Facial nerve paralysis
| Facial nerve paralysis | |
|---|---|
 | |
| Classification and external resources | |
| Specialty | neurology |
| ICD-10 | G51 |
| ICD-9-CM | 351 |
| MedlinePlus | 003028 |
| eMedicine | plastic/522 |
| MeSH | D005158 |
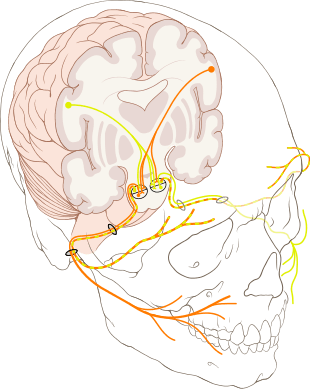
Facial nerve paralysis is a common problem that involves the paralysis of any structures innervated by the facial nerve. The pathway of the facial nerve is long and relatively convoluted, and so there are a number of causes that may result in facial nerve paralysis.[1] The most common is Bell's palsy, an idiopathic disease that may only be diagnosed by exclusion.
Classification
Facial nerve paralysis may be divided into supranuclear and infranuclear lesions.
Supranuclear and nuclear lesions
Central facial palsy can be caused by a lacunar infarct affecting fibers in the internal capsule going to the nucleus. The facial nucleus itself can be affected by infarcts of the pontine arteries.
Infranuclear lesions
Infranuclear lesions refer to the majority of causes of facial palsy.
Signs and symptoms
Facial nerve paralysis is characterised by unilateral facial weakness, with other symptoms including loss of taste, hyperacusis, and decreased salivation and tear secretion. Other signs may be linked to the cause of the paralysis, such as vesicles in the ear, which is may occur if the facial palsy is due to shingles. Symptoms may develop over several hours.[2] :1228 Acute facial pain radiating from the ear may precede the onset of other symptoms.[3] :2585
Causes
Bell's palsy
Bell's palsy is the most common cause of acute facial nerve paralysis. There is no known cause of Bell's palsy,[2][3] although it has been associated with herpes simplex infection. Bell's palsy may develop over several days, and may last several months, in the majority of cases recovering spontaneously. It is typically diagnosed clinically, in patients with no risk factors for other causes, without vesicles in the ear, and with no other neurological signs. Recovery may be delayed in the elderly, or those with a complete paralysis. Bell's palsy is often treated with corticosteroids.[2][3]
Infection
Reactivation of herpes zoster virus, as well as being associated with Bell's palsy, may also be a direct cause of facial nerve palsy. Reactivation of latent virus within the dorsal root ganglion of the facial nerve is associated with vesicles affecting the ear canal, and termed Ramsay Hunt syndrome type II.[3] In addition to facial paralysis, symptoms may include ear pain and vesicles, sensorineural hearing loss, and vertigo. Management includes Antiviral drugs and oral steroids.
Otitis media is an infection in the middle ear, which can spread to the facial nerve and inflame it, causing compression of the nerve in its canal. Antibiotics are used to control the otitis media, and other options include a wide myringotomy (an incision in the tympanic membrane) or decompression if the patient does not improve. Chronic otitis media usually presents in an ear with chronic discharge (otorrhea), or hearing loss, with or without ear pain (otalgia). Once suspected, there should be immediate surgical exploration to determine if a cholesteatoma has formed as this must be removed if present. Inflammation from the middle ear can spread to the canalis facialis of the temporal bone - through this canal travels the facial nerve together with the steatoacoustisus nerve. In the case of inflammation the nerve is exposed to edema and subsequent high pressure, resulting in a periferic type palsy.
Lyme disease, caused by chronic Borrelia burgdorferi infection, is a common cause of facial nerve paralysis in endemic areas.[3]
Trauma
Physical trauma, especially fractures of the temporal bone, may also cause acute facial nerve paralysis. Understandably, the likelihood of facial paralysis after trauma depends on the location of the trauma. Most commonly, facial paralysis follows temporal bone fractures, though the likelihood depends on the type of fracture.
Transverse fractures in the horizontal plane present the highest likelihood of facial paralysis (40-50%). Patients may also present with blood behind the tympanic membrane, sensory deafness, and vertigo; the latter two symptoms due to damage to vestibulocochlear nerve and the inner ear. Longitudinal fracture in the vertical plane present a lower likelihood of paralysis (20%). Patients may present with blood coming out of the external auditory meatus), tympanic membrane tear, fracture of external auditory canal, and conductive hearing loss. In patients with mild injuries, management is the same as with Bell's palsy – protect the eyes and wait. In patients with severe injury, progress is followed with nerve conduction studies. If nerve conduction studies show a large (>90%) change in nerve conduction, the nerve should be decompressed. The facial paralysis can follow immediately the trauma due to direct damage to the facial nerve, in such cases a surgical treatment may be attempted. In other cases the facial paralysis can occur a long time after the trauma due to oedema and inflammation. In those cases steroids can be a good help.
