Visual processing abnormalities in schizophrenia
Schizophrenia is a complex mental disorder with a heterogeneous set of symptoms. Scientists have identified visual processing abnormalities in this disorder by studying the behavior and physiology of subjects with schizophrenia, and have proposed this as a topic meriting further investigation.[1] There is evidence that schizophrenia affects perception of contrast[1][2][3][4][5][6][7][8][9][10][11][12][13] and motion,[1][14][15][16][17][18] control of eye movements,[19][20][21][22] detection of visual contours,[1][23][24][25][26][27][28][29] and recognition of faces [30][31][32][33] or facial expressions.[34][35][36][37] The specificity of many visual processing abnormalities in schizophrenia is still an area of active debate within the scientific community.[8][9][32][33][34][35][36][38]
Perception of Contrast
Contrast Sensitivity
Contrast is a feature of visual stimuli that characterizes the difference in brightness between dark and light regions of an image. Perception of contrast is affected by the temporal frequency and spatial frequency properties of a stimulus, and the sensitivity to contrast in sine wave stimuli is characterized by the Contrast sensitivity function. Contrast sensitivity has been shown to be impaired in schizophrenia.[2][3][4][5][6][7][8][9][10] There is evidence that these impairments may be more severe among patients with predominantly Negative symptoms,[2][5][6][7] or those who are not medicated.[10] Butler and colleagues[8][9] have proposed that patients with schizophrenia may have a specific deficit in the magnocellular visual processing pathway, and electroencephalography (EEG) data have been presented that may support this view.[9] Results from pharmacological studies in cats[1] have demonstrated the role of NMDA in contrast perception of magnocellular-tuned stimuli. Application of drugs that deactivate this glutamate receptor type led to reduced neural responses in the visual system of cats, and some argue this suppression is similar to the reduced behavioral responses observed among patients with schizophrenia. They claim these results are consistent with the glutamate hypothesis of schizophrenia,[1] which proposes that dysfunction in this neurotransmitter system leads to abnormal neural activity underlying this disorder. Skottun and colleagues[38] dispute the magnocellular deficit theory however, saying that there is not enough evidence from different research groups to support it, and that the experiments focused on this topic have shown very mixed results.
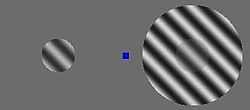
Surround Suppression
The perceived contrast of a stimulus is sometimes suppressed when another stimulus is presented surrounding it, an effect known as surround suppression (see Figure 1), which is similar to the simultaneous contrast illusion. In schizophrenia, estimations of perceived contrast in surround suppression are less suppressed than for healthy adults.[11][12][13] Further, the magnitude of this perceptual suppression effect has been shown to correlate with the concentration of γ-aminobutyric acid or GABA, an inhibitory neurotransmitter in visual cortex.[13] These results may illustrate the role of GABA in mechanisms that regulate the overall level of neural activity[39] in visual cortex, and it has been suggested that such mechanisms may be disrupted in schizophrenia.[1] Such a disruption would be consistent with the GABA hypothesis of schizophrenia,[40][41] which states that dysfunctional GABAergic inhibition may disrupt neural activity in subjects with this disorder, and this in turn may lead to visual processing abnormalities.[13]
Motion Processing
Motion perception is an important visual function and occurs from the earliest stages of cortical visual processing, with individual neurons being tuned to a preferred direction of motion.[42] The cortical area MT (medial temporal cortex, also known as V5) plays a significant role in motion processing, and deactivation of this region using Transcranial magnetic stimulation can affect perception of motion.[43] Subjects with schizophrenia have shown abnormalities in perceptual judgments of motion, speed and direction,[14][15][16][17][18][20][44][45] with deficits in these judgments generally being reported. It has been suggested that these findings are related to the aforementioned magnocellular deficit purported to exist in this disorder.[45] Inhibition of motion perception by the addition of a surround stimulus has also been examined in schizophrenia, with one group finding evidence both of impaired motion perception and weaker perceptual suppression effects in schizophrenia.[18] This agrees with the findings mentioned previously related to weaker suppression of perceived contrast in this disorder.[11][12][13] However, another recent report has disputed this finding, instead showing evidence consistent with stronger surround influence on motion perception in schizophrenia.[17]
