Primary biliary cirrhosis
| Primary biliary cirrhosis | |
|---|---|
 | |
| Classification and external resources | |
| Synonyms | Primary biliary cholangitis |
| Specialty | Gastroenterology |
| ICD-10 | K74.3 |
| ICD-9-CM | 571.6 |
| OMIM | 109720 |
| DiseasesDB | 10615 |
| MedlinePlus | 000282 |
| eMedicine | med/223 |
| Patient UK | Primary biliary cirrhosis |
| MeSH | D008105 |
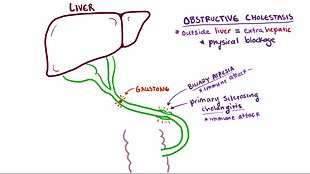
Primary biliary cirrhosis, also known as primary biliary cholangitis (PBC), is an autoimmune disease of the liver.[1][2][3] It is marked by slow progressive destruction of the small bile ducts of the liver, with the intralobular ducts and the Canals of Hering (intrahepatic ductules) affected early in the disease.[4] When these ducts are damaged, bile and other toxins build up in the liver (cholestasis) and over time damages the liver tissue in combination with ongoing immune related damage. This can lead to scarring, fibrosis and cirrhosis.
PBC is a relatively rare disease, with some studies showing that it affects up to 1 in 3–4,000 people.[5][6] The sex ratio is at least 9:1 female to male.[1]
As cirrhosis is only a feature of advanced disease, a change of name to "primary biliary cholangitis" was proposed by patient advocacy groups in 2014.[7][8] Use of the new name was advocated in the medical literature in September 2015.[9]
Signs and symptoms
People with PBC experience fatigue (80%) that leads to sleepiness during the daytime; more half of those have severe fatigue. 20–70% have itching.[10] Those with more severe disease may have jaundice (yellowing of the eyes and skin).[10] PBC impairs bone density and there is an increased risk of fracture.[10] Xanthelasma (skin lesions around the eyes) or other xanthoma may be present as a result of increased cholesterol levels.[11]
PBC can eventually progress to cirrhosis of the liver. This in turn may lead to a number of symptoms or complications:
- Fluid retention in the abdomen (ascites) in more advanced disease
- Enlarged spleen in more advanced disease
- Oesophageal varices in more advanced disease
- Hepatic encephalopathy, including coma in extreme cases in more advanced disease.
People with PBC may have the findings of an associated extrahepatic autoimmune disorder such as rheumatoid arthritis or Sjögren's syndrome (in up to 80% of cases).[11][12]
Causes
The cause of the disease is attributed to an immunological basis for the disease, making it an autoimmune disorder.[13] Most of the patients (>90%) have anti-mitochondrial antibodies (AMAs) against pyruvate dehydrogenase complex (PDC-E2), an enzyme complex that is found in the mitochondria.[1] Those 'negative' for AMAs are usually found to be positive when more sensitive methods of detection are used.[14]
Many PBC patients have a concomitant autoimmune disease, including rheumatological, endocrinological, gastrointestinal, pulmonary, or dermatological conditions, which suggests shared genetic and immune abnormalities.[12] Common associations include Sjögren's syndrome, systemic sclerosis, rheumatoid arthritis, SLE, hypothyroidism and gluten sensitive enteropathy.[12][15][16][17] In some cases of disease, protein expression may cause an immune tolerance failure, as might be the case with gp210 and p62, nuclear pore proteins. Gp210 has increased expression in the bile duct of anti-gp210 positive patients.[18] Both proteins appear to be prognostic of liver failure relative to anti-mitochondrial antibodies.
A genetic predisposition to disease has been thought important for some time, as evident by cases of PBC in family members, concordance in identical twins, and clustering of autoimmune diseases.[13] In 2009, a Canadian-led group of investigators reported in the New England Journal of Medicine results from the first PBC genome-wide association study.[19][20] This research revealed parts of the IL12 signaling cascade, particularly IL12A and IL12RB2 polymorphisms, to be important in the etiology of the disease in addition to the HLA region. In 2012, two independent PBC association studies increased the total number of genomic regions associated to 26, implicating many genes involved in cytokine regulation such as TYK2, SH2B3 and TNFSF11.[21][22]
In 2003 it was reported that an environmental Gram negative alphabacterium — Novosphingobium aromaticivorans[23] was strongly associated with this disease. Subsequent reports appear to have confirmed this finding suggesting an aetiological role for this organism.[24][25][26] The mechanism appears to be a cross reaction between the proteins of the bacterium and the mitochondrial proteins of the liver cells.[27] The gene encoding CD101 may also play a role in host susceptibility to this disease.[28]
Diagnosis
To diagnose PBC, it needs to be distinguished from other conditions with similar symptoms, such as autoimmune hepatitis or primary sclerosing cholangitis (PSC).
