 mg per day, derived primarily from meat.[58]
Effect of heat and processing
Cooking by frying reduces CoQ10 content by 14–32%.[59]
See also
- Idebenone – synthetic analog with reduced oxidant generating properties
References
- ↑ Ernster, L; Dallner, G (1995). "Biochemical, physiological and medical aspects of ubiquinone function". Biochimica et Biophysica Acta 1271 (1): 195–204. doi:10.1016/0925-4439(95)00028-3. PMID 7599208.
- ↑ Dutton, PL; Ohnishi, T; Darrouzet, E; Leonard, MA; Sharp, RE; Cibney, BR; Daldal, F; Moser, CC (2000). "4 Coenzyme Q oxidation reduction reactions in mitochondrial electron transport". In Kagan, VE; Quinn, PJ. Coenzyme Q: Molecular mechanisms in health and disease. Boca Raton: CRC Press. pp. 65–82.
- ↑ Okamoto, T; Matsuya, T; Fukunaga, Y; Kishi, T; Yamagami, T (1989). "Human serum ubiquinol-10 levels and relationship to serum lipids". International journal for vitamin and nutrition research. Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. Journal international de vitaminologie et de nutrition 59 (3): 288–92. PMID 2599795.
- ↑ Aberg, F; Appelkvist, EL; Dallner, G; Ernster, L (1992). "Distribution and redox state of ubiquinones in rat and human tissues". Archives of Biochemistry and Biophysics 295 (2): 230–4. doi:10.1016/0003-9861(92)90511-T. PMID 1586151.
- ↑ Shindo, Y; Witt, E; Han, D; Epstein, W; Packer, L (1994). "Enzymic and non-enzymic antioxidants in epidermis and dermis of human skin". The Journal of Investigative Dermatology 102 (1): 122–4. doi:10.1111/1523-1747.ep12371744. PMID 8288904.
- 1 2 Trevisson E, Dimauro S, Navas P, Salviati L (October 2011). "Coenzyme Q deficiency in muscle". Curr. Opin. Neurol. 24 (5): 449–56. doi:10.1097/WCO.0b013e32834ab528. PMID 21844807.
- ↑ Hyson HC, Kieburtz K, Shoulson I; et al. (September 2010). "Safety and tolerability of high-dosage coenzyme Q10 in Huntington's disease and healthy subjects". Mov. Disord. 25 (12): 1924–8. doi:10.1002/mds.22408. PMID 20669312.
- ↑ Hathcock JN, Shao A (August 2006). "Risk assessment for coenzyme Q10 (Ubiquinone)". Regul. Toxicol. Pharmacol. 45 (3): 282–8. doi:10.1016/j.yrtph.2006.05.006. PMID 16814438.
- ↑ Montero R, Sánchez-Alcázar JA, Briones P; et al. (June 2008). "Analysis of coenzyme Q10 in muscle and fibroblasts for the diagnosis of CoQ10 deficiency syndromes". Clin. Biochem. 41 (9): 697–700. doi:10.1016/j.clinbiochem.2008.03.007. PMID 18387363.
- ↑ Kishi, T; Watanabe, T; Folkers, K (1977). "Bioenergetics in clinical medicine XV. Inhibition of coenzyme Q10-enzymes by clinically used adrenergic blockers of beta-receptors". Research communications in chemical pathology and pharmacology 17 (1): 157–64. PMID 17892.
- ↑ Mortensen, SA; Leth, A; Agner, E; Rohde, M (1997). "Dose-related decrease of serum coenzyme Q10 during treatment with HMG-CoA reductase inhibitors". Molecular aspects of medicine 18 (Suppl): S137–44. doi:10.1016/S0098-2997(97)00014-9. PMID 9266515.
- ↑ Ghirlanda, G; Oradei, A; Manto, A; Lippa, S; Uccioli, L; Caputo, S; Greco, AV; Littarru, GP (1993). "Evidence of plasma CoQ10-lowering effect by HMG-CoA reductase inhibitors: a double-blind, placebo-controlled study". The Journal of Clinical Pharmacology 33 (3): 226–9. doi:10.1002/j.1552-4604.1993.tb03948.x. PMID 8463436.
- 1 2 3 4 White, J. (lead reviewer); National Cancer Institute (NCI) (14 May 2014). "PDQ® Coenzyme Q10". NCI, National Institutes of Health, US Dept. of Health and Human Services. Retrieved 29 June 2014.
