Chronic kidney disease
| Chronic kidney disease | |
|---|---|
 Uremic frost on the forehead and scalp of a young man who presented with complaints of chronic anorexia and fatigue with blood urea nitrogen and serum creatinine levels around 100 and 50 mg/dl, respectively | |
| Classification and external resources | |
| Specialty | Nephrology |
| ICD-10 | N18 |
| ICD-9-CM | 585.9 585.1-585.5 403 |
| DiseasesDB | 11288 |
| MedlinePlus | 000471 |
| eMedicine | article/238798 |
| Patient UK | Chronic kidney disease |
| MeSH | D007676 |
Chronic kidney disease (CKD), also known as chronic renal disease, is progressive loss in kidney function over a period of months or years. The symptoms of worsening kidney function are not specific, and might include feeling generally unwell and experiencing a reduced appetite. Often, chronic kidney disease is diagnosed as a result of screening of people known to be at risk of kidney problems, such as those with high blood pressure or diabetes and those with a blood relative with CKD. This disease may also be identified when it leads to one of its recognized complications, such as cardiovascular disease, anemia, pericarditis or renal osteodystrophy (the latter included in the novel term CKD-MBD).[1][2] CKD is a long-term form of kidney disease; thus, it is differentiated from acute kidney disease (acute kidney injury) in that the reduction in kidney function must be present for over 3 months. CKD is an internationally recognized public health problem affecting 5–10% of the world population.[3][4]
Chronic kidney disease is identified by a blood test for creatinine, which is a breakdown product of muscle metabolism. Higher levels of creatinine indicate a lower glomerular filtration rate and as a result a decreased capability of the kidneys to excrete waste products. Creatinine levels may be normal in the early stages of CKD, and the condition is discovered if urinalysis (testing of a urine sample) shows the kidney is allowing the loss of protein or red blood cells into the urine. To fully investigate the underlying cause of kidney damage, various forms of medical imaging, blood tests, and sometimes a kidney biopsy (removing a small sample of kidney tissue) are employed to find out if a reversible cause for the kidney malfunction is present.[1]
Previous professional guidelines classified the severity of CKD in five stages, with stage 1 being the mildest and usually causing few symptoms and stage 5 being a severe illness with poor life expectancy if untreated. Stage 5 CKD is often called end-stage kidney disease, end-stage renal disease, or end-stage kidney failure, and is largely synonymous with the now outdated terms chronic renal failure or chronic kidney failure; and usually means the patient requires renal replacement therapy, which may involve a form of dialysis, but ideally constitutes a kidney transplant. Recent international guidelines (KDIGO 2012) reclassified CKD based on cause, glomerular filtration rate category (G1,G2,G3a,G3b,G4 and G5), and albuminuria category (A1,A2,A3).[5]
Screening of at-risk people is important because treatments exist that delay the progression of CKD.[6] If an underlying cause of CKD, such as vasculitis, or obstructive nephropathy (blockage to the drainage system of the kidneys) is found, it may be treated directly to slow the damage. In more advanced stages, treatments may be required for anemia and kidney bone disease [also called renal osteodystrophy, secondary hyperparathyroidism or chronic kidney disease - mineral bone disorder (CKD-MBD)]. Chronic kidney disease resulted in 956,000 deaths in 2013 up from 409,000 deaths in 1990.[7]
Signs and symptoms
CKD is initially without specific symptoms and is generally only detected as an increase in serum creatinine or protein in the urine. As the kidney function decreases:
- Blood pressure is increased due to fluid overload and production of vasoactive hormones created by the kidney via the renin-angiotensin system, increasing one's risk of developing hypertension and/or suffering from congestive heart failure.
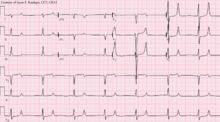
- Urea accumulates, leading to azotemia and ultimately uremia (symptoms ranging from lethargy to pericarditis and encephalopathy). Due to its high systemic circulation, urea is excreted in eccrine sweat at high concentrations and crystallizes on skin as the sweat evaporates ("uremic frost").
- Potassium accumulates in the blood (hyperkalemia with a range of symptoms including malaise and potentially fatal cardiac arrhythmias). Hyperkalemia usually does not develop until the glomerular filtration rate falls to less than 20-25 ml/min/1.73 m2, at which point the kidneys have decreased ability to excrete potassium. Hyperkalemia in CKD can be exacerbated by acidemia (which leads to extracellular shift of potassium) and from lack of insulin.[8]
- Erythropoietin synthesis is decreased causing anemia.
- Fluid volume overload symptoms may range from mild edema to life-threatening pulmonary edema.
