Surgery


Surgery (from the Greek: χειρουργική cheirourgikē (composed of χείρ, "hand", and ἔργον, "work"), via Latin: chirurgiae, meaning "hand work") is an ancient medical specialty that uses operative manual and instrumental techniques on a patient to investigate and/or treat a pathological condition such as disease or injury, to help improve bodily function or appearance or to repair unwanted ruptured areas (for example, a perforated ear drum).
An act of performing surgery may be called a surgical procedure, operation, or simply surgery. In this context, the verb operate means to perform surgery. The adjective surgical means pertaining to surgery; e.g. surgical instruments or surgical nurse. The patient or subject on which the surgery is performed can be a person or an animal. A surgeon is a person who practises surgery and a surgeon's assistant is a person who practices surgical assistance. A surgical team is made up of surgeon, surgeon's assistant, anesthesia provider, circulating nurse and surgical technologist. Surgery usually spans minutes to hours, but it is typically not an ongoing or periodic type of treatment. The term surgery can also refer to the place where surgery is performed, or simply the office of a physician, dentist, or veterinarian.
Elective surgery generally refers to a surgical procedure that can be scheduled in advance because it does not involve a medical emergency. Plastic, or cosmetic surgeries are common elective procedures.
Definitions
Surgery is a technology consisting of a physical intervention on tissues, and muscle.
As a general rule, a procedure is considered surgical when it involves cutting of a patient's tissues or closure of a previously sustained wound. Other procedures that do not necessarily fall under this rubric, such as angioplasty or endoscopy, may be considered surgery if they involve "common" surgical procedure or settings, such as use of a sterile environment, anesthesia, antiseptic conditions, typical surgical instruments, and suturing or stapling. All forms of surgery are considered invasive procedures; so-called "noninvasive surgery" usually refers to an excision that does not penetrate the structure being excised (e.g. laser ablation of the cornea) or to a radiosurgical procedure (e.g. irradiation of a tumor).
Types of surgery
Surgical procedures are commonly categorized by urgency, type of procedure, body system involved, degree of invasiveness, and special instrumentation.
- Based on timing: Elective surgery is done to correct a non-life-threatening condition, and is carried out at the patient's request, subject to the surgeon's and the surgical facility's availability. Emergency surgery is surgery which must be done promptly to save life, limb, or functional capacity. A semi-elective surgery is one that must be done to avoid permanent disability or death, but can be postponed for a short time.
- Based on purpose: Exploratory surgery is performed to aid or confirm a diagnosis. Therapeutic surgery treats a previously diagnosed condition.
- By type of procedure: Amputation involves cutting off a body part, usually a limb or digit; castration is also an example. Resection is the removal of all or part of an internal organ or part of the body. Replantation involves reattaching a severed body part. Reconstructive surgery involves reconstruction of an injured, mutilated, or deformed part of the body. Cosmetic surgery is done to improve the appearance of an otherwise normal structure. Excision is the cutting out or removal of an organ, tissue, or other body part from the patient. Transplant surgery is the replacement of an organ or body part by insertion of another from different human (or animal) into the patient. Removing an organ or body part from a live human or animal for use in transplant is also a type of surgery.
- By body part: When surgery is performed on one organ system or structure, it may be classed by the organ, organ system or tissue involved. Examples include cardiac surgery (performed on the heart), gastrointestinal surgery (performed within the digestive tract and its accessory organs), and orthopedic surgery (performed on bones and/or muscles).
- By degree of invasiveness: Minimally invasive surgery involves smaller outer incision(s) to insert miniaturized instruments within a body cavity or structure, as in laparoscopic surgery or angioplasty. By contrast, an open surgical procedure or laparotomy requires a large incision to access the area of interest.
- By equipment used: Laser surgery involves use of a laser for cutting tissue instead of a scalpel or similar surgical instruments. Microsurgery involves the use of an operating microscope for the surgeon to see small structures. Robotic surgery makes use of a surgical robot, such as the Da Vinci or the Zeus surgical systems, to control the instrumentation under the direction of the surgeon.
Terminology
- Excision surgery names often start with a name for the organ to be excised (cut out) and end in -ectomy.
- Procedures involving cutting into an organ or tissue end in -otomy. A surgical procedure cutting through the abdominal wall to gain access to the abdominal cavity is a laparotomy.
- Minimally invasive procedures involving small incisions through which an endoscope is inserted end in -oscopy. For example, such surgery in the abdominal cavity is called laparoscopy.
- Procedures for formation of a permanent or semi-permanent opening called a stoma in the body end in -ostomy.