- Abnormalities in liver enzyme tests are usually present and elevated gamma-glutamyl transferase and alkaline phosphatase are found in early disease.[11] Elevations in bilirubin occur in advanced disease.
- Antimitochondrial antibodies (AMA) are the characteristic serological marker for PBC, being found in 90%-95% of patients and only 1% of controls. PBC patients have AMA against pyruvate dehydrogenase complex (PDC-E2), an enzyme complex that is found in the mitochondria.[11] Those people who are AMA negative but with disease similar to PBC have been found to have AMAs when more sensitive detection methods are employed.[29]
- Other auto-antibodies may be present:
- Antinuclear antibody (ANA) are not diagnostic (as they are not specific) but are have a role in prognosis.
- Anti-glycoprotein-210 antibodies, and to a lesser degree anti-p62 antibodies, correlate with the disease's progression toward end stage liver failure. Anti-gp210 antibodies are found in 47% of PBC patients.[30][31]
- Anti-centromere antibodies often correlate with developing portal hypertension.[32]
- Anti-np62[33] and anti-sp100 are also found in association with PBC.
- Abdominal ultrasound, MR scanning (MRCP) or a CT scan is usually performed to rule out blockage to the bile ducts. Most suspected cases have a liver biopsy performed, and if uncertainty remains as in some patients, an endoscopic retrograde cholangiopancreatography or ERCP, where an endoscopic investigation of the bile duct is performed.
Most patients can be diagnosed without invasive investigation, as the combination of anti-mitochondrial antibodies and typical (cholestatic) liver enzyme tests are considered diagnostic. However, a liver biopsy is needed to determine the stage of disease.
-

Low magnification micrograph of PBC. H&E stain.
-

Intermediate magnification micrograph of PBC showing bile duct inflammation and periductal granulomas. Liver biopsy. H&E stain.
-
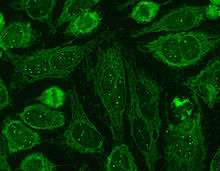
Immunofluorescence staining pattern of sp100 antibodies (nuclear dots) and AMA.
Biopsy
PBC is characterized by interlobular bile duct destruction. Histopathologic findings of primary biliary cholangitis include the following:[34]
- Inflammation of the bile ducts, characterized by intraepithelial lymphocytes, and
- Periductal epithelioid granulomata.
Stages
- Stage 1 — Portal Stage: Normal sized triads; portal inflammation, subtle bile duct damage. Granulomas are often detected in this stage.
- Stage 2 — Periportal Stage: Enlarged triads; periportal fibrosis and/or inflammation. Typically characterized by the finding of a proliferation of small bile ducts.
- Stage 3 — Septal Stage: Active and/or passive fibrous septa.
- Stage 4 — Biliary Cirrhosis: Nodules present; garland or jigsaw puzzle pattern.
Treatment
There is no known cure, but medication may slow the progression so that a normal lifespan and quality of life may be attainable for many patients.[11][35][36]
- Ursodeoxycholic acid (Ursodiol) is the most frequently used treatment. This helps reduce the cholestasis and improves blood test results (liver function tests). It has a minimal effect on symptoms and whether it improves prognosis is controversial.[37][11]
- To relieve itching caused by bile acids in circulation, which would normally be removed by the liver, cholestyramine (a bile acid sequestrant) may be prescribed to absorb bile acids in the gut and be eliminated, rather than re-enter the blood stream. Alternative agents include stanozolol, naltrexone and rifampicin.[35][36][38]
- Specific treatment for fatigue, which may be debilitating in some patients, is limited and undergoing trials.[39] Some studies indicate that Provigil (modafinil) may be effective without damaging the liver.[40] Though off-patent, the limiting factor in the use of modafinil in the U.S. is cost. The manufacturer, Cephalon, has made agreements with manufacturers of generic modafinil to provide payments in exchange for delaying their sale of modafinil.[41] The FTC has filed suit against Cephalon alleging anti-competitive behavior.[42]
- Patients with PBC have poor lipid-dependent absorption of Vitamins A, D, E, K.[43] Appropriate supplementation is recommended when bilirubin is elevated.[11]
- Patients with PBC are at elevated risk of developing osteoporosis[44] and esophageal varices[45] as compared to the general population and others with liver disease. Screening and treatment of these complications is an important part of the management of PBC.
