Lamivudine
 | |
 | |
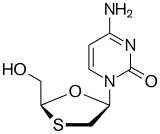
| Systematic (IUPAC) name | |
|---|---|
|
4-amino-1-[(2R,5S)-2-(hydroxymethyl)-1,3-oxathiolan-5-yl]-1,2-dihydropyrimidin-2-one | |
| Clinical data | |
| Trade names | Epivir |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a696011 |
| Pregnancy category | |
| Legal status | |
| Routes of administration | Oral |
| Pharmacokinetic data | |
| Bioavailability | 86% |
| Protein binding | Less than 36% |
| Biological half-life | 5 to 7 hours |
| Excretion | Renal (circa 70%) |
| Identifiers | |
| CAS Number |
134678-17-4 |
| ATC code | J05AF05 |
| PubChem | CID 73339 |
| DrugBank |
DB00709 |
| ChemSpider |
66068 |
| UNII |
2T8Q726O95 |
| KEGG |
D00353 |
| ChEMBL |
CHEMBL141 |
| NIAID ChemDB | 000388 |
| Synonyms | L-2′,3′-dideoxy-3′-thiacytidine |
| PDB ligand ID | 3TC (PDBe, RCSB PDB) |
| Chemical data | |
| Formula | C8H11N3O3S |
| Molar mass | 229.26 g/mol |
| |
| |
| | |
Lamivudine (2′,3′-dideoxy-3′-thiacytidine, commonly called 3TC) is an antiretroviral medication used to prevent and treat HIV/AIDS and used to treat chronic hepatitis B.[1]
It is of the nucleoside analog reverse transcriptase inhibitor (NRTI) class. It is marketed in the United States under the tradenames Epivir and Epivir-HBV.
It is on the World Health Organization's List of Essential Medicines, a list of the most important medication needed in a basic health system.[2]
Medical uses
Lamivudine has been used for treatment of chronic hepatitis B at a lower dose than for treatment of HIV/AIDS. It improves the seroconversion of e-antigen positive hepatitis B and also improves histology staging of the liver. Long term use of lamivudine leads to emergence of a resistant hepatitis B virus (YMDD) mutant. Despite this, lamivudine is still used widely as it is well tolerated.
Resistance
In HIV, high level resistance is associated with the M184V/I mutation in the reverse transcriptase gene as reported by Raymond Schinazi's group at Emory University. GlaxoSmithKline claimed that the M184V mutation reduces "viral fitness", because of the finding that continued lamivudine treatment causes the HIV viral load to rebound but at a much lower level, and that withdrawal of lamivudine results in a higher viral load rebound with rapid loss of the M184V mutation; GSK therefore argued that there may be benefit in continuing lamivudine treatment even in the presence of high level resistance, because the resistant virus is "less fit". The COLATE study has suggested that there is no benefit to continuing lamivudine treatment in patients with lamivudine resistance.[3] A better explanation of the data is that lamivudine continues to have a partial anti-viral effect even in the presence of the M184V mutation.
In hepatitis B, lamivudine resistance was first described in the YMDD (tyrosine-methionine-aspartate-aspartate) locus of the HBV reverse transcriptase gene. The HBV reverse transcriptase gene is 344 amino acids long and occupies codons 349 to 692 on the viral genome. The most commonly encountered resistance mutations are M204V/I/S.[4] The change in amino acid sequence from YMDD to YIDD results in a 3.2 fold reduction in the error rate of the reverse transcriptase, which correlates with a significant growth disadvantage of the virus. Other resistance mutations are L80V/I, V173L and L180M.[5]
Mechanism of action
Lamivudine is an analogue of cytidine. It can inhibit both types (1 and 2) of HIV reverse transcriptase and also the reverse transcriptase of hepatitis B virus. It is phosphorylated to active metabolites that compete for incorporation into viral DNA. They inhibit the HIV reverse transcriptase enzyme competitively and act as a chain terminator of DNA synthesis. The lack of a 3'-OH group in the incorporated nucleoside analogue prevents the formation of the 5' to 3' phosphodiester linkage essential for DNA chain elongation, and therefore, the viral DNA growth is terminated.
