Testicular torsion
| Testicular torsion | |
|---|---|
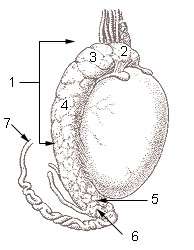 1. Epididymis 2. Head of epididymis 3. Lobules of epididymis 4. Body of epididymis 5. Tail of epididymis 6. Duct of epididymis 7. Deferent duct (ductus deferens or vas deferens) | |
| Classification and external resources | |
| Specialty | Urology |
| ICD-10 | N44 |
| ICD-9-CM | 608.2 |
| OMIM | 187400 |
| DiseasesDB | 12984 |
| MedlinePlus | 000517 |
| eMedicine | med/2780 |
| MeSH | D013086 |
Testicular torsion occurs when the spermatic cord (from which the testicle is suspended) twists, cutting off the testicle's blood supply, a condition called ischemia. The principal symptom is rapid onset of testicular pain. The most common underlying cause is a congenital malformation known as a "bell-clapper deformity" wherein the testis is inadequately affixed to the scrotum allowing it to move freely on its axis and susceptible to induced twisting of the cord and its vessels.
The diagnosis should usually be made on the presenting signs and symptoms[1] and an urgent ultrasound should only be done when the diagnosis is unclear.[1] Irreversible ischemia begins around six hours after onset and emergency diagnosis and treatment is required within this time to minimize the risk of testicle loss.
It is most common just after birth and during puberty.[1] It occurs in about 1 in 4,000 to 1 per 25,000 males per year before 25 years of age.[2][3][1]
Signs and symptoms
Testicular torsion usually presents with sudden, severe, testicular pain (in groin & lower abdomen) and tenderness.[1] There is often associated nausea and vomiting.[1] The testis may be higher than its normal position. Mild pyrexia and redness of overlying area may be found.
Some of the symptoms are similar to epididymitis though epididymitis may be characterized by discoloration and swelling of the testis, often with fever, while the cremasteric reflex is usually present. Testicular torsion, or more probably impending testicular infarction, can also produce a low-grade fever.[4] There is often an absent or decreased cremasteric reflex.[1]
Risk factors
A larger testicle either due to normal variation or a tumor increases the risk of torsion.[2]
Congenital
Conditions that allow the testicle to rotate predispose to torsion.[2] A congenital malformation of the processus vaginalis known as the "bell-clapper deformity" accounts for 90% of all cases.[3] In this condition, rather than the testes attaching posteriorly to the inner lining of the scrotum by the mesorchium, the mesorchium terminates early and the testis is free floating in the tunica vaginalis.
Diagnosis
The diagnosis should be made on the history and presenting signs and symptoms.[1] With a convincing history and physical exam immediate surgery is recommended[1][2] and doppler ultrasound should only be obtained in low suspicion cases to rule out torsion.[2]
Clinical exam
Prehn's sign, a classic physical exam finding, has not been reliable in distinguishing torsion from other causes of testicular pain such as epididymitis.[5] In cases of true torsion the cremasteric reflex is typically absent (the twisted cords of the testicle make reflexive responses all but impossible). On physical examination, the testis will be swollen, tender, and high-riding, with an abnormal transverse lie.[6] The individual will not usually have a fever, though nausea is common.
Imaging
A doppler ultrasound scan of the scrotum is nearly 90% accurate in diagnosis[1][2] identifying the absence of blood flow in the twisted testicle, which distinguishes torsion from epididymitis.[7]
Radionuclide scanning of the scrotum is the most accurate, imaging technique, but it is not routinely available, particularly with the urgency that might be required.[8] The agent of choice for this purpose is technetium-99m pertechnetate.[9] Initially it provides a radionuclide angiogram, followed by a static image after the radionuclide has perfused the tissue. In the healthy patient, initial images show symmetric flow to the testes, and delayed images show uniformly symmetric activity.[9]
Pathophysiology
Torsion is due to a mechanical twisting process. It is also believed that torsion occurring during fetal development can lead to so-called neonatal torsion or vanishing testis, and is one of the causes of an infant being born with monorchism (one testicle).[10]
Intermittent testicular torsion
A variant is a less serious but chronic condition called intermittent testicular torsion (ITT), characterized by the symptoms of torsion but followed by eventual spontaneous detortion and resolution of pain. Nausea or vomiting may also occur.[11]:p.150 Though less pressing, such individuals are at significant risk of complete torsion and possible subsequent orchiectomy and the recommended treatment is elective bilateral orchiopexy. Ninety-seven percent of patients who undergo such surgery experience complete relief from their symptoms.[4]:p.316
Extravaginal testicular torsion
A torsion which occurs outside of the tunica vaginalis, when the testis and gubernaculum can rotate freely, is termed an extravaginal testicular torsion. This type occurs exclusively in newborns. Neonates experiencing such a torsion present with scrotal swelling, discoloration, and a firm, painless mass in the scrotum. Such testes are usually necrotic from birth and must be removed surgically.[4]:p.315
Torsion of the testicular appendix
This type of torsion is the most common cause of acute scrotal pain in boys ages 7–14. Its appearance is similar to that of testicular torsion but the onset of pain is more gradual. Palpation reveals a small firm nodule on the upper portion of the testis which displays a characteristic "blue dot sign." This is the appendix of the testis which has become discolored and is noticeably blue through the skin. Unlike other torsions, however, the cremasteric reflex is still active. Typical treatment involves the use of over-the-counter analgesics and the condition resolves within 2–3 days.[4]:p.316
Treatment
With prompt diagnosis and treatment the testicle can often be saved.[2] Typically, when a torsion takes place, the surface of the testicle has rotated towards the midline of the body. Non-surgical correction can sometimes be accomplished by manually rotating the testicle in the opposite direction (i.e., outward, towards the thigh); if this is initially unsuccessful, a forced manual rotation in the other direction may correct the problem.[11]:p.149 The success rate of manual detorsion is not known with confidence.