As in all liver diseases, consumption of alcohol is contraindicated.
In advanced cases, a liver transplant, if successful, results in a favorable prognosis.[46][47]
The farnesoid X receptor agonist, obeticholic acid, which is a modified bile acid, is in phase III clinical trials for PBC.[48]
Epidemiology
PBC is a chronic autoimmune liver disease with a female gender predominance with female:male ratio is at least 9:1 and a peak incidence in the fifth decade of life.[1][49] In some areas of the US and UK the prevalence is estimated to be as high as 1 in 4000. This is much more common than in South America or Africa, which may be due to better recognition in the US and UK.[5][6] First-degree relatives may have as much as a 500 times increase in prevalence, but there is debate if this risk is greater in the same generation relatives or the one that follows.
Prognosis
The serum bilirubin level is an indicator of the prognosis of PBC, with levels of 2–6 mg/dL having a mean survival time of 4.1 years, 6–10 mg/dL having 2.1 years and those above 10 mg/dL having a mean survival time of 1.4 years.[50]
After liver transplant, the recurrence rate may be as high as 18% at 5 years, and up to 30% at 10 years. There is no consensus on risk factors for recurrence of the disease.[51]
Patients with PBC have an increased risk of hepatocellular carcinoma compared to the general population, as is found in other cirrhotic patients. In patients with advanced disease, one series found an incidence of 20% in men and 4% in women.[52]
History
Addison and Gull in 1851 described the clinical picture of progressive obstructive jaundice in the absence of mechanical obstruction of the large bile ducts. Ahrens et al in 1950 coined the term primary biliary cirrhosis for this disease. The association with anti-mitochondrial antibodies was first reported in 1965[53] and their presence was recognized as a marker of early, pre-cirrhotic disease.[54]
Society and culture
Support groups
PBC Foundation
The PBC Foundation is a UK-based international charity offering support and information to people with PBC, their families and friends.[55] It campaigns for increasing recognition of the disorder, improved diagnosis and treatments, and estimates over 8000 people are undiagnosed in the UK.[56][57] The Foundation has supported research into PBC including the development of the PBC-40 quality of life measure published in 2004[58] and helped establish the PBC Genetics Study.[59][21] It was founded by Collette Thain in 1996, after she was diagnosed with the condition.[56] Thain was awarded an MBE Order of the British Empire in 2004 for her work with the Foundation.[60] The PBC Foundation helped initiate the name change campaign in 2014.[7][8][61]
PBCers
The PBCers is a US-based patient support group that was founded in 1996 and advocates for greater awareness of the disease and new treatments.[62] It has supported the initiative for a change in name.[8]
Name
In 2014 the PBC Foundation, with the support of the PBCers, the PBC Society (Canada)[63] and other patient groups, advocated a change in name from "primary biliary cirrhosis" to "primary biliary cholangitis", citing that most PBC patients did not have cirrhosis and that this often had negative connotations of alcoholism.[7][8][64] Patient and professional groups were canvassed.[65] Support for this name change came from professional bodies including the American Association for the Study of Liver Diseases[66] and the European Association for the Study of the Liver.[67] Advocates for the name change published calls to adopt the new name in multiple hepatology journals in the fall of 2015.[65][9][67][68]
References
- 1 2 3 4 Poupon R (2010). "Primary biliary cirrhosis: a 2010 update". J. Hepatol. 52 (5): 745–58. doi:10.1016/j.jhep.2009.11.027. PMID 20347176.
- ↑ Hirschfield GM, Gershwin ME (Jan 2013). "The immunobiology and pathophysiology of primary biliary cirrhosis". Annual Review of Pathology 8: 303–30. doi:10.1146/annurev-pathol-020712-164014. PMID 23347352.
- ↑ Dancygier, Henryk (2010). Clinical Hepatology Principles and Practice of. Springer. pp. 895–. ISBN 978-3-642-04509-7. Retrieved 29 June 2010.