- Reconstruction, plastic or cosmetic surgery of a body part starts with a name for the body part to be reconstructed and ends in -oplasty. Rhino is used as a prefix for "nose", therefore a rhinoplasty is reconstructive or cosmetic surgery for the nose.
- Repair of damaged or congenital abnormal structure ends in -rraphy. Herniorraphy is the reparation of a hernia, while perineorraphy is the reparation of perineum.
- Reoperation (return to the operating room) refers to a return to the operating theater after an initial surgery is performed to re-address an aspect of patient care best treated surgically. Reasons for reoperation include persistent bleeding after surgery, development of or persistence of infection or, more insidiously, retained foreign objects.
Description of surgical procedure
Location
At a hospital, modern surgery is often done in an operating theater using surgical instruments, an operating table for the patient, and other equipment. The environment and procedures used in surgery are governed by the principles of aseptic technique: the strict separation of "sterile" (free of microorganisms) things from "unsterile" or "contaminated" things. All surgical instruments must be sterilized, and an instrument must be replaced or re-sterilized if it becomes contaminated (i.e. handled in an unsterile manner, or allowed to touch an unsterile surface). Operating room staff must wear sterile attire (scrubs, a scrub cap, a sterile surgical gown, sterile latex or non-latex polymer gloves and a surgical mask), and they must scrub hands and arms with an approved disinfectant agent before each procedure. There is moderate-quality evidence that usage of two layers of gloves compared to single gloving during surgery reduces perforations and blood stains on the skin, indicating a decrease in percutaneous exposure incidents.[1]
Patient Safety
The Agency for Healthcare and Research Quality suggests that patients should ask your doctor questions.
Preoperative care
Prior to surgery, the patient is given a medical examination, certain pre-operative tests, and their physical status is rated according to the ASA physical status classification system. If these results are satisfactory, the patient signs a consent form and is given a surgical clearance. If the procedure is expected to result in significant blood loss, an autologous blood donation may be made some weeks prior to surgery. If the surgery involves the digestive system, the patient may be instructed to perform a bowel prep by drinking a solution of polyethylene glycol the night before the procedure. Patients are also instructed to abstain from food or drink (an NPO order after midnight on the night before the procedure), to minimize the effect of stomach contents on pre-operative medications and reduce the risk of aspiration if the patient vomits during or after the procedure.
Some medical systems have a practice of routinely performing chest x-rays before surgery. The premise behind this practice is that the physician might discover some unknown medical condition which would complicate the surgery, and that upon discovering this with the chest x-ray, the physician would adapt the surgery practice accordingly.[2] In fact, medical specialty professional organizations recommend against routine pre-operative chest x-rays for patients who have an unremarkable medical history and presented with a physical exam which did not indicate a chest x-ray.[2] Routine x-ray examination is more likely to result in problems like misdiagnosis, overtreatment, or other negative outcomes than it is to result in a benefit to the patient.[2] Likewise, other tests including complete blood count, prothrombin time, partial thromboplastin time, basic metabolic panel, and urinalysis should not be done unless the results of these tests can help evaluate surgical risk.[3]
Staging for surgery
In the pre-operative holding area, the patient changes out of his or her street clothes and is asked to confirm the details of his or her surgery. A set of vital signs are recorded, a peripheral IV line is placed, and pre-operative medications (antibiotics, sedatives, etc.) are given. When the patient enters the operating room, the skin surface to be operated on, called the operating field, is cleaned and prepared by applying an antiseptic such as chlorhexidine gluconate or povidone-iodine to reduce the possibility of infection. If hair is present at the surgical site, it is clipped off prior to prep application. The patient is assisted by an anesthesiologist or resident to make a specific surgical position, then sterile drapes are used to cover all of the patient's body except for the head and the surgical site or at least a wide area surrounding the operating field; the drapes are clipped to a pair of poles near the head of the bed to form an "ether screen", which separates the anesthetist/anesthesiologist's working area (unsterile) from the surgical site (sterile).
Anesthesia is administered to prevent pain from incision, tissue manipulation and suturing. Based on the procedure, anesthesia may be provided locally or as general anesthesia. Spinal anesthesia may be used when the surgical site is too large or deep for a local block, but general anesthesia may not be desirable. With local and spinal anesthesia, the surgical site is anesthetized, but the patient can remain conscious or minimally sedated. In contrast, general anesthesia renders the patient unconscious and paralyzed during surgery. The patient is intubated and is placed on a mechanical ventilator, and anesthesia is produced by a combination of injected and inhaled agents. Choice of surgical method and anaesthetic technique aims to reduce risk of complications, shorten time needed for recovery and minimise the surgical stress response.