- Hyperphosphatemia, due to reduced phosphate excretion, follows the decrease in glomerular filtration. Hyperphosphatemia is associated with increased cardiovascular risk, being a direct stimulus to vascular calcification.[9] Moreover, circulating concentrations of fibroblast growth factor-23 (FGF-23) increase progressively as the renal capacity for phosphate excretion declines, but this adaptative response may also contribute to left ventricular hypertrophy and increased mortality in CKD patients.[10][11]
- Hypocalcemia, due to 1,25 dihydroxyvitamin D3 deficiency (caused by stimulation of FGF-23 and reduction of renal mass),[12] and resistance to the calcemic action of parathyroid hormone.[13] Osteocytes are responsible for the increased production of FGF23, which is a potent inhibitor of the enzyme 1-alpha-hydroxylase (responsible for the conversion of 25-hydroxycholecalciferol into 1,25 dihydroxyvitamin D3).[14] Later, this progresses to secondary hyperparathyroidism, renal osteodystrophy, and vascular calcification that further impairs cardiac function. An extreme consequence is the occurrence of the rare condition named calciphylaxis.[15]

- The current concept of chronic kidney disease-mineral bone disorder (CKD-MBD)[2][16] currently describes a broader clinical syndrome that develops as a systemic disorder of mineral and bone metabolism due to CKD manifested by either one or a combination of: 1) abnormalities of calcium, phosphorus (phosphate), parathyroid hormone, or vitamin D metabolism; 2) abnormalities in bone turnover, mineralization, volume, linear growth, or strength (renal osteodystrophy); and 3) vascular or other soft-tissue calcification.[2] CKD-MBD has been associated to poor hard outcomes.[2]
- Metabolic acidosis (due to accumulation of sulfates, phosphates, uric acid etc.) may cause altered enzyme activity by excess acid acting on enzymes; and also increased excitability of cardiac and neuronal membranes by the promotion of hyperkalemia due to excess acid (acidemia).[17] Acidosis is also due to decreased capacity to generate enough ammonia from the cells of the proximal tubule.[8]
- Iron deficiency anemia, which increases in prevalence as kidney function decreases, is especially prevalent in those requiring haemodialysis. It is multifactoral in cause, but includes increased inflammation, reduction in erythropoietin, and hyperuricemia leading to bone marrow suppression.
People with CKD suffer from accelerated atherosclerosis and are more likely to develop cardiovascular disease than the general population. Patients afflicted with CKD and cardiovascular disease tend to have significantly worse prognoses than those suffering only from the latter.[18]
Sexual dysfunction is very common in both men and women with CKD. A majority of men have a reduced sex drive, difficulty obtaining an erection, and reaching orgasm, and the problems get worse with age. A majority of women have trouble with sexual arousal, and painful menstruation and problems with performing and enjoying sex are common.[19]
Causes
The most common recognised cause of CKD is diabetes mellitus. Others include idiopathic (i.e. unknown cause, often associated with small kidneys on renal ultrasound), hypertension, and glomerulonephritis.[20] Together, these cause about 75% of all adult cases.
Historically, kidney disease has been classified according to the part of the kidney anatomy involved.[21]
- Vascular disease includes large vessel disease such as bilateral renal artery stenosis and small vessel disease such as ischemic nephropathy, hemolytic-uremic syndrome, and vasculitis.
- Glomerular disease comprises a diverse group and is classified into:
- Primary glomerular disease such as focal segmental glomerulosclerosis and IgA nephropathy (or nephritis)
- Secondary glomerular disease such as diabetic nephropathy and lupus nephritis
- Congenital disease such as polycystic kidney disease.
- Tubulointerstitial disease includes drug- and toxin-induced chronic tubulointerstitial nephritis, and reflux nephropathy.
- Obstructive nephropathy is exemplified by bilateral kidney stones and diseases of the prostate.
- On rare cases, pinworms infecting the kidney can also cause nephropathy.
- Nontraditional causes of CKD (CKDu) are denoted if the common causes of CKD are not present:
- CKD of unknown etiology is the subject of a major study by the Sri Lanka Ministry of Health and the World Health Organization 2009–2012.[22]
- Mesoamerican nephropathy, a form of CKDu, is "a new form of kidney disease that could be called agricultural nephropathy".[23]
Diagnosis
Diagnosis of CKD is largely based on the clinical picture combined with the measurement of the serum creatinine level (see above).
Etiology
In many CKD patients, previous kidney disease or other underlying diseases are already known. A significant number present with CKD of unknown cause. In these patients, a cause is occasionally identified retrospectively.