- ↑ Saxena R, Theise N (Feb 2004). "Canals of Hering: recent insights and current knowledge". Seminars in Liver Disease 24 (1): 43–8. doi:10.1055/s-2004-823100. PMID 15085485.
- 1 2 Boonstra K, Beuers U, Ponsioen CY (2012). "Epidemiology of primary sclerosing cholangitis and primary biliary cirrhosis: a systematic review". J. Hepatol. 56 (5): 1181–8. doi:10.1016/j.jhep.2011.10.025. PMID 22245904.
- 1 2 James OF, Bhopal R, Howel D, Gray J, Burt AD, Metcalf JV (1999). "Primary biliary cirrhosis once rare, now common in the United Kingdom?". Hepatology 30 (2): 390–4. doi:10.1002/hep.510300213. PMID 10421645.
- 1 2 3 PBC Foundation (UK). "PBC Name Change Press Release". Retrieved 8 July 2015.
- 1 2 3 4 PBCers Organization. "Primary Biliary Cirrhosis Name Change Initiative" (PDF).
- 1 2 Beuers U, Gershwin ME, Gish RG, Invernizzi P, Jones DE, Lindor K, Ma X, Mackay IR, Parés A, Tanaka A, Vierling JM, Poupon R (2015). "Changing nomenclature for PBC: From 'cirrhosis' to 'cholangitis'". Hepatology. doi:10.1002/hep.28140. PMID 26372460.
- 1 2 3 Selmi C, Bowlus CL, Gershwin LE, Coppel RL (7 May 2011). "Primary biliary cirrhosis". Lancet 377: 1600–1609. doi:10.1016/S0140-6736(10)61965-4. PMID 21529926.
- 1 2 3 4 5 6 7 Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ (Jul 2009). "Primary biliary cirrhosis". Hepatology 50 (1): 291–308. doi:10.1002/hep.22906. PMID 19554543.
The AASLD Practice Guideline
- 1 2 3 Floreani A, Franceschet I, Cazzagon N (Aug 2014). "Primary biliary cirrhosis: overlaps with other autoimmune disorders". Seminars in Liver Disease 34 (3): 352–60. doi:10.1055/s-0034-1383734. PMID 25057958.
- 1 2 Webb GJ, Siminovitch KA, Hirschfield GM (2015). "The immunogenetics of primary biliary cirrhosis: A comprehensive review.". J Autoimmun. doi:10.1016/j.jaut.2015.07.004. PMID 26250073.
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/15062200
- ↑ Watt FE, James OF, Jones DE (Jul 2004). "Patterns of autoimmunity in primary biliary cirrhosis patients and their families: a population-based cohort study". Qjm 97 (7): 397–406. doi:10.1093/qjmed/hch078. PMID 15208427.
- ↑ Logan RF, Ferguson A, Finlayson ND, Weir DG (Feb 1978). "Primary biliary cirrhosis and coeliac disease: an association?". Lancet 1 (8058): 230–3. doi:10.1016/S0140-6736(78)90480-4. PMID 74661.
- ↑ Volta U, Rodrigo L, Granito A, Petrolini N, Muratori P, Muratori L, et al. (Oct 2002). "Celiac disease in autoimmune cholestatic liver disorders". The American Journal of Gastroenterology 97 (10): 2609–13. doi:10.1111/j.1572-0241.2002.06031.x. PMID 12385447.
- ↑ Nakamura M, Takii Y, Ito M, Komori A, Yokoyama T, Shimizu-Yoshida Y, et al. (Mar 2006). "Increased expression of nuclear envelope gp210 antigen in small bile ducts in primary biliary cirrhosis". Journal of Autoimmunity 26 (2): 138–45. doi:10.1016/j.jaut.2005.10.007. PMID 16337775.
- ↑ Hirschfield GM, Liu X, Xu C, Lu Y, Xie G, Lu Y, et al. (Jun 2009). "Primary biliary cirrhosis associated with HLA, IL12A, and IL12RB2 variants". The New England Journal of Medicine 360 (24): 2544–55. doi:10.1056/NEJMoa0810440. PMC 2857316. PMID 19458352.
- ↑ http://www.uk-pbc.com
- 1 2 Liu JZ, Almarri MA, Gaffney DJ, Mells GF, Jostins L, Cordell HJ, et al. (Oct 2012). "Dense fine-mapping study identifies new susceptibility loci for primary biliary cirrhosis". Nature Genetics 44 (10): 1137–41. doi:10.1038/ng.2395. PMC 3459817. PMID 22961000.
