Alveolar–arterial gradient
| BMP/ELECTROLYTES: | |||
| Na+ = 140 | Cl− = 100 | BUN = 20 | / |
| Glu = 150 | |||
| K+ = 4 | CO2 = 22 | PCr = 1.0 | \ |
| ARTERIAL BLOOD GAS: | |||
| HCO3− = 24 | paCO2 = 40 | paO2 = 95 | pH = 7.40 |
| ALVEOLAR GAS: | |||
| pACO2 = 36 | pAO2 = 105 | A-a g = 10 | |
| OTHER: | |||
| Ca = 9.5 | Mg2+ = 2.0 | PO4 = 1 | |
| CK = 55 | BE = −0.36 | AG = 16 | |
| SERUM OSMOLARITY/RENAL: | |||
| PMO = 300 | PCO = 295 | POG = 5 | BUN:Cr = 20 |
| URINALYSIS: | |||
| UNa+ = 80 | UCl− = 100 | UAG = 5 | FENa = 0.95 |
| UK+ = 25 | USG = 1.01 | UCr = 60 | UO = 800 |
| PROTEIN/GI/LIVER FUNCTION TESTS: | |||
| LDH = 100 | TP = 7.6 | AST = 25 | TBIL = 0.7 |
| ALP = 71 | Alb = 4.0 | ALT = 40 | BC = 0.5 |
| AST/ALT = 0.6 | BU = 0.2 | ||
| AF alb = 3.0 | SAAG = 1.0 | SOG = 60 | |
| CSF: | |||
| CSF alb = 30 | CSF glu = 60 | CSF/S alb = 7.5 | CSF/S glu = 0.4 |
The Alveolar–arterial gradient (A-aO2,[1] or A–a gradient), is a measure of the difference between the alveolar concentration (A) of oxygen and the arterial (a) concentration of oxygen. It is used in diagnosing the source of hypoxemia.[2]
It helps to assess the integrity of alveolar capillary unit. For example, in high altitude, the arterial oxygen [[PaO<sub>2</sub>]] is low but only because the alveolar oxygen (PAO2) is also low. However, in states of ventilation perfusion mismatch, such as pulmonary embolism or right-to-left shunt, oxygen is not effectively transferred from the alveoli to the blood which results in elevated A-a gradient
Equation
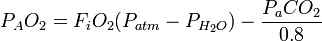
The equation for calculating the A–a gradient is:
Where:
- PAO2 = alveolar PO2 (calculated from the alveolar gas equation)
- PaO2 = arterial PO2 (measured in arterial blood)
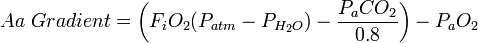
In its expanded form, the A–a gradient can be calculated by:
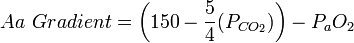
On room air ( FiO2 = 0.21, or 21% ), at sea level ( Patm = 760 mmHg ) assuming 100% humidity in the alveoli, a simplified version of the equation is:
Values and meaning
The A–a gradient is useful in determining the source of hypoxemia. The measurement helps isolate the location of the problem as either intrapulmonary (within the lungs) or extrapulmonary (somewhere else in the body).
A normal A–a gradient for a young adult non-smoker breathing air, is between 5–10 mmHg. Normally, the A–a gradient increases with age. For every decade a person has lived, their A–a gradient is expected to increase by 1 mmHg. A conservative estimate of normal A–a gradient is less than [age in years/4] + 4. Thus, a 40-year-old should have an A–a gradient less than 14.
An abnormally increased A–a gradient suggests a defect in diffusion, V/Q (ventilation/perfusion ratio) mismatch, or right-to-left shunt.[4]
Because A–a gradient is approximated as: (150 − 5/4(pCO2)) – PaO2 at sea level and on room air (0.21x(760-47) = 149.7 mmHg for the alveolar oxygen partial pressure, after accounting for the water vapor), the direct mathematical cause of a large value is that the blood has a low PO2, a low PCO2, or both. CO2 is very easily exchanged in the lungs and low PCO2 directly correlates with high minute ventilation; therefore a low arterial PCO2 indicates that extra respiratory effort is being used to oxygenate the blood. A low PaO2 indicates that at the patient's current minute ventilation (whether high or normal) is not enough to allow adequate oxygen diffusion into the blood. Therefore the A–a gradient essentially demonstrates a high respiratory effort (low arterial PCO2) relative to the achieved level of oxygenation (arterial PO2). A high A–a gradient could indicate a patient breathing hard to achieve normal oxygenation, a patient breathing normally and attaining low oxygenation, or a patient breathing hard and still failing to achieve normal oxygenation.
If lack of oxygenation is proportional to low respiratory effort, then the A–a gradient is not increased; a healthy person who hypoventilates would have hypoxia, but a normal A–a gradient. At an extreme, high CO2 levels from hypoventilation can mask an existing high A–a gradient. This mathematical artifact makes A–a gradient more clinically useful in the setting of hyperventilation.
| ||||||||||||||||||||||||||
See also
References
- ↑ Logan, Carolynn M.; Rice, M. Katherine (1987). Logan's Medical and Scientific Abbreviations. Philadelphia: J. B. Lippincott Company. p. 4. ISBN 0-397-54589-4.
- ↑ "iROCKET Learning Module: Intro to Arterial Blood Gases, Pt. 1". Retrieved 2008-11-14.
- ↑ "Alveolar-arterial Gradient". Retrieved 2008-11-14.
- ↑ Costanzo, Linda (2006). BRS Physiology. Hagerstown: Lippincott Williams & Wilkins. ISBN 0-7817-7311-3.