Surgery
An incision is made to access the surgical site. Blood vessels may be clamped or cauterized to prevent bleeding, and retractors may be used to expose the site or keep the incision open. The approach to the surgical site may involve several layers of incision and dissection, as in abdominal surgery, where the incision must traverse skin, subcutaneous tissue, three layers of muscle and then peritoneum. In certain cases, bone may be cut to further access the interior of the body; for example, cutting the skull for brain surgery or cutting the sternum for thoracic (chest) surgery to open up the rib cage. Whilst in surgery health and safety is used to prevent infection or further spreading of the disease. The surgeon will remove hair from the face and eyes, using a head hat. Hands, wrists and forearms are washed thoroughly to prevent germs getting into the operated body, then gloves are placed onto the hands. A PVC apron will be worn at all times, to stop any contamination. A yellow substance – typically an antiseptic iodine solution – is lighly coated onto the located area of the patient's body that will be performed on, this stops germs and disease infecting areas of the body, whilst the patient is being cut into.
Work to correct the problem in body then proceeds. This work may involve:
- excision – cutting out an organ, tumor,[4] or other tissue.
- resection – partial removal of an organ or other bodily structure.
- reconnection of organs, tissues, etc., particularly if severed. Resection of organs such as intestines involves reconnection. Internal suturing or stapling may be used. Surgical connection between blood vessels or other tubular or hollow structures such as loops of intestine is called anastomosis.
- Reduction – the movement or realignment of a body part to its normal position. e.g. Reduction of a broken nose involves the physical manipulation of the bone and/or cartilage from their displaced state back to their original position to restore normal airflow and aesthetics.
- ligation – tying off blood vessels, ducts, or "tubes".
- grafts – may be severed pieces of tissue cut from the same (or different) body or flaps of tissue still partly connected to the body but resewn for rearranging or restructuring of the area of the body in question. Although grafting is often used in cosmetic surgery, it is also used in other surgery. Grafts may be taken from one area of the patient's body and inserted to another area of the body. An example is bypass surgery, where clogged blood vessels are bypassed with a graft from another part of the body. Alternatively, grafts may be from other persons, cadavers, or animals.
- insertion of prosthetic parts when needed. Pins or screws to set and hold bones may be used. Sections of bone may be replaced with prosthetic rods or other parts. Sometime a plate is inserted to replace a damaged area of skull. Artificial hip replacement has become more common. Heart pacemakers or valves may be inserted. Many other types of prostheses are used.
- creation of a stoma, a permanent or semi-permanent opening in the body
- in transplant surgery, the donor organ (taken out of the donor's body) is inserted into the recipient's body and reconnected to the recipient in all necessary ways (blood vessels, ducts, etc.).
- arthrodesis – surgical connection of adjacent bones so the bones can grow together into one. Spinal fusion is an example of adjacent vertebrae connected allowing them to grow together into one piece.
- modifying the digestive tract in bariatric surgery for weight loss.
- repair of a fistula, hernia, or prolapse
- other procedures, including:
- clearing clogged ducts, blood or other vessels
- removal of calculi (stones)
- draining of accumulated fluids
- debridement- removal of dead, damaged, or diseased tissue
- Surgery has also been conducted to separate conjoined twins.
- Sex change operations
Blood or blood expanders may be administered to compensate for blood lost during surgery. Once the procedure is complete, sutures or staples are used to close the incision. Once the incision is closed, the anesthetic agents are stopped and/or reversed, and the patient is taken off ventilation and extubated (if general anesthesia was administered).[5]
Post-operative care
After completion of surgery, the patient is transferred to the post anesthesia care unit and closely monitored. When the patient is judged to have recovered from the anesthesia, he/she is either transferred to a surgical ward elsewhere in the hospital or discharged home. During the post-operative period, the patient's general function is assessed, the outcome of the procedure is assessed, and the surgical site is checked for signs of infection. There are several risk factors associated with postoperative complications, such as immune deficienty and obesity. Obesity has long been considered a risk factor for adverse post-surgical outcomes. It has been linked to many disorders such as obesity hypoventilation syndrome, atelectasis and pulmonary embolism, adverse cardiovascular effects, and wound healing complications.[6] If removable skin closures are used, they are removed after 7 to 10 days post-operatively, or after healing of the incision is well under way.
It is not uncommon for surgical drains (see Drain (surgery)) to be required to remove blood or fluid from the surgical wound during recovery. Mostly these drains stay in until the volume tapers off, then they are removed. These drains can become clogged, leading to retained blood complications or abscess.
Postoperative therapy may include adjuvant treatment such as chemotherapy, radiation therapy, or administration of medication such as anti-rejection medication for transplants. Other follow-up studies or rehabilitation may be prescribed during and after the recovery period.