- ↑ Juran BD, Hirschfield GM, Invernizzi P, Atkinson EJ, Li Y, Xie G, et al. (Dec 2012). "Immunochip analyses identify a novel risk locus for primary biliary cirrhosis at 13q14, multiple independent associations at four established risk loci and epistasis between 1p31 and 7q32 risk variants". Human Molecular Genetics 21 (23): 5209–21. doi:10.1093/hmg/dds359. PMC 3490520. PMID 22936693.
- ↑ Selmi C, Balkwill DL, Invernizzi P, Ansari AA, Coppel RL, Podda M, et al. (Nov 2003). "Patients with primary biliary cirrhosis react against a ubiquitous xenobiotic-metabolizing bacterium". Hepatology 38 (5): 1250–7. doi:10.1053/jhep.2003.50446. PMID 14578864.
- ↑ Mohammed JP, Mattner J (Jul 2009). "Autoimmune disease triggered by infection with alphaproteobacteria". Expert Review of Clinical Immunology 5 (4): 369–379. doi:10.1586/ECI.09.23. PMC 2742979. PMID 20161124.
- ↑ Kaplan MM (Nov 2004). "Novosphingobium aromaticivorans: a potential initiator of primary biliary cirrhosis". The American Journal of Gastroenterology 99 (11): 2147–9. doi:10.1111/j.1572-0241.2004.41121.x. PMID 15554995.
- ↑ Selmi C, Gershwin ME (Jul 2004). "Bacteria and human autoimmunity: the case of primary biliary cirrhosis". Current Opinion in Rheumatology 16 (4): 406–10. doi:10.1097/01.bor.0000130538.76808.c2. PMID 15201604.
- ↑ Mattner J, Savage PB, Leung P, Oertelt SS, Wang V, Trivedi O, et al. (May 2008). "Liver autoimmunity triggered by microbial activation of natural killer T cells". Cell Host & Microbe 3 (5): 304–15. doi:10.1016/j.chom.2008.03.009. PMC 2453520. PMID 18474357.
- ↑ Mohammed JP, Fusakio ME, Rainbow DB, Moule C, Fraser HI, Clark J, et al. (Jul 2011). "Identification of Cd101 as a susceptibility gene for Novosphingobium aromaticivorans-induced liver autoimmunity". Journal of Immunology 187 (1): 337–49. doi:10.4049/jimmunol.1003525. PMC 3134939. PMID 21613619.
- ↑ Vierling, JM (February 2004). "Primary biliary cirrhosis and autoimmune cholangiopathy.". Clinics in liver disease 8 (1): 177–94. PMID 15062200.
- ↑ Nickowitz RE, Worman HJ (1993). "Autoantibodies from patients with primary biliary cirrhosis recognize a restricted region within the cytoplasmic tail of nuclear pore membrane glycoprotein Gp210". J. Exp. Med. 178 (6): 2237–42. doi:10.1084/jem.178.6.2237. PMC 2191303. PMID 7504063.
- ↑ Bauer A, Habior A (2007). "Measurement of gp210 autoantibodies in sera of patients with primary biliary cirrhosis". J. Clin. Lab. Anal. 21 (4): 227–31. doi:10.1002/jcla.20170. PMID 17621358.
- ↑ Nakamura M, Kondo H, Mori T, Komori A, Matsuyama M, Ito M, et al. (Jan 2007). "Anti-gp210 and anti-centromere antibodies are different risk factors for the progression of primary biliary cirrhosis". Hepatology 45 (1): 118–27. doi:10.1002/hep.21472. PMID 17187436.
- ↑ Nesher G, Margalit R, Ashkenazi YJ (Apr 2001). "Anti-nuclear envelope antibodies: Clinical associations". Seminars in Arthritis and Rheumatism 30 (5): 313–20. doi:10.1053/sarh.2001.20266. PMID 11303304.
- ↑ Nakanuma Y, Tsuneyama K, Sasaki M, Harada K (Aug 2000). "Destruction of bile ducts in primary biliary cirrhosis". Baillière's Best Practice & Research. Clinical Gastroenterology 14 (4): 549–70. doi:10.1053/bega.2000.0103. PMID 10976014.