Differential diagnosis
It is important to differentiate CKD from acute kidney injury (AKI) because AKI can be reversible. Abdominal ultrasound, in which the size of the kidneys is measured, is commonly performed. Kidneys with CKD are usually smaller (≤ 9 cm) than normal kidneys, with notable exceptions such as in early diabetic nephropathy and polycystic kidney disease. Another diagnostic clue that helps differentiate CKD from AKI is a gradual rise in serum creatinine (over several months or years) as opposed to a sudden increase in the serum creatinine (several days to weeks). If these levels are unavailable (because the patient has been well and has had no blood tests), it is occasionally necessary to treat a patient briefly as having AKI until the kidney impairment has been established to be irreversible.
Work-up
Additional tests may include nuclear medicine MAG3 scan to confirm blood flow and establish the differential function between the two kidneys. Dimercaptosuccinic acid (DMSA) scans are also used in kidney imaging; with both MAG3 and DMSA being used chelated with the radioactive element technetium-99.
Toxins
In CKD numerous uremic toxins accumulate in the blood. Even when ESKD (largely synonymous with CKD5) is treated with dialysis, the toxin levels do not go back to normal as dialysis is not that efficient. Similarly, after a kidney transplant, the levels may not go back to normal as the transplanted kidney may not work 100%. If it does, the creatinine level is often normal. The toxins show various cytotoxic activities in the serum and have different molecular weights, and some of them are bound to other proteins, primarily to albumin. Such toxic protein-bound substances are receiving the attention of scientists who are interested in improving the standard chronic dialysis procedures used today.
Screening
Screening those who have neither symptoms nor risk factors for CKD is not recommended.[24] Those who should be screened include: those with hypertension or history of cardiovascular disease, those with diabetes or marked obesity, those aged > 60 years, subjects with indigenous racial origin, those with a history of kidney disease in the past, and subjects who have relatives who had kidney disease requiring dialysis. Screening should include calculation of estimated GFR from the serum creatinine level, and measurement of urine albumin-to-creatinine ratio (ACR) in a first-morning urine specimen (this reflects the amount of a protein called albumin in the urine), as well as a urine dipstick screen for hematuria.[25] The GFR (glomerular filtration rate) is derived from the serum creatinine and is proportional to 1/creatinine, i.e. it is a reciprocal relationship (the higher the creatinine, the lower the GFR). It reflects one aspect of kidney function: how efficiently the glomeruli (filtering units) work. But as they make up <5% of the mass of the kidney, the GFR does not tell you about all aspects of kidney health and function. This can be done by combining the GFR level with the clinical assessment of the patient (especially fluid state) and measuring the levels of hemoglobin, potassium, phosphate and parathyroid hormone (PTH). Normal GFR is 90-120 mls/min. The units of creatinine vary from country to country.
Referral to nephrologist
Guidelines for referral to a nephrologist vary between countries. Though most would agree that nephrology referral is required by Stage 4 CKD (when eGFR/1.73m2 is less than 30 ml/min; or decreasing by more than 3 ml/min/year); and may be useful at an earlier stage (e.g. CKD3) when urine albumin-to-creatinine ratio is more than 30 mg/mmol, when blood pressure is difficult to control, or when hematuria or other findings suggest either a primarily glomerular disorder or secondary disease amenable to specific treatment. Other benefits of early nephrology referral include proper patient education regarding options for renal replacement therapy as well as pre-emptive transplantation, and timely workup and placement of an arteriovenous fistula in those patients opting for future hemodialysis
Severity-based stages
| CKD Stage | GFR level (mL/min/1.73 m2) |
|---|---|
| Stage 1 | ≥ 90 |
| Stage 2 | 60 – 89 |
| Stage 3 | 30 – 59 |
| Stage 4 | 15 – 29 |
| Stage 5 | < 15 |
All individuals with a glomerular filtration rate (GFR) <60 ml/min/1.73 m2 for 3 months are classified as having chronic kidney disease, irrespective of the presence or absence of kidney damage. The rationale for including these individuals is that reduction in kidney function to this level or lower represents loss of half or more of the adult level of normal kidney function, which may be associated with a number of complications such as the development of cardiovascular disease.[1]
The loss of protein in the urine is regarded as an independent marker for worsening of kidney function and cardiovascular disease. Hence, British guidelines append the letter "P" to the stage of chronic kidney disease if protein loss is significant.[26]
- Stage 1
Slightly diminished function; kidney damage with normal or relatively high GFR (≥90 ml/min/1.73 m2). Kidney damage is defined as pathological abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies.[1]
- Stage 2
Mild reduction in GFR (60–89 ml/min/1.73 m2) with kidney damage. Kidney damage is defined as pathological abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies.[1]
- Stage 3
Moderate reduction in GFR (30–59 ml/min/1.73 m2):.[1] British guidelines distinguish between stage 3A (GFR 45–59) and stage 3B (GFR 30–44) for purposes of screening and referral.[26]
- Stage 4
Severe reduction in GFR (15–29 ml/min/1.73 m2)[1] Preparation for renal replacement therapy.