The use of topical antibiotics on surgical wounds does not reduce infection rates in comparison with non-antibiotic ointment or no ointment at all.[7] Antibiotic ointments will irritate the skin, slow healing, and greatly increase risk of developing contact dermatitis and antibiotic resistance.[7] Because of this, they should only be used when a person shows signs of infection and not as a preventative.[7]
Through a retrospective analysis of national administrative data, the association between mortality and day of elective surgical procedure suggests a higher risk in procedures carried out later in the working week and on weekends. The odds of death were 44% and 82% higher respectively when comparing procedures on a Friday to a weekend procedure. This “weekday effect” has been postulated to be from several factors including poorer availability of services on a weekend, and also, decrease number and level of experience over a weekend.[8]
Epidemiology
Of the 38.6 million hospital stays that occurred in U.S. hospitals in 2011, 29% included at least one operating room procedure. These stays accounted for 48% of the total $387 billion in hospital costs.[9]
In total, there were over 15 million operating room procedures performed in U.S. hospitals in 2011. The overall number of procedures remained stable from 2001-2011.[10]
A study of data from 2003-2011 showed that U.S. hospital costs were highest for the surgical service line; the surgical service line costs were $17,600 in 2003 and projected to be $22,500 in 2013.[11] For hospital stays in 2012 in the United States, private insurance had the highest percentage of surgical expenditure.[12] Mean hospital costs in the United States in 2012 were highest for surgical stays.[12]
In special populations
Elderly people
Older adults have widely varying physical health. Frail elderly people are at significant risk of post-surgical complications and the need for extended care. Assessment of older patients before elective surgeries can accurately predict the patients' recovery trajectories.[13] One frailty scale uses five items: unintentional weight loss, muscle weakness, exhaustion, low physical activity, and slowed walking speed. A healthy person scores 0; a very frail person scores 5. Compared to non-frail elderly people, people with intermediate frailty scores (2 or 3) are twice as likely to have post-surgical complications, spend 50% more time in the hospital, and are three times as likely to be discharged to a skilled nursing facility instead of to their own homes.[13] Frail elderly patients (score of 4 or 5) have even worse outcomes, with the risk of being discharged to a nursing home rising to twenty times the rate for non-frail elderly people.
Other populations
- Children
Surgery on children requires considerations which are not common in adult surgery. Children and adolescents are still developing physically and mentally making it difficult for them to make informed decisions and give consent for surgical treatments. Bariatric surgery in youth is among the controversial topics related to surgery in children.
- Persons with health conditions
A person with a debilitating medical condition may have special needs during a surgery which a typical patient would not.
- Vulnerable populations
Doctors perform surgery with the consent of the patient. Some patients are able to give better informed consent than others. Populations such as incarcerated persons, the mentally incompetent, persons subject to coercion, and other people who are not able to make decisions with the same authority as a typical patient have special needs when making decisions about their personal healthcare, including surgery.
History
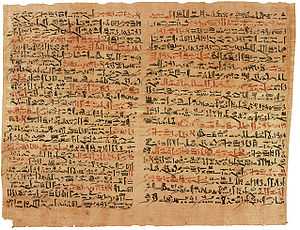
Surgical treatments date back to the prehistoric era. The oldest for which there is evidence is trepanation,[14] in which a hole is drilled or scraped into the skull, thus exposing the dura mater in order to treat health problems related to intra cranial pressure and other diseases. Prehistoric surgical techniques are seen in Ancient Egypt, where a mandible dated to approximately 2650 BCE shows two perforations just below the root of the first molar, indicating the draining of an abscessed tooth. Remains from the early Harappan periods of the Indus Valley Civilization (c. 3300 BCE) show evidence of teeth having been drilled dating back 9,000 years.[15] Instruments resembling surgical tools have also been found in the archaeological sites of Bronze Age China dating from the Shang Dynasty, along with seeds likely used for herbalism.[16]

The oldest known surgical texts date back to ancient Egypt about 3500 years ago. Surgical operations were performed by priests, specialized in medical treatments similar to today.[17] and the use of sutures to close wounds.[18] Infections were treated with honey.[19] In ancient Greece, temples dedicated to the healer-god Asclepius, known as Asclepieia (Greek: Ασκληπιεία, sing. Asclepieion Ασκληπιείον), functioned as centers of medical advice, prognosis, and healing.[20] In the Asclepieion of Epidaurus, some of the surgical cures listed, such as the opening of an abdominal abscess or the removal of traumatic foreign material, are realistic enough to have taken place.[5] The Greek Galen was one of the greatest surgeons of the ancient world and performed many audacious operations—including brain and eye surgery—that were not tried again for almost two millennia.