- ↑ "ConsumerLab.com finds discrepancies in strength of CoQ10 supplements". Townsend Letter for Doctors and Patients. August–September 2004. p. 19.
- 1 2 Wyman M, Leonard M, Morledge T (July 2010). "Coenzyme Q10: a therapy for hypertension and statin-induced myalgia?". Cleve Clin J Med 77 (7): 435–42. doi:10.3949/ccjm.77a.09078. PMID 20601617.
- ↑ Madmani, M.E.; Yusuf Solaiman, A.; Tamr Agha, K.; Madmani, Y.; et al. (2 June 2014). "Coenzyme Q10 for heart failure". Heart Group. Cochrane Database of Systematic Reviews (John Wiley & Sons) (6): Art. no. CD008684. doi:10.1002/14651858.CD008684.pub2 – via The Cochrane Library. (subscription required (help)).
- ↑ Flowers, N; Hartley, L; Todkill, D; Stranges, S; Rees, K (4 December 2014). "Co-enzyme Q10 supplementation for the primary prevention of cardiovascular disease.". The Cochrane database of systematic reviews 12: CD010405. doi:10.1002/14651858.CD010405.pub2. PMID 25474484.
- ↑ Ho, MJ; Bellusci, A; Wright, JM (Oct 7, 2009). "Blood pressure lowering efficacy of coenzyme Q10 for primary hypertension.". The Cochrane database of systematic reviews (4): CD007435. doi:10.1002/14651858.CD007435.pub2. PMID 19821418.
- ↑ Armstrong, MJ; Miyasaki, JM (Aug 7, 2012). "Evidence-based guideline: pharmacologic treatment of chorea in Huntington disease: report of the guideline development subcommittee of the American Academy of Neurology.". Neurology (American Academy of Neurology) 79 (6): 597–603. doi:10.1212/wnl.0b013e318263c443. PMC 3413759. PMID 22815556.
- ↑ Lafuente, R; González-Comadrán, M; Solà, I; López, G; Brassesco, M; Carreras, R; Checa, MA (Sep 2013). "Coenzyme Q10 and male infertility: a meta-analysis.". Journal of assisted reproduction and genetics 30 (9): 1147–56. doi:10.1007/s10815-013-0047-5. PMID 23912751.
- ↑ Markley HG (October 2012). "CoEnzyme Q10 and riboflavin: the mitochondrial connection". Headache (Review). 52 Suppl 2: 81–7. doi:10.1111/j.1526-4610.2012.02233.x. PMID 23030537.
- ↑ Yorns WR, Hardison HH (September 2013). "Mitochondrial dysfunction in migraine". Semin Pediatr Neurol 20 (3): 188–93. doi:10.1016/j.spen.2013.09.002. PMID 24331360.
- ↑ Pringsheim T, Davenport W, Mackie G; et al. (March 2012). "Canadian Headache Society guideline for migraine prophylaxis". Can J Neurol Sci 39 (2 Suppl 2): S1–59. PMID 22683887.
- ↑ Banach M, Serban C, Sahebkar A, Ursoniu S, Rysz J, Muntner P, Toth PP, Jones SR, Rizzo M, Glasser SP, Lip GY, Dragan S, Mikhailidis DP; Lipid and Blood Pressure Meta-analysis Collaboration Group (January 2015). "Effects of coenzyme Q10 on statin-induced myopathy: a meta-analysis of randomized controlled trials". Mayo Clin Proc (Systematic Review and Meta-Analysis) 90 (1): 24–34. doi:10.1016/j.mayocp.2014.08.021. PMID 25440725.
- ↑ "Coenzyme Q10". American Cancer Society. Retrieved 20 February 2014.
- ↑ T.L.P. Watts, BDS, MDS, PhD, FDS, Department of Periodontology and Preventive Dentistry, UMDS, Guy's Hospital London (1995). "Coënzyme Q10 and periodontal treatment: is there any beneficial effect?". British Dental Journal 178 (6): 209–213. doi:10.1038/sj.bdj.4808715. PMID 7718355.
- ↑ Folkers, K; Hanioka, T; Xia, L; McRee Jr, J; Langsjoen, P (1991). "Coenzyme Q10 increases T4/T8 ratios of lymphocytes in ordinary subjects and relevance to patients having the aids related complex". Biochemical and Biophysical Research Communications 176 (2): 786–91. doi:10.1016/S0006-291X(05)80254-2. PMID 1673841.
