Clearing the cervical spine
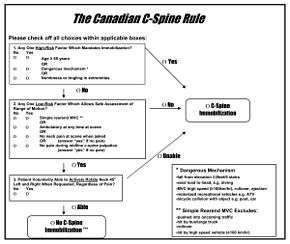
Clearing the cervical spine is the process by which medical professionals determine whether cervical spine injuries exist. This process can take place in the emergency department or take place in the field by appropriately trained EMS personnel. The following is based on the NEXUS (National Emergency X-Radiography Utilization Study) criteria.[1] There are other clinical criteria in common use, such as the Canadian C-spine rule.[2]
Excluding a cervical spinal injury requires clinical judgement and training.
When a significant mechanism of injury is present, a cervical spine is determined to be stable if:
- There is no posterior midline cervical tenderness
- There is no evidence of intoxication
- The patient is alert and oriented to person, place, time, and event
- There is no focal neurological deficit (see focal neurological signs)
- There are no painful distracting injuries (e.g., long bone fracture)
If the patient does not meet all the above criteria then they require a three view cervical x-ray series, adding a swimmer's view if the lateral doesn't include the C7/T1 interface. In those with degenerative disease of the cervical spine, a plain film series is often inadequate to assess for injury. Plain radiographs, even when technically optimal, my fail to reveal significant injury. If there is clinical suspicion, a Computerized Tomography (CT Scan) may be needed to rule out a fracture, and flexion-extension radiographs or Magnetic Resonance Imaging to exclude a ligament injury.[3]
If the patient is obtunded, i.e. has a head injury with altered sensorium, is intoxicated, or has been given potent analgesics, the cervical spine must remain immobilized until a clinical examination becomes possible.[4]
If the patient is not expected to be clinically evaluable within 48–72 hours because of severe head or multiple injuries, they should remain immobilized until a time when such an examination is possible. A 64-slice CT with reconstructions does not entirely rule out ligamentous injury leading to instability, but is a practical means of identifying the majority of C-spine injuries in obtunded patients. MR C-spine suffers from frequent false-positives, limiting its usefulness. In these cases, a consultation with a Spine Surgery specialist is prudent.
The indication for MR spine is a focal neurological deficit. Another indication for MR of the cervical spine is persistent mid-line neck pain or tenderness despite a normal CT in the awake patient.
Neurosurgeons or orthopaedic surgeons manage any detected injury. Today, most large centers have Spine Surgery specialists, that have trained in this field after their Orthopedic or Neurosurgical residency.
See also
References
- ↑ Hoffman JR, Wolfson AB, Todd K, Mower WR. (1998). "Selective cervical spine radiography in blunt trauma: methodology of the National Emergency X-Radiography Utilization Study (NEXUS).". Ann Emerg Med. 32 (4): 461–9. doi:10.1016/s0196-0644(98)70176-3. PMID 9774931.
- ↑ Canadian CT Head and C-Spine (CCC) Study Group. (2004). "Canadian C-Spine Rule study for alert and stable trauma patients: I. Background and rationale.". CJEM 4 (2): 84–90. PMID 17612425.
- ↑ Jaeseong, Jason (2015). "The utility of flexion–extension radiography for the detection of ligamentous cervical spine injury and its current role in the clearance of the cervical spine". Emergency Medicine Australasia. doi:10.1111/1742-6723.12525.
- ↑ Morris CGT, McCoy E. (2004). "Clearing the cervical spine in unconscious polytrauma victims, balancing risks and effective screening". Anasthesia 59: 464–482. doi:10.1111/j.1365-2044.2004.03666.x.
External links
- Wilderness Medicine Protocols
- State of Maine EMS Protocols
- NEXUS Criteria for C-Spine Imaging
- Canadian C-Spine Rule