In the Middle East, surgery was developed to a high degree in the Islamic world. Abulcasis (Abu al-Qasim Khalaf ibn al-Abbas Al-Zahrawi), an Andalusian-Arab physician and scientist who practised in the Zahra suburb of Córdoba, wrote medical texts that influenced European surgical procedures.[21]
In Europe, the demand grew for surgeons to formally study for many years before practicing; universities such as Montpellier, Padua and Bologna were particularly renowned. In the 15th century, Rogerius Salernitanus composed his Chirurgia, laying the foundation for modern Western surgical manuals. Barber-surgeons generally had a bad reputation that was not to improve until the development of academic surgery as a specialty of medicine, rather than an accessory field.[22] Basic surgical principles for asepsis etc., are known as Halsteads principles.
Early modern Europe

There were some important advances to the art of surgery during this period. The professor of anatomy at the University of Padua, Andreas Vesalius, was a pivotal figure in the Renaissance transition from classical medicine and anatomy based on the works of Galen, to an empirical approach of 'hands-on' dissection. In his anatomic treatis, De humani corporis fabrica, he exposed the many anatomical errors in Galen and advocated that all surgeons should train by engaging in practical dissections themselves.
The second figure of importance in this era was Ambroise Paré (sometimes spelled "Ambrose"[23]), a French army surgeon from the 1530s until his death in 1590. The practice for cauterizing gunshot wounds on the battlefield had been to use boiling oil; an extremely dangerous and painful procedure. Paré began to employ a less irritating emollient, made of egg yolk, rose oil and turpentine. He also described more efficient techniques for the effective ligation of the blood vessels during an amputation.
Modern surgery

The discipline of surgery was put on a sound, scientific footing during the Age of Enlightenment in Europe. An important figure in this regard was the English surgical scientist, John Hunter, generally regarded as the father of modern scientific surgery.[24] He brought an empirical and experimental approach to the science and was renowned around Europe for the quality of his research and his written works. Hunter reconstructed surgical knowledge from scratch; refusing to rely on the testimonies of others he conducted his own surgical experiments to determine the truth of the matter. To aid comparative analysis, he built up a collection of over 13,000 specimens of separate organ systems, from the simplest plants and animals to humans.
He greatly advanced knowledge of venereal disease and introduced many new techniques of surgery, including new methods for repairing damage to the Achilles tendon and a more effective method for applying ligature of the arteries in case of an aneurysm.[25] He was also one of the first to understand the importance of pathology, the danger of the spread of infection and how the problem of inflammation of the wound, bone lesions and even tuberculosis often undid any benefit that was gained from the intervention. He consequently adopted the position that all surgical procedures should be used only as a last resort.[26]
Other important 18th and early 19th century surgeons included Percival Pott (1713 -1788) who described tuberculosis on the spine and first demonstrated that a cancer may be caused by an environmental carcinogen - (he noticed a connection between chimney sweep's exposure to soot and their high incidence of scrotal cancer. Astley Paston Cooper (1768-1841) first performed a successful ligation of the abdominal aorta, and James Syme (1799-1870) pioneered the Symes Amputation for the ankle joint and successfully carried out the first hip disarticulation.
Modern pain control through anesthesia was discovered in the mid-19th century. Before the advent of anesthesia, surgery was a traumatically painful procedure and surgeons were encouraged to be as swift as possible to minimize patient suffering. This also meant that operations were largely restricted to amputations and external growth removals. Beginning in the 1840s, surgery began to change dramatically in character with the discovery of effective and practical anaesthetic chemicals such as ether, first used by the American surgeon Crawford Long, and chloroform, discovered by James Young Simpson and later pioneered by John Snow, physician to Queen Victoria.[27] In addition to relieving patient suffering, anaesthesia allowed more intricate operations in the internal regions of the human body. In addition, the discovery of muscle relaxants such as curare allowed for safer applications.
Infection and antisepsis
Unfortunately, the introduction of anesthetics encouraged more surgery, which inadvertently caused more dangerous patient post-operative infections. The concept of infection was unknown until relatively modern times. The first progress in combating infection was made in 1847 by the Hungarian doctor Ignaz Semmelweis who noticed that medical students fresh from the dissecting room were causing excess maternal death compared to midwives. Semmelweis, despite ridicule and opposition, introduced compulsory handwashing for everyone entering the maternal wards and was rewarded with a plunge in maternal and fetal deaths, however the Royal Society dismissed his advice.