Eye Movements
Eye movements are important behaviors for locating and tracking objects in the visual world. Two of the major types of eye movements are saccades and smooth pursuit. Saccades are very rapid and precise eye movements between two positions, and are important in establishing fixation. Smooth pursuit on the other hand, allows the viewer to track a moving object along its trajectory within the visual field. Deficits in eye movement behavior among patients with schizophrenia have been reported since the beginning of the 20th century.[19] Genetic factors are believed to be involved in these abnormalities, as unaffected relatives of schizophrenia patients show similar dysfunction.[19] Specifically, saccade abnormalities have been observed in this disorder, with patients showing changes in saccade rate, amplitude and accuracy.[19] Such deficits have been linked to medication with lithium, as well as damage in frontal lobe regions.[19] Further, patients with schizophrenia often exhibit errors in smooth pursuit eye movements.[19][20][21][22] The neural correlates of smooth pursuit behavior in schizophrenia have been studied using functional Magnetic Resonance Imaging (fMRI), with abnormal activation having been observed in multiple cortical regions implicated in motion processing, such as Frontal Eye Fields and area MT.[21] Some have speculated that errors in smooth pursuit in this disorder may depend on deficits in frontal lobe processing, such as errors in anticipating the direction of stimulus motion, and that this in turn may be consistent with working memory deficits in schizophrenia.[19][22] Others have disputed this claim, presenting evidence instead pointing to the aforementioned deficits in motion processing, and abnormalities in cortical area MT as a possible source of smooth pursuit errors.[20] In this experiment, it was found that motion perception and smooth pursuit task performance were correlated, but no relationship between measures of smooth pursuit and attention was observed.
Contour Detection
Detecting visual contours, edges, or boundaries is an important function in human and computer vision which facilitates figure-ground segmentation and object recognition. Contour integration depends on a subject’s ability to link representations of separate visual stimuli into a coherent percept. Subjects with schizophrenia have been shown to perform worse than healthy adults on tasks that depend on contour integration,[1][23][24][25][26][27][28][29] and these deficits may be related to factors such as illness severity, chronicity, and degree of disorganized symptoms.[1] In these experiments, subjects often viewed stimuli that could be connected to form a coherent perception of a line, like a simplified connect the dots puzzle. It is worth noting that in general, the magnitude of visual processing abnormalities (such as abnormal contour detection performance) in schizophrenia are fairly small. Therefore it may be necessary to examine experimental data from a large number of subjects in order to observe difference between healthy adults and those with schizophrenia using statistical methods. It has been proposed that weaker lateral excitation due to deficient NMDA-receptor functioning could disrupt neural processing, and that this might underlie problems with contour integration in schizophrenia. This idea is consistent with the Glutamate hypothesis of schizophrenia,[1] as dysfunction in this neurotransmitter system may explain symptoms observed in this disorder.
Presentation of collinear stimuli flanking a target can enhance responses to the target in cortex, an effect known as flanker or collinear facilitation, which has been shown to be weaker in schizophrenia subjects than in healthy adults or those with bipolar disorder.[26] Publications from multiple research groups indicate that schizophrenia patients perform more poorly than healthy adults when asked to identify contours composed of separated line segments embedded in backgrounds made up of randomly oriented segments.[23][24][25][28][29] This includes evidence from an fMRI experiment indicating abnormally reduced activation in visual areas V2-4.[25] Another group used EEG to examine illusory contour processing deficits in schizophrenia.[27] They found decreased amplitude and altered source location for the P1 component in patients, which they claim reflects abnormal dorsal stream processing in this disorder.
Crowding Phenomenon
Crowding refers to the phenomenon where recognition of visual stimuli presented in the periphery is impaired by the presence of other nearby objects (sometimes called "flankers"). Abnormal crowding has been observed in schizophrenia, with different groups reporting stronger[46] or weaker[28] crowding effects.
