Type I hypersensitivity
| Type I hypersensitivity | |
|---|---|
 | |
| Classification and external resources | |
| MeSH | D006969 |
Type I hypersensitivity (or immediate hypersensitivity) is an allergic reaction provoked by reexposure to a specific type of antigen referred to as an allergen.[1] Type I is not to be confused with Type II, Type III, or Type IV hypersensitivities.
Exposure may be by ingestion, inhalation, injection, or direct contact.
Pathophysiology
In type 1 hypersensitivity, an antigen is presented to CD4+ Th2 cells specific to the antigen that stimulate B-cell production of IgE antibodies also specific to the antigen. The difference between a normal infectious immune response and a type 1 hypersensitivity response is that in type 1 hypersensitivity the antibody is IgE instead of IgA, IgG, or IgM. During sensitisation, the IgE antibodies bind to Fcε receptors on the surface of tissue mast cells and blood basophils.[2] Mast cells and basophils coated by IgE antibodies are "sensitised." Later exposure to the same allergen cross-links the bound IgE on sensitised cells, resulting in degranulation and the secretion of pharmacologically active mediators such as histamine, leukotriene (LTC4 and LTD4), and prostaglandin that act on the surrounding tissues. The principal effects of these products are vasodilation and smooth-muscle contraction.
Type 1 hypersensitivity can be further classified into an immediate and late-phase reaction. The immediate hypersensitivity reaction occurs minutes after exposure and includes release of vasoactive amines and lipid mediators, whereas the late-phase reaction occurs 2–4 hours after exposure and includes the release of cytokines.[3]
| Vasodilation and increased permeability |
| |
|---|---|---|
| Smooth muscle spasm |
| |
| Leukocyte extravasation |
| |
| Unless otherwise specified, the reference for this table is:[4] | ||
The reaction may be either local or systemic. Symptoms vary from mild irritation to sudden death from anaphylactic shock.
Treatment and prognosis
Treatment usually involves adrenaline (epinephrine), antihistamines, and corticosteroids. If the entire body gets involved, then anaphylaxis can take place, which is an acute, systemic reaction that can prove fatal.
Examples
Some examples:
- Allergic asthma
- Allergic conjunctivitis
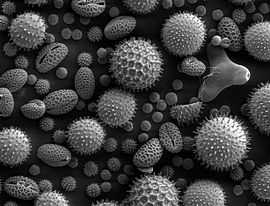
- Allergic rhinitis ("hay fever")
- Anaphylaxis
- Angioedema
- Urticaria (hives)
- Eosinophilia
- Penicillin allergy
- Cephalosporin allergy
- Food allergy
See also
References
- ↑ med/1101 at eMedicine
- ↑ "The Adaptive Immune System: Type I Immediate Hypersensitivity". Retrieved 2008-09-22.
- ↑ Shiv Pillai MD; Abul K. Abbas MBBS; Andrew Wilson PhD (2011). Cellular and Molecular Immunology: with STUDENT CONSULT Online Access. Philadelphia: Saunders. ISBN 1-4377-1528-1.
- ↑ Table 5-2 in:Mitchell, Richard Sheppard; Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson. Robbins Basic Pathology. Philadelphia: Saunders. ISBN 1-4160-2973-7. 8th edition.
External links
- Type I hypersensitivity (Flash Animation)
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||