Assisted reproductive technology
| Assisted reproductive technology | |
|---|---|
| Intervention | |
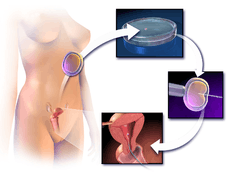 Illustration depicting intracytoplasmic sperm injection (ICSI), an example of assisted reproductive technology. | |
| MeSH | D027724 |
Assisted reproductive technology (ART) is the technology used to achieve pregnancy in procedures such as fertility medication, artificial insemination, in vitro fertilization and surrogacy. It is reproductive technology used primarily for infertility treatments, and is also known as fertility treatment. It mainly belongs to the field of reproductive endocrinology and infertility, and may also include intracytoplasmic sperm injection (ICSI) and cryopreservation. Some forms of ART are also used with regard to fertile couples for genetic reasons (preimplantation genetic diagnosis). ART is also used for couples who are discordant for certain communicable diseases; for example, AIDS to reduce the risk of infection when a pregnancy is desired.
Procedures
General
With ART, the process of sexual intercourse is bypassed either by artificial insemination or fertilization of the oocytes in the laboratory environment (i.e., in vitro fertilization). The Centers for Disease Control and Prevention (CDC)—which is required as a result of the 1992 Fertility Clinic Success Rate and Certification Act to publish the annual ART success rates at U.S. fertility clinics—defines ART to include "all fertility treatments in which both eggs and sperm are handled. In general, ART procedures involve surgically removing eggs from a woman's ovaries, combining them with sperm in the laboratory, and returning them to the woman's body or donating them to another woman." According to CDC, "they do not include treatments in which only sperm are handled (i.e., intrauterine—or artificial—insemination) or procedures in which a woman takes medicine only to stimulate egg production without the intention of having eggs retrieved."
Procedures are mainly fertility medication, as well as ART techniques that use more substantial and forceful interventions, of which in vitro fertilization (IVF) and expansions of it (e.g. OCR, AZH, ICSI, ZIFT) are the most prevalent. However, there are also other manual ART, not necessarily dependent on IVF (e.g. PGD, GIFT, SSR).
Fertility medication
Most fertility medications are agents that stimulate the development of follicles in the ovary. Examples are gonadotropins and gonadotropin releasing hormone.
Artificial insemination
Artificial insemination involves sperm being placed into a female's uterus (intrauterine) or cervix (intracervical) using artificial means rather than by sexual intercourse. This can be a very low-tech process, performed at home by the woman alone or with her partner.[1]
Conception devices, such as a conception cap may be used to aid conception by enhancing the natural process. Conception caps are used by placing semen into a small conception cap, then placing the cap onto the cervix. This holds the semen at the cervical os, protecting the semen from the acidic vaginal secretions and keeping it in contact with the cervical mucus.
Sperm donors may be used where the woman does not have a male partner with functional sperm.
In vitro fertilization
In vitro fertilization is the technique of letting fertilization of the male and female gametes (sperm and egg) occur outside the female body.
Techniques usually used in in vitro fertilization include:
- Transvaginal ovum retrieval (OCR) is the process whereby a small needle is inserted through the back of the vagina and guided via ultrasound into the ovarian follicles to collect the fluid that contains the eggs.
- Embryo transfer is the step in the process whereby one or several embryos are placed into the uterus of the female with the intent to establish a pregnancy.
Less commonly used techniques in in vitro fertilization are:
- Assisted zona hatching (AZH) is performed shortly before the embryo is transferred to the uterus. A small opening is made in the outer layer surrounding the egg in order to help the embryo hatch out and aid in the implantation process of the growing embryo.
- Intracytoplasmic sperm injection (ICSI) is beneficial in the case of male factor infertility where sperm counts are very low or failed fertilization occurred with previous IVF attempt(s). The ICSI procedure involves a single sperm carefully injected into the center of an egg using a microneedle. With ICSI, only one sperm per egg is needed. Without ICSI, you need between 50,000 and 100,000.[2] This method is also sometimes employed when donor sperm is used.
 Intracytoplasmic sperm injection (ICSI)
Intracytoplasmic sperm injection (ICSI) - Autologous endometrial coculture is a possible treatment for patients who have failed previous IVF attempts or who have poor embryo quality. The patient's fertilized eggs are placed on top of a layer of cells from the patient's own uterine lining, creating a more natural environment for embryo development.