Until the pioneering work of British surgeon Joseph Lister in the 1860s, most medical men believed that chemical damage from exposures to bad air (see "miasma") was responsible for infections in wounds, and facilities for washing hands or a patient's wounds were not available.[28] Lister became aware of the work of French chemist Louis Pasteur, who showed that rotting and fermentation could occur under anaerobic conditions if micro-organisms were present. Pasteur suggested three methods to eliminate the micro-organisms responsible for gangrene: filtration, exposure to heat, or exposure to chemical solutions. Lister confirmed Pasteur's conclusions with his own experiments and decided to use his findings to develop antiseptic techniques for wounds. As the first two methods suggested by Pasteur were inappropriate for the treatment of human tissue, Lister experimented with the third, spraying carbolic acid on his instruments. He found that this remarkably reduced the incidence of gangrene and he published his results in The Lancet. [29] Later, on 9 August 1867, he read a paper before the British Medical Association in Dublin, on the Antiseptic Principle of the Practice of Surgery, which was reprinted in The British Medical Journal.[30][31][32] His work was groundbreaking and laid the foundations for a rapid advance in infection control that saw modern antiseptic operating theatres widely used within 50 years.
Lister continued to develop improved methods of antisepsis and asepsis when he realised that infection could be better avoided by preventing bacteria from getting into wounds in the first place. This led to the rise of sterile surgery. Lister introduced the Steam Steriliser to sterilize equipment, instituted rigorous hand washing and later implemented the wearing of rubber gloves. These three crucial advances - the adoption of a scientific methodology toward surgical operations, the use of anaesthetic and the introduction of sterilised equipment - laid the groundwork for the modern invasive surgical techniques of today.
The use of X-rays as an important medical diagnostic tool began with their discovery in 1895 by German physicist Wilhelm Röntgen. He noticed that these rays could penetrate the skin, allowing the skeletal structure to be captured on a specially treated photographic plate.
Surgical specialties
- General surgery
- craniofacial surgery
- Dental surgery
- Gynaecology
- Neurosurgery
- Ophthalmology
- Oral and maxillofacial surgery
- Orthopaedic surgery
- Otolaryngology
- Podiatric surgery
- Urology
Diagnoses and treatments that involve the use of invasive methods – such as catheterization and endoscopy – are also sometimes considered to be "surgery" or "surgical", although not by most of the medical profession.
See also
- Anesthesia
- ASA physical status classification system or pre-operative physical fitness
- Biomaterial
- Cardiac surgery
- Surgical drain
- Endoscopy
- Fluorescence image-guided surgery
- Hypnosurgery
- Jet ventilation
- List of surgical procedures
- Minimally invasive procedure
- Operative report
- Perioperative mortality
- Robotic surgery
- Surgeon's assistant
- Surgical Outcomes Analysis and Research
- Surgical Sieve
- Trauma surgery
- Reconstructive surgery
- WHO Surgical Safety Checklist
National Societies
- American College of Surgeons
- American College of Osteopathic Surgeons
- American Academy of Orthopedic Surgeons
- American College of Foot and Ankle Surgeons
- Royal Australasian College of Surgeons
- Royal Australasian College of Dental Surgeons
- Royal College of Physicians and Surgeons of Canada
- Royal College of Surgeons in Ireland
- Royal College of Surgeons of Edinburgh
- Royal College of Physicians and Surgeons of Glasgow
- Royal College of Surgeons of England
Qualifications in the UK and Ireland
Notes and references
- ↑ Mischke, Christina; Verbeek, Jos H; Saarto, Annika; Lavoie, Marie-Claude; Pahwa, Manisha; Ijaz, Sharea; Verbeek, Jos H (2014). "Gloves, extra gloves or special types of gloves for preventing percutaneous exposure injuries in healthcare personnel". doi:10.1002/14651858.CD009573.pub2.
- ↑ 2.0 2.1 2.2 American College of Radiology. "Five Things Physicians and Patients Should Question". Choosing Wisely: an initiative of the ABIM Foundation (American College of Radiology). Retrieved August 17, 2012, citing
- "American College of Radiology ACR Appropriateness Criteria". American College of Radiology. 2000. Retrieved 4 September 2012. Last reviewed 2011.
- Gómez-Gil, E.; Trilla, A.; Corbella, B.; Fernández-Egea, E.; Luburich, P.; De Pablo, J.; Ferrer Raldúa, J.; Valdés, M. (2002). "Lack of clinical relevance of routine chest radiography in acute psychiatric admissions". General hospital psychiatry 24 (2): 110–113. doi:10.1016/s0163-8343(01)00179-7. PMID 11869746.
- Archer, C.; Levy, A. R.; McGregor, M. (1993). "Value of routine preoperative chest x-rays: A meta-analysis". Canadian Journal of Anaesthesia 40 (11): 1022–1027. doi:10.1007/BF03009471. PMID 8269561.
- Munro, J.; Booth, A.; Nicholl, J. (1997). "Routine preoperative testing: A systematic review of the evidence". Health technology assessment (Winchester, England) 1 (12): i–iv; 1–62. PMID 9483155.