- Stage 5
Established kidney failure (GFR <15 ml/min/1.73 m2), permanent renal replacement therapy,[1] or end-stage kidney disease.
NDD-CKD vs. ESRD
The term "non-dialysis-dependent chronic kidney disease" (NDD-CKD) is a designation used to encompass the status of those persons with an established CKD who do not yet require the life-supporting treatments for kidney failure known as renal replacement therapy (RRT, including maintenance dialysis or kidney transplantation). The condition of individuals with CKD, who require either of the two types of renal replacement therapy (dialysis or transplant), is referred to as the end-stage kidney disease (ESKD). Hence, the start of the ESKD is practically the irreversible conclusion of the NDD-CKD. Even though the NDD-CKD status refers to the status of persons with earlier stages of CKD (stages 1 to 4), patients with advanced stage of CKD (stage 5), who have not yet started renal replacement therapy, are also referred to as NDD-CKD.
Treatment
The presence of CKD confers a markedly increased risk of cardiovascular disease, and people with CKD often have other risk factors for heart disease, such as high blood lipids. The most common cause of death in people with CKD is cardiovascular disease rather than kidney failure. Aggressive treatment of hyperlipidemia is warranted.[27]
Apart from controlling other risk factors, the goal of therapy is to slow down or halt the progression of CKD to stage 5. Control of blood pressure and treatment of the original disease, whenever feasible, are the broad principles of management. Generally, angiotensin converting enzyme inhibitors (ACEIs) or angiotensin II receptor antagonists (ARBs) are used, as they have been found to slow the progression of CKD to kidney failure.[28] They have also been found to reduce the risk of major cardiovascular events such as myocardial infarction, stroke, heart failure, and death from cardiovascular disease when compared to placebo in individuals with CKD.[28] Furthermore, ACEIs may be superior to ARBs for protection against progression to kidney failure and death from any cause in those with CKD.[28]
Although the use of ACE inhibitors and ARBs represents the current standard of care for people with CKD, people progressively lose kidney function while on these medications, as seen in the IDNT[29] and RENAL[30] studies, which reported a decrease over time in estimated GFR (an accurate measure of CKD progression, as detailed in the K/DOQI guidelines[1]) in people treated by these conventional methods.
Replacement of erythropoietin and calcitriol, two hormones processed by the kidney, is often necessary in people with advanced disease. Guidelines[31] recommend treatment with parenteral iron prior to treatment with erythropoietin. A target hemoglobin level of 9–12 g/dl is recommended.[32][33] The normalization of hemoglobin has not been found to be of benefit.[34] It is unclear if androgens help with anemia.[35] Phosphate binders are also used to control the serum phosphate levels, which are usually elevated in advanced chronic kidney disease. Although the evidence for them is limited, phosphodiesterase-5 inhibitors and zinc show potential for helping men with sexual dysfunction.[19]
At stage 5 CKD, renal replacement therapy is usually required, in the form of either dialysis or a transplant.
Prognosis
The prognosis of patients with chronic kidney disease is guarded as epidemiological data have shown that all cause mortality (the overall death rate) increases as kidney function decreases.[36] The leading cause of death in patients with chronic kidney disease is cardiovascular disease, regardless of whether there is progression to stage 5.[36][37][38]
While renal replacement therapies can maintain patients indefinitely and prolong life, the quality of life is severely affected.[39][40] Kidney transplantation increases the survival of patients with stage 5 CKD significantly when compared to other therapeutic options;[41][42] however, it is associated with an increased short-term mortality due to complications of the surgery. Transplantation aside, high-intensity home hemodialysis appears to be associated with improved survival and a greater quality of life, when compared to the conventional three-times-a-week hemodialysis and peritoneal dialysis.[43]
Cancer risk
Patients with ESKD are at increased overall risk for cancer.[44] This risk is particularly high in younger patients and gradually diminishes with age.[44] Medical specialty professional organizations recommend that physicians do not perform routine cancer screening in patients with limited life expectancies due to ESKD because evidence does not show that such tests lead to improved patient outcomes.[45][46]
Epidemiology
Chronic kidney disease resulted in 956,000 deaths in 2013 up from 409,000 deaths in 1990.[7]
In Canada, 1.9 to 2.3 million people have CKD.[34] The U.S. Centers for Disease Control and Prevention found that CKD affected an estimated 16.8% of U.S. adults aged 20 years and older, during 1999 to 2004.[47] UK estimates suggest that 8.8% of the population of Great Britain and Northern Ireland have symptomatic CKD.[48]
CKD is a major concern in African Americans, mostly due to increased prevalence of hypertension. As an example, 37% of ESKD cases in African Americans can be attributed to high blood pressure, compared with 19% among Caucasians.[49] Treatment efficacy also differs between racial groups. Administration of antihypertensive drugs generally halts disease progression in white populations, but has little effect in slowing kidney disease among blacks, and additional treatment such as bicarbonate therapy is often required.[49] While lower socioeconomic status contributes to prevalence of CKD, significant differences in CKD prevalence are still evident between African Americans and Whites when controlling for environmental factors.[49]
Studies have shown a true association between history of chronic kidney disease in first- or second-degree relatives, and risk of disease.[50] In addition, African Americans may have higher serum levels of human leukocyte antigens (HLA).[50] High HLA concentrations can contribute to increased systemic inflammation, which indirectly may lead to heightened susceptibility for developing kidney disease. Lack of nocturnal reduction in blood pressure among groups of African Americans is also offered as an explanation,[50] which lends further credence to a genetic etiology of CKD racial disparities.