- In zygote intrafallopian transfer (ZIFT), egg cells are removed from the woman's ovaries and fertilized in the laboratory; the resulting zygote is then placed into the fallopian tube.
- Cytoplasmic transfer is the technique in which the contents of a fertile egg from a donor are injected into the infertile egg of the patient along with the sperm.
- Egg donors are resources for women with no eggs due to surgery, chemotherapy, or genetic causes; or with poor egg quality, previously unsuccessful IVF cycles or advanced maternal age. In the egg donor process, eggs are retrieved from a donor's ovaries, fertilized in the laboratory with the sperm from the recipient's partner, and the resulting healthy embryos are returned to the recipient's uterus.
- Sperm donation may provide the source for the sperm used in IVF procedures where the male partner produces no sperm or has an inheritable disease, or where the woman being treated has no male partner.
- Preimplantation genetic diagnosis (PGD) involves the use of genetic screening mechanisms such as fluorescent in-situ hybridization (FISH) or comparative genomic hybridization (CGH) to help identify genetically abnormal embryos and improve healthy outcomes.
- Embryo splitting can be used for twinning to increase the number of available embryos.[3]
Surrogacy
Surrogacy, where a woman agrees to become pregnant and deliver a child for a contracted party. It may be her own genetic child, or a child conceived through natural insemination, in vitro fertilization or embryo transfer using another woman's ova. Surrogacy via a gestational carrier is an option when a patient's medical condition prevents a safe pregnancy, when a patient has ovaries but no uterus due to congenital absence or previous surgical removal, and where a patient has no ovaries and is also unable to carry a pregnancy to full term.
Others
Other assisted reproduction techniques include:
- In gamete intrafallopian transfer (GIFT) a mixture of sperm and eggs is placed directly into a woman's fallopian tubes using laparoscopy following a transvaginal ovum retrieval.
- Sex selection is the attempt to control the sex of offspring to achieve a desired sex. It can be accomplished in several ways, both pre- and post-implantation of an embryo, as well as at birth. Pre-implantation techniques include PGD, but also sperm sorting.
- Reproductive surgery, treating e.g. fallopian tube obstruction and vas deferens obstruction, or reversing a vasectomy by a reverse vasectomy.
- In surgical sperm retrieval (SSR) the reproductive urologist obtains sperm from the vas deferens, epididymis or directly from the testis in a short outpatient procedure.
- By cryopreservation, eggs, sperm and reproductive tissue can be preserved for later IVF.
Risks
The majority of IVF-conceived infants do not have birth defects.[4] However, some studies have suggested that assisted reproductive technology is associated with an increased risk of birth defects.[5][6] In the largest U.S. study, which used data from a statewide registry of birth defects,[7] 6.2% of IVF-conceived children had major defects, as compared with 4.4% of naturally conceived children matched for maternal age and other factors (odds ratio, 1.3; 95% confidence interval, 1.00 to 1.67).[4]
The main risks are:
- Genetic disorders[8]
- Low birth weight. In IVF and ICSI, a risk factor is the decreased expression of proteins in energy metabolism; Ferritin light chain and ATP5A1.[9]
- Preterm birth. Low birth weight and preterm birth are strongly associated with many health problems, such as visual impairment and cerebral palsy, and children born after IVF are roughly twice as likely to have cerebral palsy.[10]
Other risk factors are:
- Membrane damage, which may be reflected by increased expression of the membrane fusion proteins NAPA and Annexin A3.[9]
Sperm donation is an exception, with a birth defect rate of almost a fifth compared to the general population.[11] It may be explained by that sperm banks accept only people with high sperm count.
Current data indicate little or no increased risk for postpartum depression among women who use ART.[12]
Usage of assisted reproductive technology including ovarian stimulation, artificial insemination and in vitro fertilization have been associated with an increased overall risk of childhood cancer in the offspring, which may be caused by the same original disease or condition that caused the infertility or subfertility in the mother or father.[13]
Usage
Assisted reproductive technology procedures performed in the U.S. has more than doubled over the last 10 years, with 140,000 procedures in 2006,[14] resulting in 55,000 births.[14]
In Australia, 3.1% of births are a result of ART.[15]
In case of discontinuation of fertility treatment, the most common reasons have been estimated to be: postponement of treatment (39%), physical and psychological burden (19%, psychological burden 14%, physical burden 6.32%), relational and personal problems (17%, personal reasons 9%, relational problems 9%), treatment rejection (13%) and organizational (12%) and clinic (8%) problems.[16]
Costs
United States
Many Americans do not have insurance coverage for fertility investigations and treatments. Many states are starting to mandate coverage, and the rate of use is 277% higher in states with complete coverage.[17]
There are some health insurance companies that cover diagnosis of infertility but frequently once diagnosed will not cover any treatment costs.