Perception of Faces and Facial Emotions
Faces
Face perception is a function of the visual system which is critical for social behavior. Patients with schizophrenia have shown abnormalities in tasks designed to probe facial processing and recognition.[30][31][32][33] Specifically, performance deficits have been observed in this disorder when subjects were asked to identify degraded pictures of faces, and the deficits observed were specific to patients with predominantly disorganized symptoms.[31] Another experiment using the same stimuli during EEG found poorer performance and slower reaction times among patients with schizophrenia, as well as abnormalities in beta band activity.[30] The authors state that these results are related to deficits in long range coordination of neural activity, as described for contour detection. Another experiment using EEG and structural MRI to examine facial processing abnormalities in schizophrenia found decreased N170 component responses in patients, and this was correlated with decreased gray matter volumes in the fusiform gyrus.[32] There is evidence that the fusiform face area is a visual cortical region that may be specialized for detecting faces. The authors of this study conclude that their data support a specific face processing deficit in schizophrenia. However, another study using fractured images of faces found that patients with schizophrenia were better than healthy adults at identifying images of famous people that had been distorted.[33] These experiments state that this may be evidence of weaker "configural" processing in schizophrenia patients, who instead may rely more on local image features for face identification, as these were preserved in their image manipulation.
Facial Emotions
Recognizing emotional expressions in images of human faces is a particularly important component of face perception with clear implications in human social interactions. People with schizophrenia reportedly perform poorly compared with healthy adults when asked to identify facial emotions.[34][35][36][37] Some researchers have claimed that this is not a deficit specific to facial emotion perception per se, but rather evidence of a generalized deficit or overall poorer task performance in schizophrenia.[34][35] However, others have argued that a review of the literature shows evidence of an additional specific deficit in processing negative emotions, such as anger and fear, among patients with schizophrenia.[36] In addition, evidence has been presented of a link between a specific emotion processing deficit in schizophrenia and the volume of temporal lobe structures, including fusiform gyrus and middle temporal gyrus, as measured using MRI.[37]
See also
- Schizophrenia
- Mechanisms of schizophrenia
- Causes of schizophrenia
- Diagnosis of schizophrenia
- Visual perception
- Visual system
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Butler, P. D., Silverstein, S. M., & Dakin, S. C. (2008). "Visual perception and its impairment in schizophrenia". Biological Psychiatry 64 (1): 40–47. doi:10.1016/j.biopsych.2008.03.023. PMC 2435292. PMID 18549875.
- ↑ 2.0 2.1 2.2 Slaghuis, W.L. (1998). "Contrast sensitivity for stationary and drifting spatial frequency gratings in positive- and negative-symptom schizophrenia". Journal of Abnormal Psychology 107 (1): 49–62. doi:10.1037/0021-843X.107.1.49. PMID 9505038.
- ↑ 3.0 3.1 Chen, Y., Nakayama, K., Levy, D. L., Matthysse, S., & Holzman, P. S. (1999). "Psychophysical isolation of a motion-processing deficit in schizophrenics and their relatives and its association with impaired smooth pursuit". Proceedings of the National Academy of Sciences 96 (8): 4724. doi:10.1073/pnas.96.8.4724.
- ↑ 4.0 4.1 Keri, S., Antal, A., Szekeres, G., Benedek, G., & Janka, Z. (2002). "Spatiotemporal visual processing in schizophrenia". Journal of Neuropsychiatry and Clinical Neurosciences 14 (2): 190–6. doi:10.1176/appi.neuropsych.14.2.190. PMID 11983794.
- ↑ 5.0 5.1 5.2 Slaghuis, W.L. & Bishop, A.M. (2001). "Luminance flicker sensitivity in positive- and negative-symptom schizophrenia". Experimental Brain Research 138: 88–99. doi:10.1007/s002210100683.
- ↑ 6.0 6.1 6.2 Slaghuis, W.L., & Thompson, A. K. (2003). "The effect of peripheral visual motion on focal contrast sensitivity in positive-and negative-symptom schizophrenia". Neuropsychologia 41 (8): 968–980. doi:10.1016/S0028-3932(02)00321-4. PMID 12667532.
- ↑ 7.0 7.1 7.2 Slaghuis, Walter L. (2004). "Spatio-temporal luminance contrast sensitivity and visual backward masking in schizophrenia". Experimental Brain Research 156 (2): 196–211. doi:10.1007/s00221-003-1771-3.
- ↑ 8.0 8.1 8.2 8.3 Butler; P. D.; Zemon; V.; Schechter; I.; Saperstein; A. M.; Hoptman (2005). "Early-stage visual processing and cortical amplification deficits in schizophrenia". Archives of General Psychiatry 62 (5): 495–504. doi:10.1001/archpsyc.62.5.495. PMC 1298183. PMID 15867102.