A high and so-far unexplained incidence of CKD, referred to as the Mesoamerican nephropathy, has been noted among male workers in Central America, mainly in sugar cane fields in the lowlands of El Salvador and Nicaragua. Heat stress from long hours of piece-rate work at high average temperatures[51][52][53][54] (in the range of 96 °F) is suspected, as are agricultural chemicals[55][56] and other factors. In Sri Lanka, another epidemic of CKD of unknown etiology has become a serious public health concern.[22]
Society and culture
In the USA, the National Kidney Foundation is a national organization representing patients and professionals who treat kidney diseases. The American Kidney Fund is a national nonprofit organization providing treatment-related financial assistance to one of every five dialysis patients each year. The Renal Support Network is a nonprofit, patient-focused, patient-run organization that provides nonmedical services to those affected by CKD. The American Association of Kidney Patients is a nonprofit, patient-centric group focused on improving the health and well-being of CKD and dialysis patients. The Renal Physicians Association is an association representing nephrology professionals.
In the United Kingdom, the UK National Kidney Federation and British Kidney Patient Association (BKPA) represents patients, and the Renal Association represents renal physicians and works closely with the National Service Framework for kidney disease.
Kidney Health Australia serves that country.
The International Society of Nephrology is an international body representing specialists in kidney diseases.
Research
Currently, several compounds are in development for the treatment of CKD. These include the angiotensin receptor blocker (ARB) olmesartan medoxomil [citation needed]; and sulodexide, a mixture of low molecular weight heparin and dermatan sulfate [citation needed].
References
- 1 2 3 4 5 6 7 8 9 National Kidney Foundation (2002). "K/DOQI clinical practice guidelines for chronic kidney disease". Retrieved 2008-06-29.
- 1 2 3 4 KDIGO: Kidney Disease Improving Global Outcomes. "KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD)" (PDF).
- ↑ Eknoyan G, Lameire N, Barsoum R; et al. ""The burden of kidney disease: improving global outcomes.".". Kidney Int 66: 1310–1314; 2004.
- ↑ A Martínez-Castelao, JL. Górriz, J Bover; et al. "Consensus document for the detection and management of chronic kidney disease". Nefrologia 34(2):243-62; 2014. doi:10.3265/Nefrologia.pre2014.Feb.12455.
- ↑ KDIGO (Kidney Disease Improving Global Outcomes. "KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease" (PDF). Kidney Int Suppl 3 (1): 1-150; 2013. Retrieved 5 February 2016.
- ↑ Plantinga LC, Tuot DS, Powe NR (2010). "Awareness of chronic kidney disease among patients and providers". Adv Chronic Kidney Dis 17 (3): 225–236. doi:10.1053/j.ackd.2010.03.002. PMC 2864779. PMID 20439091.
- 1 2 GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.". Lancet 385 (9963): 117–171. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- 1 2 "Chronic Kidney Disease". medscape.
- ↑ Hruska KA, Mathew S, Lund R, Qiu P, Pratt R (2008). "Hyperphosphatemia of chronic kidney disease". Kidney Int. 74 (2): 148–57. doi:10.1038/ki.2008.130. PMC 2735026. PMID 18449174.
- ↑ Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, Gutiérrez OM, Aguillon-Prada R, Lincoln J, Hare JM, Mundel P, Morales A, Scialla J, Fischer M, Soliman EZ, Chen J, Go AS, Rosas SE, Nessel L, Townsend RR, Feldman HI, St John Sutton M, Ojo A, Gadegbeku C, Di Marco GS, Reuter S, Kentrup D, Tiemann K, Brand M, Hill JA, Moe OW, Kuro-O M, Kusek JW, Keane MG, Wolf M. (2011). "FGF23 induces left ventricular hypertrophy.". J Clin Invest 121 (11): 4393–408. doi:10.1172/JCI46122.