- Grier, D. J.; Watson, L. J.; Hartnell, G. G.; Wilde, P. (1993). "Are routine chest radiographs prior to angiography of any value?". Clinical radiology 48 (2): 131–133. doi:10.1016/S0009-9260(05)81088-8. PMID 8004892.
- Gupta, S. D.; Gibbins, F. J.; Sen, I. (1985). "Routine chest radiography in the elderly". Age and ageing 14 (1): 11–14. doi:10.1093/ageing/14.1.11. PMID 4003172.
- Amorosa JK; Bramwit MP; Mohammed TL; Reddy GP et al. "ACR Appropriateness Criteria routine chest radiographs in ICU patients.". National Guideline Clearinghouse. Retrieved 4 September 2012.
- ↑ American Society for Clinical Pathology, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Society for Clinical Pathology), retrieved August 1, 2013, which cites
- Keay, L.; Lindsley, K.; Tielsch, J.; Katz, J.; Schein, O. (2009). Keay, Lisa, ed. "Routine preoperative medical testing for cataract surgery". The Cochrane Library (2): CD007293. doi:10.1002/14651858.CD007293.pub2. PMID 19370681.
- Katz, R. I.; Dexter, F.; Rosenfeld, K.; Wolfe, L.; Redmond, V.; Agarwal, D.; Salik, I.; Goldsteen, K.; Goodman, M.; Glass, P. S. A. (2011). "Survey Study of Anesthesiologistsʼ and Surgeonsʼ Ordering of Unnecessary Preoperative Laboratory Tests". Anesthesia & Analgesia 112 (1): 207–212. doi:10.1213/ANE.0b013e31820034f0. PMID 21081771.
- Munro, J.; Booth, A.; Nicholl, J. (1997). "Routine preoperative testing: A systematic review of the evidence". Health technology assessment (Winchester, England) 1 (12): i–iv; 1–62. PMID 9483155.
- Reynolds, T. M.; National Institute for Health Clinical Excellence; Clinical Scince Reviews Committee of the Association for Clinical Biochemistry (2006). "National Institute for Health and Clinical Excellence guidelines on preoperative tests: The use of routine preoperative tests for elective surgery". Annals of Clinical Biochemistry 43 (Pt 1): 13–16. doi:10.1258/000456306775141623. PMID 16390604.
- Capdenat Saint-Martin, E.; Michel, P.; Raymond, J. M.; Iskandar, H.; Chevalier, C.; Petitpierre, M. N.; Daubech, L.; Amouretti, M.; Maurette, P. (1998). "Description of local adaptation of national guidelines and of active feedback for rationalising preoperative screening in patients at low risk from anaesthetics in a French university hospital". Quality in health care : QHC 7 (1): 5–11. doi:10.1136/qshc.7.1.5. PMC 2483578. PMID 10178152.
- ↑ Wagman LD. "Principles of Surgical Oncology" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ↑ 5.0 5.1 Askitopoulou, H., Konsolaki, E., Ramoutsaki, I., Anastassaki, E. Surgical cures by sleep induction as the Asclepieion of Epidaurus. The history of anesthesia: proceedings of the Fifth International Symposium, by José Carlos Diz, Avelino Franco, Douglas R. Bacon, J. Rupreht, Julián Alvarez. Elsevier Science B.V., International Congress Series 1242(2002), p.11-17.
- ↑ Doyle, S. L., Lysaght, J. and Reynolds, J. V. (2010), Obesity and post-operative complications in patients undergoing non-bariatric surgery. Obesity Reviews, 11: 875–886.
- ↑ 7.0 7.1 7.2 American Academy of Dermatology (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Academy of Dermatology), retrieved 5 December 2013, which cites
- Sheth, V. M.; Weitzul, S. (2008). "Postoperative topical antimicrobial use". Dermatitis : contact, atopic, occupational, drug 19 (4): 181–189. PMID 18674453.
- ↑ Aylin P, Alexandrescu R, Jen MH, Mayer EK, Bottle A (2013). "Day of week of procedure and 30 day mortality for elective surgery: retrospective analysis of hospital episode statistics". BMJ 346: f2424. doi:10.1136/bmj.f2424. PMC 3665889. PMID 23716356.
- ↑ Weiss AJ, Elixhauser A, Andrews RM. (February 2014). "Characteristics of Operating Room Procedures in U.S. Hospitals, 2011.". HCUP Statistical Brief #170. Rockville, MD: Agency for Healthcare Research and Quality.
- ↑ Weiss AJ, Elixhauser A. (March 2014). "Trends in Operating Room Procedures in U.S. Hospitals, 2001—2011.". HCUP Statistical Brief #171. Rockville, MD: Agency for Healthcare Research and Quality.