- ↑ 9.0 9.1 9.2 9.3 9.4 Butler; P. D.; Martinez; A.; Foxe; J. J.; Kim; D.; Zemon (2007). "Subcortical visual dysfunction in schizophrenia drives secondary cortical impairments". Brain 130 (2): 417. doi:10.1093/brain/awl233.
- ↑ 10.0 10.1 10.2 O’Donnell, B. F., Bismark, A., Hetrick, W. P., Bodkins, M., Vohs, J. L., & Shekhar, A. (2006). "Early stage vision in schizophrenia and schizotypal personality disorder". Schizophrenia research 86 (1–3): 89–98. doi:10.1016/j.schres.2006.05.016. PMID 16829048.
- ↑ 11.0 11.1 11.2 Dakin, S., Carlin, P., & Hemsley, D. (2005). "Weak suppression of visual context in chronic schizophrenia". Current Biology 16 (20): R822–R824. doi:10.1016/j.cub.2005.10.015.
- ↑ 12.0 12.1 12.2 Yoon, J. H., Rokem, A. S., Silver, M. A., Minzenberg, M. J., Ursu, S., Ragland, J. D., & Carter, C. S. (2009). "Diminished Orientation-Specific Surround Suppression of Visual Processing in Schizophrenia". Schizophrenia Bulletin 35 (6): 1078–1084. doi:10.1093/schbul/sbp064. PMC 2762622. PMID 19620601.
- ↑ 13.0 13.1 13.2 13.3 13.4 Yoon, J. H., Maddock, R. J., Rokem, A. S., Silver, M. A., Minzenberg, M. J., Ragland, J. D., & Carter, C. S. (2010). "GABA Concentration Is Reduced in Visual Cortex in Schizophrenia and Correlates with Orientation-Specific Surround Suppression". Journal of Neuroscience 30 (10): 3777–3781. doi:10.1523/JNEUROSCI.6158-09.2010. PMC 2846788. PMID 20220012.
- ↑ 14.0 14.1 Li, C. S. R. (2002). "Impaired detection of visual motion in schizophrenia patients". Progress in neuro-psychopharmacology and biological psychiatry 26 (5): 929–934. doi:10.1016/S0278-5846(02)00207-5. PMID 12369268.
- ↑ 15.0 15.1 Chen, Y., Palafox, G. P., Nakayama, K., Levy, D. L., Matthysse, S., & Holzman, P. S. (1999). "Motion perception in schizophrenia". Archives of General Psychiatry 56 (2): 149–54. doi:10.1001/archpsyc.56.2.149. PMID 10025439.
- ↑ 16.0 16.1 Chen, Y., Nakayama, K., Levy, D., Matthysse, S., & Holzman, P. (2003). "Processing of global, but not local, motion direction is deficient in schizophrenia". Schizophrenia research 61 (2–3): 215–227. doi:10.1016/S0920-9964(02)00222-0. PMID 12729873.
- ↑ 17.0 17.1 17.2 Chen, Y., Norton, D., & Ongur, D. (2008). "Altered center-surround motion inhibition in schizophrenia". Biological Psychiatry 64 (2): 74–77. doi:10.1016/j.biopsych.2007.11.017.
- ↑ 18.0 18.1 18.2 Tadin, D., Kim, J., Doop, M. L., Gibson, C., Lappin, J. S., Blake, R., & Park, S. (2006). "Weakened Center-Surround Interactions in Visual Motion Processing in Schizophrenia". Journal of Neuroscience 26 (44): 11403–11412. doi:10.1523/JNEUROSCI.2592-06.2006. PMID 17079669.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 Abel, L. A., Levin, S., & Holzman, P. S. (1992). "Abnormalities of Smooth Pursuit and Saccadic Control in Schizophrenia and Affective Disorders". Vision Research 32 (6): 1009–1014. doi:10.1016/0042-6989(92)90002-Z. PMID 1509692.
- ↑ 20.0 20.1 20.2 20.3 Stuve, T., Friedman, L., Jesberger, J., Gilmore, G., Strauss, M., & Meltzer, H. (2004). "The relationship between smooth pursuit performance, motion perception and sustained visual attention in patients with schizophrenia and normal controls". Psychological Medicine 27 (1): 143–152. PMID 9122294.