2005 approximate treatment/diagnosis costs (United States, costs in US$):
- Initial workup: hysteroscopy, hysterosalpingogram, blood tests ~$2,000
- Intrauterine Insemination (IUI) aka Artificial insemination ~ $200– 900 per. trial
- Sonohysterogram (SHG) ~ $600–$1,000
- Clomiphene citrate cycle ~ $200–$500
- IVF cycle ~ $10,000–$30,000
- Use of a surrogate mother to carry the child – dependent on arrangements
Another way to look at costs is to determine the expected cost of establishing a pregnancy. Thus if a clomiphene treatment has a chance to establish a pregnancy in 8% of cycles and costs $500, the expected cost is $6,000 to establish a pregnancy, compared to an IVF cycle (cycle fecundity 40%) with a corresponding expected cost of $30,000 ($12,000/.4).
For the community as a whole, the cost of IVF on average pays back by 700% by tax from future employment by the conceived human being.[18]
United Kingdom
In the United Kingdom, all patients have the right to preliminary testing, provided free of charge by the National Health Service. However, treatment is not widely available on the NHS and there can be long waiting lists. Many patients therefore pay for immediate treatment within the NHS or seek help from private clinics.
In 2013, the National Institute for Health and Care Excellence published new guidelines about who should have access to IVF treatment on the NHS in England and Wales.[19]
Women aged under 40 should be offered three cycles of IVF treatment on the NHS if they have been trying to get pregnant through regular unprotected intercourse for two years, or have not been able to get pregnant after 12 cycles of artificial insemination. The guidelines also say women aged between 40 and 42 should be offered one cycle of IVF on the NHS if all of the following additional criteria are also met: They have never had IVF treatment before, have no evidence of low ovarian reserve (this is when eggs in the ovary are low in number or low in quality) and have been informed of the additional implications of IVF and pregnancy at this age. However, if tests show IVF is the only treatment likely to help them get pregnant, women should be referred for IVF straight away.
This policy is often modified by local Clinical Commissioning Groups, in a fairly blatant breach of the NHS Constitution for England which provides that patients have the right to drugs and treatments that have been recommended by NICE for use in the NHS. For example the Cheshire, Merseyside and West Lancashire Clinical Commissioning Group insists on additional conditions:[20]
- The person undergoing treatment must have commenced treatment before her 40th birthday.
- The person undergoing treatment must have a BMI of between 19 and 29.
- Neither partner must have any living children, from either the current or previous relationships. This includes adopted as well as biological children.
- Sub-fertility must not be the direct result of a sterilisation procedure in either partner (this does not include conditions where sterilisation occurs as a result of another medical problem). Couples who have undertaken a reversal of their sterilisation procedure are not eligible for treatment.
Sweden
In Sweden, official fertility clinics provide most necessary treatments and initial workup, but there are long waiting lists, especially for egg donations, since the donor gets just as low reward as the receiving couple are charged. However, there are private fertility clinics.
Canada
Some treatments are covered by OHIP (public health insurance) in Ontario and others are not. Those undergoing artificial insemination or with bilaterally blocked fallopian tubes and under 40 have treatment is covered but are still required to pay lab fees (around $3,000–4,000). Coverage varies in other provinces. Most other patients are required to pay for treatments themselves.[21]
Israel
Israel's national health insurance, which is mandatory for all Israeli citizens, covers nearly all fertility treatments. IVF costs are fully subsidized up to the birth of two children for all Israeli women, including single women and lesbian couples. Embryo transfers for purposes of gestational surrogacy are also covered.[22]
New Zealand
The national public health system of New Zealand covers IVF treatment in specific circumstances only, based on a 'points for conception challenges' equation. Publicly funded IVF treatments are limited (between one and three treatments dependent on criteria) and are subject to substantial wait-lists, dependent on local health funding region, which raises potential inequity of ART support across the country. Infertility testing through blood tests can be covered by public funding, however in the absence of explicit gynecological complications, additional investigations are may not be covered publicly. Investigation such as a hysterosalpingogram may be covered, but the wait-list could be in excess of six weeks, whereas a privately sourced HSG can cost $NZ900 but is readily available. Many New Zealanders select self-funded IVF cycles, at approximately $NZ10,000 per cycle, and other forms of ART, such as IUI, at approximately $NZ1200, using the services of private fertility clinics, which in itself is a growing local industry. Individuals using private services are generally not covered under personal health insurance policies in New Zealand.