- ↑ Weiss AJ, Barrett ML, Steiner CA (July 2014). "Trends and Projections in Inpatient Hospital Costs and Utilization, 2003-2013". HCUP Statistical Brief #175. Rockville, MD: Agency for Healthcare Research and Quality.
- ↑ 12.0 12.1 Moore B, Levit K and Elixhauser A (October 2014). "Costs for Hospital Stays in the United States, 2012". HCUP Statistical Brief #181. Rockville, MD: Agency for Healthcare Research and Quality.
- ↑ 13.0 13.1 Makary MA, Segev DL, Pronovost PJ et al. (June 2010). "Frailty as a predictor of surgical in older patients". J. Am. Coll. Surg. 210 (6): 901–8. doi:10.1016/j.jamcollsurg.2010.01.028. PMID 20510798. Lay summary (28 December 2010).
- ↑ Capasso, Luigi (2002). Principi di storia della patologia umana: corso di storia della medicina per gli studenti della Facoltà di medicina e chirurgia e della Facoltà di scienze infermieristiche (in Italian). Rome: SEU. ISBN 88-87753-65-2. OCLC 50485765.
- ↑ "Stone age man used dentist drill". BBC News. 6 April 2006. Retrieved 24 May 2010.
- ↑ Hong, Francis (2004). "History of Medicine in China" (PDF). McGill Journal of Medicine 8 (1): 7984.
- ↑ Shiffman, Melvin. Cosmetic Surgery: Art and Techniques. Springer. p. 20. ISBN 978-3-642-21837-8.
- ↑ R. Sullivan "The Identity and Work of the Ancient Egyptian Surgeon". Journal of the Royal Society of Medicine. 89, no 8 (1996): 469.
- ↑ James P. Allen, "The Art of Medicine in Ancient Egypt". (New York: The Metropolitan Museum of Art, 2005), 72.
- ↑ Risse, G.B. Mending bodies, saving souls: a history of hospitals. Oxford University Press, 1990. p. 56
- ↑ biography from Famousmuslims.com accessed 16 April 2007.
- ↑ Sven Med Tidskr. (2007). "From barber to surgeon- the process of professionalization". Svensk medicinhistorisk tidskrift 11 (1): 69–87. PMID 18548946.
- ↑ Levine JM (March 1992). "Historical notes on pressure ulcers: the cure of Ambrose Paré". Decubitus 5 (2): 23–4, 26. PMID 1558689.
- ↑ Moore, Wendy (2005). The Knife Man: The Extraordinary Life and Times of John Hunter, Father of Modern Surgery. Crown Publishing Group. Retrieved 2013-02-07.
- ↑ "John Hunter: "the father of scientific surgery": Resources from the collection of the P.I. Nixon Library". Retrieved 2012-12-17.
- ↑ "John Hunter: ‘Founder of Scientific Surgery’". Retrieved 2012-12-17.
- ↑ Gordon, H. Laing (November 2002). Sir James Young Simpson and Chloroform (1811–1870). The Minerva Group, Inc. p. 108. ISBN 978-1-4102-0291-8. Retrieved 11 November 2011.
- ↑ Robinson, Victor. The Story Of Medicine. Kessinger Publishing. p. 420.
- ↑ The Lancet, "On a new method of treating compound fracture, abscess, etc.: with observation on the conditions of suppuration".
5 articles running from:
Volume 89, Issue 2272, 16 March 1867, Pages 326-329 (Originally published as Volume 1, Issue 2272)
to:
Volume 90, Issue 2291, 27 July 1867, Pages 95-96 Originally published as Volume 2, Issue 2291 - ↑ Lister J (21 September 1867). "On the Antiseptic Principle in the Practice of Surgery". The British Medical Journal 2 (351): 245–260. doi:10.1136/bmj.2.351.246. PMC 2310614. PMID 20744875.. Reprinted in Lister, BJ (2010). "The classic: On the antiseptic principle in the practice of surgery. 1867". Clinical orthopaedics and related research 468 (8): 2012–6. doi:10.1007/s11999-010-1320-x. PMC 2895849. PMID 20361283.
- ↑ Lister, Joseph. "Modern History Sourcebook: Joseph Lister (1827-1912): Antiseptic Principle Of The Practice Of Surgery, 1867". Fordham University. Retrieved 2 September 2011.Modernized version of text
- ↑ Lister, Joseph. "On the Antiseptic Principle of the Practice of Surgery by Baron Joseph Lister". Project Gutenberg. Retrieved 2 September 2011. E-text, audio at Project Gutenberg.
External links
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||