- ↑ Gutiérrez OM, Mannstadt M, Isakova T, Rauh-Hain JA, Tamez H, Shah A, Smith K, Lee H, Thadhani R, Jüppner H, Wolf M. (2008). "Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis.". N Engl J Med. 7;359(6):584-92. doi:10.1056/NEJMoa0706130.
- ↑ Bacchetta J, Sea JL, Chun RF, Lisse TS, Wesseling-Perry K, Gales B, Adams JS, Salusky IB, Hewison M (August 2012). "FGF23 inhibits extra-renal synthesis of 1,25-dihydroxyvitamin D in human monocytes". J Bone Miner Res. 28 (1): 46–55. doi:10.1002/jbmr.1740. PMC 3511915. PMID 22886720.
- ↑ Bover J, Jara A, Trinidad P, Rodriguez M, Martin-Malo A, Felsenfeld AJ. "The calcemic response to PTH in the rat: effect of elevated PTH levels and uremia.". Kidney Int. 46(2):310-7; 1994.
- ↑ Longo et al., Harrison's Principles of Internal Medicine, 18th ed., p.3109
- ↑ Brandenburg VM1, Cozzolino M, Ketteler M. "Calciphylaxis: a still unmet challenge". J Nephrol. 24(2):142-8; 2011. Retrieved 6 February 2016.
- ↑ Moe S, Drüeke T, Cunningham J, Goodman W, Martin K, Olgaard K, Ott S, Sprague S, Lameire N, Eknoyan G; Kidney Disease: Improving Global Outcomes (KDIGO). "Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO).". Kidney Int. 69(11):1945-53; 2006.
- ↑ Adrogué HJ, Madias NE (September 1981). "Changes in plasma potassium concentration during acute acid-base disturbances". Am. J. Med. 71 (3): 456–67. doi:10.1016/0002-9343(81)90182-0. PMID 7025622.
- ↑ Damman, Kevin; Valente, Mattia A. E.; Voors, Adriaan A.; O'Connor, Christopher M.; Veldhuisen, Dirk J. van; Hillege, Hans L. (2014-02-14). "Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis". European Heart Journal 35 (7): 455–469. doi:10.1093/eurheartj/eht386. ISSN 0195-668X. PMID 24164864.
- 1 2 Vecchio M, Navaneethan SD, Johnson DW, Lucisano G, Graziano G, Saglimbene V, Ruospo M, Querques M, Jannini EA, Strippoli GF (2010). "Interventions for treating sexual dysfunction in patients with chronic kidney disease". Cochrane Database Syst Rev (12): CD007747. doi:10.1002/14651858.CD007747.pub2. PMID 21154382.
- ↑ "United States Renal Data System (USRDS)".
- ↑ Rahman, Mahboob; Smith, Michael C. (September 1998). "Chronic renal insufficiency: A diagnostic and therapeutic approach". Archives of Internal medicine. doi:10.1001/archinte.158.16.1743. PMID 9738603.
- 1 2 Redmon JH, Elledge MF, Womack DS, Wickremashinghe R, Wanigasuriya KP, Peiris-John RJ, Lunyera J, Smith K, Raymer JH, Levine KE (2014). "Additional perspectives on chronic kidney disease of unknown aetiology (CKDu) in Sri Lanka – lessons learned from the WHO CKDu population prevalence study". BMC Nephrology 15 (1): 125. doi:10.1186/1471-2369-15-125. PMC 4120717. PMID 25069485.
- ↑ Orantes CM, Herrera R, Almaguer M, Brizuela EG, Núñez L, Alvarado NP, Fuentes EJ, Bayarre HD, Amaya JC, Calero DJ, Vela XF, Zelaya SM, Granados DV, Orellana P (2014). "Epidemiology of chronic kidney disease in adults of Salvadoran agricultural communities". MEDICC Rev 16 (2): 23–30. PMID 24878646.
- ↑ Qaseem A, Hopkins RH, Sweet DE, Starkey M, Shekelle P (22 October 2013). "Screening, Monitoring, and Treatment of Stage 1 to 4 Chronic Kidney Disease: A Clinical Practice Guideline From the Clinical Guidelines Committee of the American College of Physicians.". Annals of internal medicine 159 (12): 835–47. doi:10.7326/0003-4819-159-12-201312170-00726. PMID 24145991.
- ↑ Johnson, David (2011-05-02). "Chapter 4: CKD Screening and Management: Overview". In Daugirdas, John. Handbook of Chronic Kidney Disease Management. Lippincott Williams and Wilkins. pp. 32–43. ISBN 1-58255-893-0.