- 1 2 Levy C, Lindor KD (Apr 2003). "Treatment Options for Primary Biliary Cirrhosis and Primary Sclerosing Cholangitis". Current Treatment Options in Gastroenterology 6 (2): 93–103. doi:10.1007/s11938-003-0010-0. PMID 12628068.
- 1 2 Oo YH, Neuberger J (2004). "Options for treatment of primary biliary cirrhosis". Drugs 64 (20): 2261–71. doi:10.2165/00003495-200464200-00001. PMID 15456326.
- ↑ Gluud C, Christensen E (2002). "Ursodeoxycholic acid for primary biliary cirrhosis". The Cochrane Database of Systematic Reviews (1): CD000551. doi:10.1002/14651858.CD000551. PMID 11869580.
- ↑ Walt RP, Daneshmend TK, Fellows IW, Toghill PJ (Feb 1988). "Effect of stanozolol on itching in primary biliary cirrhosis". British Medical Journal 296 (6622): 607. doi:10.1136/bmj.296.6622.607. PMC 2545238. PMID 3126923.
- ↑ Abbas G, Jorgensen RA, Lindor KD (Jun 2010). "Fatigue in primary biliary cirrhosis". Nature Reviews. Gastroenterology & Hepatology 7 (6): 313–9. doi:10.1038/nrgastro.2010.62. PMID 20458334.
- ↑ Modafinil#Primary biliary cirrhosis
Ian Gan S, de Jongh M, Kaplan MM (Oct 2009). "Modafinil in the treatment of debilitating fatigue in primary biliary cirrhosis: a clinical experience". Digestive Diseases and Sciences 54 (10): 2242–6. doi:10.1007/s10620-008-0613-3. PMID 19082890.
Kumagi T, Heathcote EJ (2008). "Primary biliary cirrhosis". Orphanet Journal of Rare Diseases 3: 1. doi:10.1186/1750-1172-3-1. PMC 2266722. PMID 18215315.Ref 157 viz:
Jones DE, Newton JL (Feb 2007). "An open study of modafinil for the treatment of daytime somnolence and fatigue in primary biliary cirrhosis". Alimentary Pharmacology & Therapeutics 25 (4): 471–6. doi:10.1111/j.1365-2036.2006.03223.x. PMID 17270003. - ↑ Modafinil#Patent protection and antitrust litigation
Carrier MA (2011). "Provigil: A Case Study of Anticompetitive Behavior" (PDF). Hastings Science & Technology Law Journal 3 (2): 441–452. - ↑ "Cephalon, Inc." (PDF). Federal Trade Commission.
- ↑ Bacon BR, O'Grady JG (2006). Comprehensive clinical hepatology. Elsevier Health Sciences. pp. 283–. ISBN 978-0-323-03675-7. Retrieved 29 June 2010.
- ↑ Collier JD, Ninkovic M, Compston JE (Feb 2002). "Guidelines on the management of osteoporosis associated with chronic liver disease". Gut. 50 Suppl 1 (Suppl 1): i1–9. doi:10.1136/gut.50.suppl_1.i1. PMC 1867644. PMID 11788576.
- ↑ Ali AH, Sinakos E, Silveira MG, Jorgensen RA, Angulo P, Lindor KD (Aug 2011). "Varices in early histological stage primary biliary cirrhosis". Journal of Clinical Gastroenterology 45 (7): e66–71. doi:10.1097/MCG.0b013e3181f18c4e. PMID 20856137.
- ↑ Clavien PA, Killenberg PG (2006). Medical Care of the Liver Transplant Patient: Total Pre-, Intra- and Post-Operative Management. Wiley-Blackwell. p. 155. ISBN 1-4051-3032-6.
- ↑ Kaneko J, Sugawara Y, Tamura S, Aoki T, Hasegawa K, Yamashiki N, et al. (Jan 2012). "Long-term outcome of living donor liver transplantation for primary biliary cirrhosis". Transplant International 25 (1): 7–12. doi:10.1111/j.1432-2277.2011.01336.x. PMID 21923804.
- ↑ Ali AH, Carey EJ, Lindor KD (Jan 2015). "Recent advances in the development of farnesoid X receptor agonists". Annals of Translational Medicine 3 (1): 5. doi:10.3978/j.issn.2305-5839.2014.12.06. PMC 4293481. PMID 25705637.