- ↑ Littarru GP, Nakamura R, Ho L, Folkers K, Kuzell WC (October 1971). "Deficiency of Coenzyme Q10 in Gingival Tissue from Patients with Periodontal Disease". Proc. Natl. Acad. Sci. U.S.A. 68 (10): 2332–5. doi:10.1073/pnas.68.10.2332. PMC 389415. PMID 5289867.
- ↑ Nakamura R, Littarru GP, Folkers K, Wilkinson EG (April 1974). "Study of CoQ10-Enzymes in Gingiva from Patients with Periodontal Disease and Evidence for a Deficiency of Coenzyme Q10". Proc. Natl. Acad. Sci. U.S.A. 71 (4): 1456–60. doi:10.1073/pnas.71.4.1456. PMC 388248. PMID 4151519.
- ↑ McRee JT, Hanioka T, Shizukuishi S, Folkers K (1993). "Therapy with coenzyme Q10 for patients with periodontal disease". J Dent Health 43 (5): 659–666. doi:10.5834/jdh.43.659.
- ↑ Hanioka T, Tanaka M, Ojima M, Shizukuishi S, Folkers K (1994). "Effect of topical application of coenzyme Q10 on adult periodontitis". Mol. Aspects Med. 15 (Suppl): S241–8. doi:10.1016/0098-2997(94)90034-5. PMID 7752836.
- ↑ Wilkinson, EG; Arnold, RM; Folkers, K (1976). "Bioenergetics in clinical medicine. VI. adjunctive treatment of periodontal disease with coenzyme Q10". Research communications in chemical pathology and pharmacology 14 (4): 715–9. PMID 785563.
- ↑ Liu J, Wang LN, Zhan SY, Xia Y (2012). "WITHDRAWN: Coenzyme Q10 for Parkinson's disease". Cochrane Database Syst Rev 5: CD008150. doi:10.1002/14651858.CD008150.pub3. PMID 22592726.
- ↑ http://www.sciencemag.org/content/336/6086/1241
- 1 2 http://www.mbschachter.com/coenzyme_q10.htm
- ↑ Bentinger M, Tekle M, Dallner G (May 2010). "Coenzyme Q—biosynthesis and functions". Biochem. Biophys. Res. Commun. 396 (1): 74–9. doi:10.1016/j.bbrc.2010.02.147. PMID 20494114.
- ↑ Carmen Espinós; Vicente Felipo; Francesc Palau (1 August 2009). Inherited Neuromuscular Diseases: Translation from Pathomechanisms to Therapies. Springer. pp. 122–. ISBN 978-90-481-2812-9. Retrieved 4 January 2011.
- 1 2 Bhagavan, Hemmi N.; Chopra, Raj K. (2006). "Coenzyme Q10: Absorption, tissue uptake, metabolism and pharmacokinetics". Free Radical Research 40 (5): 445–53. doi:10.1080/10715760600617843. PMID 16551570.
- ↑ Bogentoft 1991
- ↑ Ochiai A, Itagaki S, Kurokawa T, Kobayashi M, Hirano T, Iseki K (August 2007). "Improvement in intestinal coenzyme Q10 absorption by food intake". Yakugaku Zasshi 127 (8): 1251–4. doi:10.1248/yakushi.127.1251. PMID 17666877.
- 1 2 3 4 Zmitek et al. (2008) Agro Food Ind. Hi Tec. 19, 4, 9. – Improving the bioavailability of CoQ10
- ↑ Kishi, H.; Kanamori, N.; Nisii, S.; Hiraoka, E.; Okamoto, T.; Kishi, T. (1964). "Metabolism and Exogenous Coenzyme Q10 in vivo and Bioavailability of Coenzyme Q10 Preparations in Japan". Biomedical and Clinical Aspects of Coenzyme Q. Amsterdam: Elsevier. pp. 131–42.
- 1 2 3 Ozawa, Y; Mizushima, Y; Koyama, I; Akimoto, M; Yamagata, Y; Hayashi, H; Murayama, H (1986). "Intestinal absorption enhancement of coenzyme Q10 with a lipid microsphere". Arzneimittel-Forschung 36 (4): 689–90. PMID 3718593.
- ↑ Tomono, Y; Hasegawa, J; Seki, T; Motegi, K; Morishita, N (1986). "Pharmacokinetic study of deuterium-labelled coenzyme Q10 in man". International journal of clinical pharmacology, therapy, and toxicology 24 (10): 536–41. PMID 3781673.