- ↑ 21.0 21.1 21.2 Hong, L. E., Tagamets, M., Avila, M., Wonodi, I., Holcomb, H., & Thaker, G. K. (2005). "Specific motion processing pathway deficit during eye tracking in schizophrenia: a performance-matched functional magnetic resonance imaging study". Biological Psychiatry 57 (7): 726–732. doi:10.1016/j.biopsych.2004.12.015. PMID 15820229.
- ↑ 22.0 22.1 22.2 Avila, M. T.; Hong, LE; Moates, A; Turano, KA; Thaker, GK (2005). "Role of Anticipation in Schizophrenia-Related Pursuit Initiation Deficits". Journal of Neurophysiology 95 (2): 593–601. doi:10.1152/jn.00369.2005. PMID 16267121.
- ↑ 23.0 23.1 23.2 Silverstein, S. M., Kovács, I., Corry, R., & Valone, C. (2000). "Perceptual organization, the disorganization syndrome, and context processing in chronic schizophrenia". Schizophrenia research 43 (1): 11–20. doi:10.1016/S0920-9964(99)00180-2. PMID 10828411.
- ↑ 24.0 24.1 24.2 Silverstein; S.; Hatashita-Wong; M.; Schenkel; L.; Wilkniss; S.; Kovács (2006). "Reduced top-down influences in contour detection in schizophrenia". Cognitive neuropsychiatry 11 (2): 112–132. doi:10.1080/13546800444000209. PMID 16537237.
- ↑ 25.0 25.1 25.2 25.3 Silverstein, S. M., Berten, S., Essex, B., Kovács, I., Susmaras, T., & Little, D. M. (2009). "An fMRI Examination of Visual Integration in Schizophrenia". Journal of Integrative Neuroscience 8 (2): 175–202. doi:10.1142/S0219635209002113. PMID 19618486.
- ↑ 26.0 26.1 26.2 Keri, S., Kelemen, O., Benedek, G., & Janka, Z. (2005). "Lateral interactions in the visual cortex of patients with schizophrenia and bipolar disorder". Psychological Medicine 35 (7): 1043–1051. doi:10.1017/S0033291705004381. PMID 16045070.
- ↑ 27.0 27.1 27.2 Foxe, J. J., Murray, M. M., & Javitt, D. C. (2005). "Filling-in in schizophrenia: a high-density electrical mapping and source-analysis investigation of illusory contour processing". Cerebral Cortex 15 (12): 1914–27. doi:10.1093/cercor/bhi069. PMID 15772373.
- ↑ 28.0 28.1 28.2 28.3 Robol V., Tibber M.S., Anderson E.J., Bobin T., Carlin P., Shergill S.S., Dakin S.C. (2013). "Reduced crowding and poor contour detection in schizophrenia are consistent with weak surround inhibition.". PLOS ONE 8 (4): e60951. doi:10.1371/journal.pone.0060951. PMC 3621669. PMID 23585865.
- ↑ 29.0 29.1 29.2 Schallmo, M-P., Sponheim, S. R., Olman, C. A. (2013). "Abnormal Contextual Modulation of Visual Contour Detection in Patients with Schizophrenia". PLOS ONE 8 (6): e68090. doi:10.1371/journal.pone.0068090. PMC 3688981. PMID 23922637.
- ↑ 30.0 30.1 30.2 Uhlhaas, P. J., Linden, D. E. J., Singer, W., Haenschel, C., Lindner, M., Maurer, K., & Rodriguez, E. (2006). "Dysfunctional long-range coordination of neural activity during Gestalt perception in schizophrenia". Journal of Neuroscience 26 (31): 8168–75. doi:10.1523/JNEUROSCI.2002-06.2006. PMID 16885230.
- ↑ 31.0 31.1 31.2 Uhlhaas, P. J., Phillips, W. A., Mitchell, G., & Silverstein, S. M. (2006). "Perceptual grouping in disorganized schizophrenia". Psychiatry Research 145 (2–3): 105–117. doi:10.1016/j.psychres.2005.10.016. PMID 17081620.
- ↑ 32.0 32.1 32.2 32.3 Onitsuka; T.; Niznikiewicz; M. A.; Spencer; K. M.; Frumin; M.; Kuroki (2006). "Functional and structural deficits in brain regions subserving face perception in schizophrenia". American Journal of Psychiatry 163 (3): 455–62. doi:10.1176/appi.ajp.163.3.455. PMC 2773688. PMID 16513867.