- ↑ Weinmann A, Sattler T, Unold HP, Grambihler A, Teufel A, Koch S, et al. (2014). "Predictive scores in primary biliary cirrhosis: a retrospective single center analysis of 204 patients". Journal of Clinical Gastroenterology 49 (5): 438–47. doi:10.1097/MCG.0000000000000176. PMID 25014239.
- ↑ Primary Biliary Cirrhosis~followup at eMedicine
- ↑ Clavien & Killenberg 2006, p. 429
- ↑ Jones DE, Metcalf JV, Collier JD, Bassendine MF, James OF (Nov 1997). "Hepatocellular carcinoma in primary biliary cirrhosis and its impact on outcomes". Hepatology 26 (5): 1138–42. doi:10.1002/hep.510260508. PMID 9362353.
- ↑ Walker JG, Doniach D, Roitt IM, Sherlock S (Apr 1965). "Serological tests in diagnosis of primary biliary cirrhosis". Lancet 1 (7390): 827–31. doi:10.1016/s0140-6736(65)91372-3. PMID 14263538.
- ↑ Mitchison HC, Bassendine MF, Hendrick A, Bennett MK, Bird G, Watson AJ, et al. (1986). "Positive antimitochondrial antibody but normal alkaline phosphatase: is this primary biliary cirrhosis?". Hepatology 6 (6): 1279–84. doi:10.1002/hep.1840060609. PMID 3793004.
- ↑ Association of Medical Research Charities. "The PBC Foundation". Retrieved 12 July 2015.
- 1 2 Staff of The Scotsman, January 3, 2008. Dealing with a silent killer
- ↑ Thain, Collette (2015). "Primary biliary cirrhosis: getting a diagnosis" (online). At Home Magazine. Retrieved 28 July 2015.
- ↑ Jacoby A, Rannard A, Buck D, Bhala N, Newton JL, James OF, Jones DE (Nov 2005). "Development, validation, and evaluation of the PBC-40, a disease specific health related quality of life measure for primary biliary cirrhosis". Gut 54 (11): 1622–9. doi:10.1136/gut.2005.065862. PMC 1774759. PMID 15961522.
- ↑ Mells GF, Floyd JA, Morley KI, Cordell HJ, Franklin CS, Shin SY, et al. (Apr 2011). "Genome-wide association study identifies 12 new susceptibility loci for primary biliary cirrhosis". Nature Genetics 43 (4): 329–32. doi:10.1038/ng.789. PMC 3071550. PMID 21399635.
- ↑ Barry Gordon for The Scotsman. 31 December 2003 A royal seal of approval
- ↑ PBC Foundation. "EASL Name Change Presentation". Retrieved 8 July 2015.
- ↑ Kim, Margot. "New hope for PBC liver disease". ABC30 Action news. Retrieved 4 August 2015.
- ↑ Cheung AC, Montano-Loza A, Swain M, Vincent C, Renner E, Sherman M, Janssen H, Mason AL (2015). "Time to make the change from 'primary biliary cirrhosis' to 'primary biliary cholangitis'". Can J Gastroenterol Hepatol 29 (6): 293. PMID 26196152.
- ↑ PBC Foundation. "EASL Name Change Presentation". Retrieved 8 July 2015.
- 1 2 Beuers U, Gershwin ME, Gish RG, Invernizzi P, Jones DE, Lindor K, Ma X, Mackay IR, Parés A, Tanaka A, Vierling JM, Poupon R (2015). "Changing nomenclature for PBC: from 'cirrhosis' to 'cholangitis'". Gut. doi:10.1136/gutjnl-2015-310593. PMID 26374822.
- ↑ AASLD. "A name change for PBC: cholangitis replacing cirrhosis". Retrieved 6 July 2015.
- 1 2 Beuers U, Gershwin ME, Gish RG, Invernizzi P, Jones DE, Lindor K, Ma X, Mackay IR, Parés A, Tanaka A, Vierling JM, Poupon R (2015). "Changing nomenclature for PBC: From 'cirrhosis' to 'cholangitis'". J. Hepatol. doi:10.1016/j.jhep.2015.06.031. PMID 26385765.
- ↑ Beuers U, Gershwin ME, Gish RG, Invernizzi P, Jones DE, Lindor K, Ma X, Mackay IR, Parés A, Tanaka A, Vierling JM, Poupon R (2015). "Changing Nomenclature for PBC: From 'Cirrhosis' to 'Cholangitis'". Gastroenterology. doi:10.1053/j.gastro.2015.08.031. PMID 26385706.