- 1 2 National Institute for Health and Clinical Excellence. Clinical guideline 73: Chronic kidney disease. London, 2008.
- ↑ Chauhan V, Vaid M (November 2009). "Dyslipidemia in chronic kidney disease: managing a high-risk combination". Postgrad Med 121 (6): 54–61. doi:10.3810/pgm.2009.11.2077. PMID 19940417.
- 1 2 3 Xie, X; Liu, Y; Perkovic, V; Li, X; Ninomiya, T; Hou, W; Zhao, N; Liu, L; Lv, J; Zhang, H; Wang, H (November 2015). "Renin-Angiotensin System Inhibitors and Kidney and Cardiovascular Outcomes in Patients With CKD: A Bayesian Network Meta-analysis of Randomized Clinical Trials.". American Journal of Kidney Diseases (Systematic Review & Meta-Analysis). S0272-6386 (15): 01312–8. doi:10.1053/j.ajkd.2015.10.011. PMID 26597926.
- ↑ Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I (2001). "Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes". N Engl J Med 345 (12): 851–60. doi:10.1056/NEJMoa011303. PMID 11565517.
- ↑ Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S (2001). "Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy". N Engl J Med 345 (12): 861–9. doi:10.1056/NEJMoa011161. PMID 11565518.
- ↑ "Anaemia management in people with chronic kidney disease (CG114)". NICE Clinical Guideline. UK National Institute for Health and Care Excellence. February 2011.
- ↑ Locatelli F, Aljama P, Canaud B, Covic A, De Francisco A, Macdougall IC, Wiecek A, Vanholder R (September 2010). "Target haemoglobin to aim for with erythropoiesis-stimulating agents: a position statement by ERBP following publication of the Trial to reduce cardiovascular events with Aranesp therapy (TREAT) study". Nephrol Dial Transplant 25 (9): 2846–50. doi:10.1093/ndt/gfq336. PMID 20591813.
- ↑ Clement FM, Klarenbach S, Tonelli M, Johnson JA, Manns BJ (22 June 2009). "The impact of selecting a high hemoglobin target level on health-related quality of life for patients with chronic kidney disease: a systematic review and meta-analysis". Archives of Internal Medicine 169 (12): 1104–12. doi:10.1001/archinternmed.2009.112. PMID 19546410.
- 1 2 Levin A, Hemmelgarn B, Culleton B, Tobe S, McFarlane P, Ruzicka M, Burns K, Manns B, White C, Madore F, Moist L, Klarenbach S, Barrett B, Foley R, Jindal K, Senior P, Pannu N, Shurraw S, Akbari A, Cohn A, Reslerova M, Deved V, Mendelssohn D, Nesrallah G, Kappel J, Tonelli M (November 2008). "Guidelines for the management of chronic kidney disease". CMAJ 179 (11): 1154–62. doi:10.1503/cmaj.080351. PMC 2582781. PMID 19015566.
- ↑ Yang, Q; Abudou, M; Xie, XS; Wu, T (Oct 9, 2014). "Androgens for the anaemia of chronic kidney disease in adults.". The Cochrane database of systematic reviews 10: CD006881. doi:10.1002/14651858.CD006881.pub2. PMID 25300168.
- 1 2 Perazella MA, Khan S (March 2006). "Increased mortality in chronic kidney disease: a call to action". Am. J. Med. Sci. 331 (3): 150–3. doi:10.1097/00000441-200603000-00007. PMID 16538076.
- ↑ Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW (October 2003). "Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention". Circulation 108 (17): 2154–69. doi:10.1161/01.CIR.0000095676.90936.80. PMID 14581387.
- ↑ Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, McAlister F, Garg AX (July 2006). "Chronic kidney disease and mortality risk: a systematic review". J. Am. Soc. Nephrol. 17 (7): 2034–47. doi:10.1681/ASN.2005101085. PMID 16738019.
- ↑ Heidenheim AP, Kooistra MP, Lindsay RM (2004). "Quality of life". Contrib Nephrol. Contributions to Nephrology 145: 99–105. doi:10.1159/000081673. ISBN 3-8055-7808-3. PMID 15496796.
- ↑ de Francisco AL, Piñera C (January 2006). "Challenges and future of renal replacement therapy". Hemodial Int 10 (Suppl 1): S19–23. doi:10.1111/j.1542-4758.2006.01185.x. PMID 16441862.
- ↑ Groothoff JW (July 2005). "Long-term outcomes of children with end-stage renal disease". Pediatr. Nephrol. 20 (7): 849–53. doi:10.1007/s00467-005-1878-9. PMID 15834618.
- ↑ Giri M (2004). "Choice of renal replacement therapy in patients with diabetic end stage renal disease". Edtna Erca J 30 (3): 138–42. doi:10.1111/j.1755-6686.2004.tb00353.x. PMID 15715116.