Germany
On 27 January 2009, the Federal Constitutional Court ruled that it is unconstitutional, that the health insurance companies have to bear only 50% of the cost for IVF.[23] On 2 March 2012, the Federal Council has approved a draft law of some federal states, which provides that the federal government provides a subsidy of 25% to the cost. Thus, the share of costs borne for the pair would drop to just 25%.[24]
Jordan
In Jordan, not everyone has insurance coverage for fertility investigation and treatment. Army forces cover the army members for all infertility investigations and treatments. It also covers three trials of IVF in primary infertility cases. Some health insurance companies cover the diagnosis and the treatment of infertility for those with government health insurance, but it will not cover any of the assisted reproductive techniques. In private sector, there are many centers offering private treatment for infertility including the assisted reproductive techniques. Conventional I.V.F cost 1170JD = 1654 US$, ICSI cost 1270 JD = 1797 US$ Both prices include assisted hatching. But does not include the cost of medication which averages between 500-700 JD which equals around 700-1000 US$ [25]
Ethics
Some couples find it difficult to stop treatment despite very bad prognosis, resulting in futile therapies. This may give ART providers a difficult decision of whether to continue or refuse treatment.[26]
For treatment-specific ethical considerations, see entries in individual subarticles, e.g. In vitro fertilisation, Surrogacy and Sperm donation
Some assisted reproductive technologies can in fact be harmful to both the mother and child. Posing a psychological and a physical health risk, which may impact the ongoing use of these treatments. The adverse affects may cause for alarm, and they should be tightly regulated to ensure candidates are not only mentally, but physically prepared.[27]
Fictional representation
Films and other fiction depicting emotional struggles of assisted reproductive technology have had an upswing in the latter part of the 2000s decade, although the techniques have been available for decades.[28] Yet, the amount of people that can relate to it by personal experience in one way or another is ever growing, and the variety of trials and struggles are huge.[28]
For specific examples, refer to the fiction sections in individual subarticles, e.g. surrogacy, sperm donation and fertility clinic.
In addition, reproduction and pregnancy in speculative fiction has been present for many decades.
See also
- The Fertility Chase (medical documentary series)
- Religious response to ART
- Sperm donation
- Sperm bank
- Artificial uterus
- Human cloning
- Diethylstilbestrol
- Spontaneous conception, the unassisted conception of a subsequent child after prior use of assisted reproductive technology
References
- ↑ Knock Yourself Up: A Tell-All Guide to Becoming a Single Mom by Louise Sloan. Reviewed in Newsweek 27 October 2007.
- ↑ In Vitro Fertilisation with intracytoplasmic sperm injection (IVF-ICSI) infographic Retrieved 28. June 2015.
- ↑ Illmensee K, Levanduski M, Vidali A, Husami N, Goudas VT (February 2009). "Human embryo twinning with applications in reproductive medicine". Fertil. Steril. 93 (2): 423–7. doi:10.1016/j.fertnstert.2008.12.098. PMID 19217091.
- 1 2 Van Voorhis BJ (2007). "Clinical practice. In vitro fertilization". N Engl J Med 356 (4): 379–86. doi:10.1056/NEJMcp065743. PMID 17251534.
- ↑ Kurinczuk JJ, Hansen M, Bower C (2004). "The risk of birth defects in children born after assisted reproductive technologies". Current Opinion in Obstetrics and Gynecology 16 (3): 201–9. doi:10.1097/00001703-200406000-00002. PMID 15129049.
- ↑ Hansen M, Bower C, Milne E, de Klerk N, Kurinczuk JJ (2005). "Assisted reproductive technologies and the risk of birth defects—a systematic review" (PDF). Hum Reprod 20 (2): 328–38. doi:10.1093/humrep/deh593. PMID 15567881.