- ↑ Mathiowitz, Edith; Jacob, Jules S.; Jong, Yong S.; Carino, Gerardo P.; Chickering, Donald E.; Chaturvedi, Pravin; Santos, Camilla A.; Vijayaraghavan, Kavita; Montgomery, Sean; Bassett, Michael; Morrell, Craig (1997). "Biologically erodible microspheres as potential oral drug delivery systems". Nature 386 (6623): 410–4. doi:10.1038/386410a0. PMID 9121559.
- ↑ Hsu CH, Cui Z, Mumper RJ, Jay M (2003). "Preparation and characterization of novel coenzyme Q10 nanoparticles engineered from microemulsion precursors". AAPS PharmSciTech 4 (3): 24–35. doi:10.1208/pt040332. PMC 2750625. PMID 14621964.
- ↑ Joshi SS, Sawant SV, Shedge A, Halpner AD (January 2003). "Comparative bioavailability of two novel coenzyme Q10 preparations in humans". Int J Clin Pharmacol Ther 41 (1): 42–8. doi:10.5414/CPP41042. PMID 12564745.
- ↑ Kommuru, TR; Ashraf, M; Khan, MA; Reddy, IK (1999). "Stability and bioequivalence studies of two marketed formulations of coenzyme Q10 in beagle dogs". Chemical & pharmaceutical bulletin 47 (7): 1024–8. doi:10.1248/cpb.47.1024. PMID 10434405.
- ↑ Bhagavan HN, Chopra RK (June 2007). "Plasma coenzyme Q10 response to oral ingestion of coenzyme Q10 formulations". Mitochondrion 7 (Suppl): S78–88. doi:10.1016/j.mito.2007.03.003. PMID 17482886.
- ↑ K. Westesen and B. Siekmann. Particles with modified physicochemical properties, their preparation and uses. US6197349. 2001.
- ↑ H. Ohashi, T. Takami, N. Koyama, Y. Kogure and K. Ida. Aqueous solution containing ubidecarenone. US4483873. 1984
- ↑ Žmitek, Janko; Smidovnik, Andrej; Fir, Maja; Prosek, Mirko; Zmitek, Katja; Walczak, Jaroslaw; Pravst, Igor (2008). "Relative Bioavailability of Two Forms of a Novel Water-Soluble Coenzyme Q10". Annals of Nutrition and Metabolism 52 (4): 281–7. doi:10.1159/000129661. PMID 18645245.
- ↑ Kagan, Daniel; Madhavi, Doddabele (2010). "A Study on the Bioavailability of a Novel Sustained-Release Coenzyme Q10-ß-Cyclodextrin Complex". Integrative Medicine 9 (1).
- ↑ Crane, F; Hatefi, Y; Lester, R; Widmer, C (1957). "Isolation of a quinone from beef heart mitochondria". Biochimica et Biophysica Acta 25 (1): 220–1. doi:10.1016/0006-3002(57)90457-2. PMID 13445756.
- ↑ Peter H. Langsjoen,"Introduction of Coezyme Q10"
- ↑ Mellors A, Tappel A, (1966). "The Inhibition of Mitochondrial Peroxidation by Ubiquinone and Ubiquinol". J. Biol. Chem. 241 (19): 4353–4356. PMID 5922959.
- ↑ Mellors A, Tappel A, (July 1966). "Quinones and Quinols as Inhibitors of Lipid Peroxidation". Lipids 1 (4): 282–284. doi:10.1007/BF02531617. PMID 17805631.
- 1 2 3 4 5 Pravst, Igor; Zmitek, Katja; Zmitek, Janko (2010). "Coenzyme Q10 Contents in Foods and Fortification Strategies". Critical Reviews in Food Science and Nutrition 50 (4): 269–80. doi:10.1080/10408390902773037. PMID 20301015.
- ↑ Weber, C; Bysted, A; Hłlmer, G (1997). "The coenzyme Q10 content of the average Danish diet". Int J Vitam Nutr Res 67 (2): 123–9. PMID 9129255.
External links
- List of USP Verified CoQ10 Ingredients
- National Cancer Institute page on Coenzyme Q10
- Robert Alan Bonakdar and Erminia Guarneri, American Family Physician page on Coenzyme Q10
| ||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||
| ||||||||||||||