Lamivudine is administered orally, and it is rapidly absorbed with a bio-availability of over 80%. Some research suggests that lamivudine can cross the blood–brain barrier. Lamivudine is often given in combination with zidovudine, with which it is highly synergistic. Lamivudine treatment has been shown to restore zidovudine sensitivity of previously resistant HIV. Lamivudine showed no evidence of carcinogenicity or mutagenicity in in vivo studies in mice and rats at doses from 10 to 58 times those used in humans.[6]
History
Racemic BCH-189 (the minus form is known as Lamivudine) was invented by Dr. Bernard Belleau while at work at McGill University and Dr Paul Nguyen-Ba at the Montreal-based IAF BioChem International, Inc. laboratories in 1988 and the minus enantiomer isolated in 1989. Samples were first sent to Dr. Yung-Chi Cheng of Yale University for study of its toxicity. When used in combination with AZT, he discovered that Lamivudine's negative form reduced side effects and increased the drug's efficiency at inhibiting reverse transcriptase.[7] The combination of Lamivudine and AZT increased the efficiency at inhibiting an enzyme HIV uses to reproduce its genetic material. As a result, Lamivudine was identified as a less toxic agent to mitochondria DNA than other retroviral drugs.[8] Dr. Cheng in collaboration with R.F. Schinazi and D.C. Liotta first reported the anti-hepatitis B virus (HBV) activity of Lamivudine in cell culture which eventually led to the first oral antiviral agent for the treatment of HBV. Subsequently the group at Emory University headed by Dr. Dennis C. Liotta Dr. Woo-Baeg Choi and Dr. Raymond F. Schinazi developed a synthesis for the BCH-189 that gave exclusively the beta-diastereomers. They then went on to resolve the two enantiomers and demonstrated that the antiviral activity at non-toxic concentrations resided in the (−)-enantiomer, now called Lamivudine. The Emory patents to lamivudine were later invalidated by the original inventors. The drug's effectiveness for treating HIV in combination with AZT was discovered accidentally when a patient took Zidovudine secretly while in a clinical trial of Lamivudine monotherapy. The drug was later licensed to the British pharmaceutical company Glaxo by Biochem Pharma (now Shire Pharmaceuticals) for a 14 percent royalty. GlaxoSmithKline subsequently ceded the product to its ViiV Healthcare joint venture in 2009.
Lamivudine was approved by the Food and Drug Administration (FDA) on November 17, 1995 for use with zidovudine (AZT) and again in 2002 as a once-a-day dosed medication. The fifth antiretroviral drug on the market, it was the last NRTI for three years while the approval process switched to protease inhibitors. According to the manufacturer's 2004 annual report, its patent will expire in the United States in 2010 and in Europe in 2011.
On September 2014, Dr. Gorbee Logan, a Liberian physician, reported positive results while treating Ebola virus disease with Lamivudine. Out of 15 patients treated with the antiviral, 13 (those treated within the third to fifth day of symptoms being manifested) survived the disease and were declared virus-free; the remaining cases (treated from the fifth day or later) died.[9][10]
Presentation
- Epivir 150 mg or 300 mg tablets (GlaxoSmithKline; US and UK) for the treatment of HIV;
- Epivir-HBV 100 mg tablets (GlaxoSmithKline; US only) for the treatment of hepatitis B;
- Zeffix 100 mg tablets (GlaxoSmithKline; UK only) for the treatment of hepatitis B.
- 3TC 150 mg tablets (GlaxoSmithKline; South Africa) for the treatment of HIV;
Lamivudine is also available in fixed combinations with other HIV drugs:
- Combivir (with zidovudine);
- Epzicom/Kivexa (with abacavir);
- Trizivir (with zidovudine and abacavir)
See also
References
- ↑ "Lamivudine". The American Society of Health-System Pharmacists. Retrieved 31 July 2015.
- ↑ "WHO Model List of EssentialMedicines" (PDF). World Health Organization. October 2013. Retrieved 22 April 2014.
- ↑ Fox Z, Dragsted UB, Gerstoft J, et al. (2006). "A randomized trial to evaluate continuation versus discontinuation of lamivudine in individuals failing a lamivudine-containing regimen: The COLATE trial". Antiviral Therapy 11 (6): 761–70. PMID 17310820.
- ↑ http://hivdb.stanford.edu/index.html Stanford University Drug Resistance Database.
- ↑ Koziel MJ, Peters MG (2007). "Viral hepatitis in HIV infection". N Engl J Med 356 (14): 1445–54. doi:10.1056/NEJMra065142. PMID 17409326.
- ↑ "Epivir package insert" (PDF). GlaxoSmithKline. Retrieved January 20, 2011.
- ↑ Curtis, John (June 20, 1998). "Hunting Down HIV". Yale Medicine.
- ↑ Soderstrom, E John (July 10, 2003). "National Institutes of Health: Moving Research from the Bench to the Bedside".
- ↑ Cohen, Elizabeth (September 29, 2014). "Doctor treats Ebola with HIV drug in Liberia -- seemingly successfully". CNN.
- ↑ HIV drug may stop Ebola. Operonlabs.com, 27 September 2014
External links
- Epivir (manufacturer's website)
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||