- ↑ Olson CK, Keppler-Noreuil KM, Romitti PA, Budelier WT, Ryan G, Sparks AE, Van Voorhis BJ (2005). "In vitro fertilization is associated with an increase in major birth defects". Fertil Steril 84 (5): 1308–15. doi:10.1016/j.fertnstert.2005.03.086. PMID 16275219.
- ↑ "IVF FAQs". Pacific Fertility Center. Retrieved 4 November 2014.
- 1 2 Zhang Y, Zhang YL, Feng C; et al. (September 2008). "Comparative proteomic analysis of human placenta derived from assisted reproductive technology". Proteomics 8 (20): 4344–56. doi:10.1002/pmic.200800294. PMID 18792929.
- ↑ Hvidtjørn D, Schieve L, Schendel D, Jacobsson B, Sværke C, Thorsen P (2009). "Cerebral palsy, autism spectrum disorders, and developmental delay in children born after assisted conception: a systematic review and meta-analysis". Arch Pediatr Adolesc Med 163 (1): 72–83. doi:10.1001/archpediatrics.2008.507. PMID 19124707.
- ↑ motherearthnews.com – THE SPERM CRISIS
- ↑ Ross, L. E.; McQueen, K.; Vigod, S.; Dennis, C.-L. (2010). "Risk for postpartum depression associated with assisted reproductive technologies and multiple births: A systematic review". Human Reproduction Update 17 (1): 96–106. doi:10.1093/humupd/dmq025. PMID 20605900.
- ↑ Hargreave, Marie; Jensen, Allan; Toender, Anita; Andersen, Klaus Kaae; Kjaer, Susanne Krüger (2013). "Fertility treatment and childhood cancer risk: A systematic meta-analysis". Fertility and Sterility 100 (1): 150–61. doi:10.1016/j.fertnstert.2013.03.017. PMID 23562045.
- 1 2 chicagotribune.com Infertility by the numbers Colleen Mastony. June 21, 2009
- ↑ 'More IVF babies but less multiple births' THE AUSTRALIAN. September 24, 2009
- ↑ Gameiro, S.; Boivin, J.; Peronace, L.; Verhaak, C. M. (2012). "Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment". Human Reproduction Update 18 (6): 652–69. doi:10.1093/humupd/dms031. PMC 3461967. PMID 22869759.
- ↑ Jain T, Harlow BL, Hornstein MD (August 2002). "Insurance coverage and outcomes of in vitro fertilization". N. Engl. J. Med. 347 (9): 661–6. doi:10.1056/NEJMsa013491. PMID 12200554.
- ↑ Connolly MP, Pollard MS, Hoorens S, Kaplan BR, Oskowitz SP, Silber SJ (September 2008). "Long-term economic benefits attributed to IVF-conceived children: a lifetime tax calculation". Am J Manag Care 14 (9): 598–604. PMID 18778175.
- ↑ "IVF". NHS Choices. Retrieved 19 April 2014.
- ↑ "Services & how we can help". Liverpool Women's NHS Foundation Trust. Retrieved 19 April 2014.
- ↑ IVF Canada
- ↑ Teman, Elly. 2010. Birthing a Mother: the Surrogate Body and the Pregnant Self. Berkeley: University of California Press
- ↑ Zuschüsse der Krankenversicherung für eine künstliche Befruchtung Retrieved 2. January 2013.
- ↑ Finanzierung künstlicher Befruchtung Retrieved 2. January 2013.
- ↑ http://www.layyous.com/en/infertility/ivf-patients-faq.htm
- ↑ Ethics Committee of the American Society for Reproductive Medicine (2009). "Fertility treatment when the prognosis is very poor or futile". Fertility and Sterility 92 (4): 1194–7. doi:10.1016/j.fertnstert.2009.07.979. PMID 19726040.
- ↑ Noah, Lars (2003). "Assisted Reproductive Technologies and the Pitfalls of Unregulated Biomedical Innovation". Florida Law Review 55 (2): 604–609.
- 1 2 chicagotribune.com --> Heartache of infertility shared on stage, screen By Colleen Mastony, Tribune reporter. June 21, 2009
External links
- Centers for Disease Control and Prevention (CDC), Assisted Reproductive Technology
- inviTRA is an International fair for patients where professional of assisted reproductive technology give speeches and solutions to people with fertility problems.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||