- ↑ Pierratos A, McFarlane P, Chan CT (March 2005). "Quotidian dialysis–update 2005". Curr. Opin. Nephrol. Hypertens. 14 (2): 119–24. doi:10.1097/00041552-200503000-00006. PMID 15687837.
- 1 2 Maisonneuve P, Agodoa L, Gellert R, Stewart JH, Buccianti G, Lowenfels AB, Wolfe RA, Jones E, Disney AP, Briggs D, McCredie M, Boyle P (1999). "Cancer in patients on dialysis for end-stage renal disease: An international collaborative study". Lancet 354 (9173): 93–99. doi:10.1016/S0140-6736(99)06154-1. PMID 10408483.
- ↑ American Society of Nephrology. "Five Things Physicians and Patients Should Question" (PDF). Choosing Wisely: an initiative of the ABIM Foundation (American Society of Nephrology). Retrieved August 17, 2012
- ↑ Chertow GM, Paltiel AD, Owen WF, Lazarus JM (1996). "Cost-effectiveness of Cancer Screening in End-Stage Renal Disease". Archives of Internal Medicine 156 (12): 1345–1350. doi:10.1001/archinte.1996.00440110117016. PMID 8651845.
- ↑ "Prevalence of chronic kidney disease and associated risk factors—United States, 1999–2004". MMWR Morb. Mortal. Wkly. Rep. 56 (8): 161–5. March 2007. PMID 17332726.
- ↑ Morgan T (21 January 2009). "Chronic Kidney Disease (stages 3–5) prevalence estimates using data from the Neoerica study (2007)". Association of Public Health Observatories.
- 1 2 3 Appel LJ, Wright JT, Greene T, Kusek JW, Lewis JB, Wang X, Lipkowitz MS, Norris KC, Bakris GL, Rahman M, Contreras G, Rostand SG, Kopple JD, Gabbai FB, Schulman GI, Gassman JJ, Charleston J, Agodoa LY (April 2008). "Long-term effects of renin-angiotensin system-blocking therapy and a low blood pressure goal on progression of hypertensive chronic kidney disease in African Americans". Arch. Intern. Med. 168 (8): 832–9. doi:10.1001/archinte.168.8.832. PMID 18443258.
- 1 2 3 Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Stamler J (1997). "End-stage renal disease in African-American and white men. 16-year MRFIT findings". JAMA 277 (16): 1293–8. doi:10.1001/jama.1997.03540400043029. PMID 9109467.
- ↑ Tangri N (29 July 2013). "MesoAmerican Nephropathy: A New Entity". eAJKD. National Kidney Foundation.
- ↑ Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman DH (November 2013). "The epidemic of chronic kidney disease of unknown etiology in Mesoamerica: a call for interdisciplinary research and action". Am J Public Health 103 (11): 1927–30. doi:10.2105/AJPH.2013.301594. PMID 24028232.
- ↑ Johnson RJ, Sánchez-Lozada LG (October 2013). "Chronic kidney disease: Mesoamerican nephropathy—new clues to the cause". Nat Rev Nephrol 9 (10): 560–1. doi:10.1038/nrneph.2013.174. PMID 23999393.
- ↑ Roncal Jimenez CA, Ishimoto T, Lanaspa MA, Rivard CJ, Nakagawa T, Ejaz AA, Cicerchi C, Inaba S, Le M, Miyazaki M, Glaser J, Correa-Rotter R, González MA, Aragón A, Wesseling C, Sánchez-Lozada LG, Johnson RJ (August 2014). "Fructokinase activity mediates dehydration-induced renal injury". Kidney Int. 86 (2): 294–302. doi:10.1038/ki.2013.492. PMC 4120672. PMID 24336030.
- ↑ Chavkin, Sasha; Greene, Ronnie (12 December 2011). "Thousands of sugar cane workers die as wealthy nations stall on solutions". International Consortium of Investigative Journalists. Retrieved November 26, 2012.
- ↑ Orantes CM, Herrera R, Almaguer M, Brizuela EG, Hernández CE, Bayarre H, Amaya JC, Calero DJ, Orellana P, Colindres RM, Velázquez ME, Núñez SG, Contreras VM, Castro BE (October 2011). "Chronic kidney disease and associated risk factors in the Bajo Lempa region of El Salvador: Nefrolempa study, 2009" (PDF). MEDICC Rev 13 (4): 14–22. PMID 22143603.
External links
- National Kidney Foundation
- Dialysis Complications of Chronic Renal Failure at eMedicine
- The Kidney Foundation of Canada
- Chronic Renal Failure Information from Great Ormond Street Hospital
- Renalmed - understand renal medicine
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||
|