Testicular torsion is a surgical emergency that requires immediate intervention to restore the flow of blood.[2] If treated either manually or surgically within six hours, there is a high chance (approx. 90%) of saving the testicle. At 12 hours the rate decreases to 50%; at 24 hours it drops to 10%, and after 24 hours the ability to save the testicle approaches 0.[2] About 40% of cases result in loss of the testicle.[1] Common treatment for children is surgically sewing the testicle to the scrotum to prevent future recurrence (orchiopexy).
Epidemiology
Torsion is most frequent among adolescents with about 65% of cases presenting between 12 – 18 years of age.[12] It occurs in about 1 in 4,000 to 1 per 25,000 males per year before 25 years of age;[2][3][1] but it can occur at any age, including infancy.[11]:p.149
Complication
- Testicular infarction
- Scrotal abscess
- Gangrene of testis
- Recurrence
- Chronic epididymitis
See also
- Ovarian torsion - equivalent condition of the female reproductive system.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 Sharp, VJ; Kieran, K; Arlen, AM (Dec 15, 2013). "Testicular torsion: diagnosis, evaluation, and management.". American family physician 88 (12): 835–40. PMID 24364548.
- 1 2 3 4 5 6 7 8 9 10 Wampler SM, Llanes M (September 2010). "Common scrotal and testicular problems". Prim. Care 37 (3): 613–26, x. doi:10.1016/j.pop.2010.04.009. PMID 20705202.
- 1 2 3 Ringdahl E, Teague L (November 2006). "Testicular torsion". Am Fam Physician 74 (10): 1739–43. PMID 17137004.
- 1 2 3 4 Kavoussi, Parviz K.; Costabile, Raymond A. (2011). "Disorders of scrotal contents: orchitis, epididimytis, testicular tortion, tortion of the appendages, and Fournier's gangrene". In Chapple, Christopher R.; Steers, William D. Practical urology: essential principles and practice. London: Springer-Verlag. ISBN 978-1-84882-033-3.
- ↑ Lavallee ME, Cash J (April 2005). "Testicular torsion: evaluation and management". Curr Sports Med Rep 4 (2): 102–4. doi:10.1097/01.CSMR.0000306081.13064.a2. PMID 15763047.
- ↑ Liu DR. Chapter 127. Urologic and Gynecologic Problems and Procedures in Children. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD, eds. Tintinalli's Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York: McGraw-Hill; 2011.
- ↑ Arce J, Cortés M, Vargas J (2002). "Sonographic diagnosis of acute spermatic cord torsion. Rotation of the cord: a key to the diagnosis". Pediatr Radiol 32 (7): 485–91. doi:10.1007/s00247-002-0701-z. PMID 12107581.
- ↑ Sexually Transmitted Diseases Treatment Guidelines, 2010 from Centers for Disease Control and Prevention, Recommendations and Reports. December 17, 2010 / Vol. 59 / No. RR-12
- 1 2 Medscape > Testicular Torsion Imaging by David Paushter. Updated: May 25, 2011
- ↑ Callewaert PRH, Kerrebroeck PV (June 2010). "New insights into perinatal testicular torsion". Eur J Pediatr 169 (6): 705–12. doi:10.1007/s00431-009-1096-8. PMC 2859224. PMID 19856186.
- 1 2 3 Uribe, Juan F. (1 January 2008). Potts, Jeannette M., ed. Genitourinary Pain and Inflammation: Diagnosis and Management. Totowa, New Jersey: Humana. pp. 149–. ISBN 978-1-60327-126-4. Retrieved 8 July 2013.
- ↑ Edelsberg JS, Surh YS (August 1988). "The acute scrotum". Emerg. Med. Clin. North Am. 6 (3): 521–46. PMID 3292226.
External links
- Photos of swollen, excised, and detorsed testicles of patient who sought treatment within four hours of onset of pain.
| ||||||||||||||||||||||||||||||