Tumors
A tumor compressing the facial nerve anywhere along its complex pathway can result in facial paralysis. Common culprits are facial neuromas, congenital cholesteatomas, hemangiomas, acoustic neuromas, parotid gland neoplasms, or metastases of other tumours.[4][5]
Often, since facial neoplasms have such an intimate relationship with the facial nerve, removing tumors in this region becomes perplexing as the physician is unsure how to manage the tumor without causing even more palsy. Typically, benign tumors should be removed in a fashion that preserves the facial nerve, while malignant tumors should always be resected along with large areas of tissue around them, including the facial nerve. While this will inevitably lead to heightened paralysis, safe removal of a malignant neoplasm is worth the often treatable palsy that follows. In the best case scenario, paralysis can be corrected with techniques including hypoglossal-facial nerve anastomosis, end-to-end nerve repair, cross facial nerve grafting, or muscle transfer/transposition techniques, such as the gracilis free muscle transfer.
Patients with facial nerve paralysis resulting from tumours usually present with a progressive, twitching paralysis, other neurological signs, or a recurrent Bell's palsy-type presentation. The latter should always be suspicious, as Bell's palsy should not recur. A chronically discharging ear must be treated as a cholesteatoma until proven otherwise; hence, there must be immediate surgical exploration. Computed tomography (CT) or magnetic resonance (MR) imaging should be used to identify the location of the tumour, and it should be managed accordingly.
Stroke
Central facial palsy can be caused by a lacunar infarct affecting fibers in the internal capsule going to the nucleus. The facial nucleus itself can be affected by infarcts of the pontine arteries.
Other
Other causes may include:
- Diabetes mellitus[3]
- Facial nerve paralysis, sometimes bilateral, is a common manifestation of sarcoidosis of the nervous system, neurosarcoidosis.[3]
- Bilateral facial nerve paralysis may occur in Guillain-Barre syndrome, an autoimmune condition of the peripheral nervous system.[3]
- Moebius syndrome is a bilateral facial paralysis resulting from the underdevelopment of the VII cranial nerve (facial nerve), which is present at birth. The VI cranial nerve, which controls lateral eye movement, is also affected, so people with Moebius syndrome cannot form facial expression or move their eyes from side to side. Moebius syndrome is extremely rare, and its cause or causes are not known.
Investigation and diagnosis
A thorough medical history and physical examination, including a neurological examination, are the first steps in making a diagnosis. This alone may be sufficient to diagnose Bell's Palsy, in the absence of other findings.[3] Additional investigations may be pursued, including blood tests such as ESR for inflammation, and blood sugar levels for diabetes. If other specific causes, such as sarcoidosis or Lyme disease are suspected, specific tests such as angiotensin converting enzyme levels, chest x-ray or Lyme titer may be pursued.[3] If there is a history of trauma, or a tumour is suspected, a CT scan may be used.
Treatment
Primary neuropathy of facial nerve at the time of injury. Interpositional graft by using sural or greater auricular nerve grafts. Cranial nerve crossover, this is most commonly seen following nerve sacrifice. Regional muscle transposition using temporalis muscle\ masseter muscle. Free muscle transfer like gracilis muscle.
References
- ↑ "Facial Nerve". Retrieved 2009-11-22.
- 1 2 3 Colledge, Nicki R.; Walker, Brian R.; Ralston, Stuart H., eds. (2010). Davidson's principles and practice of medicine. illust. Robert Britton (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3084-0.
- 1 2 3 4 5 6 7 8 9 10 Fauci, Anthony S.; Harrison, T. R., eds. (2008). Harrison's principles of internal medicine (17th ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-147693-5.
- ↑ Thompson AL, Bharatha A, Aviv RI, Nedzelski J, Chen J, Bilbao JM, Wong J, Saad R, Symons SP (July 2009). "Chondromyoid fibroma of the mastoid facial nerve canal mimicking a facial nerve schwannoma". Laryngoscope 119 (7): 1380–1383. doi:10.1002/lary.20486.
- ↑ Thompson AL, Aviv RI, Chen JM, Nedzelski JM, Yuen H-W, Fox AJ, Bharatha A, Bartlett ES, Symons SP (December 2009). "MR imaging of facial nerve schwannoma". Laryngoscope 119 (12): 2428–2436. doi:10.1002/lary.20644.