- ↑ 33.0 33.1 33.2 33.3 Joshua, N., & Rossell, S. (1962). "Configural face processing in schizophrenia". Schizophrenia research 112 (1–3): 99–103. doi:10.1016/j.schres.2009.03.033. PMID 19419842.
- ↑ 34.0 34.1 34.2 34.3 Kerr, S.L. & Neale, J.M. (1993). "Emotion Perception in Schizophrenia: Specific Deficit or Further Evidence of Generalized Poor Performance". Journal of Abnormal Psychology 102 (2): 312–318. doi:10.1037/0021-843X.102.2.312. PMID 8315144.
- ↑ 35.0 35.1 35.2 35.3 Salem, J.E., Kring, A.M., & Kerr, S.L. (1996). "More Evidence for Generalized Poor Performance in Facial Emotion Perception in Schizophrenia". Journal of Abnormal Psychology 105 (3): 480–483. doi:10.1037/0021-843X.105.3.480. PMID 8772021.
- ↑ 36.0 36.1 36.2 36.3 Mandal, M. K., Pandey, R., & Prasad, A. B. (1998). "Facial expressions of emotions and schizophrenia: A review". Schizophrenia Bulletin 24 (3): 399–412. doi:10.1093/oxfordjournals.schbul.a033335. PMID 9718632.
- ↑ 37.0 37.1 37.2 Goghari, V. M., MacDonald, A. W., & Sponheim, S. R. (2011). "Temporal Lobe Structures and Facial Emotion Recognition in Schizophrenia Patients and Nonpsychotic Relatives". Schizophrenia Bulletin 37 (6): 1281–1294. doi:10.1093/schbul/sbq046. PMC 3196942. PMID 20484523.
- ↑ 38.0 38.1 Skottun, B. C., & Skoyles, J. R. (2007). "Contrast sensitivity and magnocellular functioning in schizophrenia". Vision research 47 (23): 2923–2933. doi:10.1016/j.visres.2007.07.016. PMID 17825350.
- ↑ Heeger, D. J. (1992). "Normalization of Cell Responses in Cat Striate Cortex". Visual Neuroscience 9 (2): 181–197. doi:10.1017/S0952523800009640. PMID 1504027.
- ↑ Lewis, D. A., Hashimoto, T., & Volk, D. W. (2005). "Cortical Inhibitory Neurons and Schizophrenia". Nature Reviews Neuroscience 6 (4): 312–324. doi:10.1038/nrn1648. PMID 15803162.
- ↑ Gonzalez-Burgos, G., & Lewis, D. A. (2008). "GABA neurons and the mechanisms of network oscillations: implications for understanding cortical dysfunction in schizophrenia". Schizophrenia Bulletin 34 (5): 944–61. doi:10.1093/schbul/sbn070. PMC 2518635. PMID 18586694.
- ↑ Hubel, D. H., & Wiesel, T. N. (1962). "Receptive fields, binocular interaction and functional architecture in the cat's visual cortex". The Journal of Physiology 160 (1): 106.
- ↑ Tadin, D., Silvanto, J., Pascual-Leone, A., & Battelli, L. (2011). "Weakened Improved Motion Perception and Impaired Spatial Suppression following Disruption of Cortical Area MT/V5". Journal of Neuroscience 31 (4): 1279–83. doi:10.1523/JNEUROSCI.4121-10.2011. PMC 3078722. PMID 21273412.
- ↑ Chen, Y., Levy, D. L., Sheremata, S., & Holzman, P. S. (2004). "Compromised late-stage motion processing in schizophrenia". Biological Psychiatry 55 (8): 834–841. doi:10.1016/j.biopsych.2003.12.024. PMID 15050865.
- ↑ 45.0 45.1 Kim, D., Wylie, G., Pasternak, R., Butler, P. D., & Javitt, D. C. (2006). "Magnocellular contributions to impaired motion processing in schizophrenia". Schizophrenia research 82 (1): 1–8. doi:10.1016/j.schres.2005.10.008. PMC 2045640. PMID 16325377.
- ↑ Kraehenmann, R., Vollenweider F.X., Seifritz E., Kometer, M. (2012). "Crowding deficits in the visual periphery of schizophrenia patients". PLoS ONE 7 (9): e45884. doi:10.1371/journal.pone.0045884. PMC 3458825. PMID 23049884.