Strychnine
 | |
 | |
| Names | |
|---|---|
| Other names
Strychnidin-10-one | |
| Identifiers | |
| 57-24-9 (base) 60-41-3 (sulfate) | |
| ChEBI | CHEBI:28973 |
| ChEMBL | ChEMBL227934 ChEMBL612118 ChEMBL486399 |
| ChemSpider | 389877 |
| |
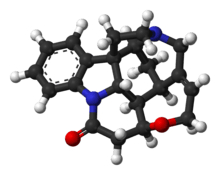
| Jmol-3D images | Image |
| KEGG | C06522 |
| PubChem | 441071 |
| |
| UNII | H9Y79VD43J |
| Properties | |
| Molecular formula |
C21H22N2O2 |
| Molar mass | 334.41 g·mol−1 |
| Appearance | white or translucent crystal or crystalline powder; Bitter tasting |
| Odor | Odorless |
| Density | 1.36 g cm−3 |
| Melting point | 543 K (270 °C) |
| Boiling point | 557−559 K (284−286 °C) |
| Acidity (pKa) | 8.25[1] |
| Except where noted otherwise, data is given for materials in their standard state (at 25 °C (77 °F), 100 kPa) | |
| | |
| Infobox references | |
Strychnine (/ˈstrɪkniːn/; also US /ˈstrɪknaɪn/ or /ˈstrɪknɪn/) is a highly toxic (LD50 = 0.16 mg/kg in rats, 1–2 mg/kg orally in humans[2]), colorless, bitter crystalline alkaloid used as a pesticide, particularly for killing small vertebrates such as birds and rodents. Strychnine, when inhaled, swallowed or absorbed through eyes or mouth, causes a poisoning which results in muscular convulsions and eventually death through asphyxia.[3] The most common source is from the seeds of the Strychnos nux-vomica tree.
History
Strychnine was the first alkaloid to be identified in plants of the genus Strychnos, family Loganiaceae. Strychnos, named by Carl Linnaeus in 1753, is a genus of trees and climbing shrubs of the gentian order. The genus contains 196 various species and is distributed throughout the warm regions of Asia (58 species), America (64 species), and Africa (75 species). The seeds and bark of many plants in this genus contain the powerful poison strychnine.
The toxic and medicinal effects of Strychnos nux-vomica have been well known from the times of ancient India, although the chemical compound itself was not identified and characterized until the 19th century. The inhabitants of these countries had historical knowledge of the species Strychnos nux-vomica and Saint-Ignatius’ bean (Strychnos ignatii). Strychnos nux-vomica is a tree native to the tropical forests on the Malabar Coast in Southern India, Sri Lanka and Indonesia, which attains a height of about 12 m. The tree has a crooked, short, thick trunk and the wood is close grained and very durable. The fruit has an orange color and is about the size of a large apple with a hard rind and contains five seeds, which are covered with a soft wool-like substance. The ripe seeds look like flattened disks, which are very hard. These seeds are the chief commercial source of strychnine and were first imported to and marketed in Europe as a poison to kill rodents and small predators. Strychnos ignatii is a woody climbing shrub of the Philippines. The fruit of the plant, known as Saint Ignatius' bean, contains as many as 25 seeds embedded in the pulp. The seeds contain more strychnine than other commercial alkaloids. The properties of S. nux-vomica and S. ignatii are substantially those of the alkaloid strychnine.
Strychnine was first discovered by French chemists Joseph Bienaimé Caventou and Pierre-Joseph Pelletier in 1818 in the Saint-Ignatius’ bean.[4] In some Strychnos plants a 9,10-dimethoxy derivative of strychnine, the alkaloid brucine, is also present. Brucine is not as poisonous as strychnine. Historic records indicate that preparations containing strychnine (presumably) had been used to kill dogs, cats, and birds in Europe as far back as 1640. The structure of strychnine was first determined in 1946 by Sir Robert Robinson and in 1954 this alkaloid was synthesized in a laboratory by Robert B. Woodward. This is one of the most famous syntheses in the history of organic chemistry. Both chemists won the Nobel prize (Robinson in 1947 and Woodward in 1965).[5]
Biosynthesis

Strychnine is a terpene indole alkaloid belonging to the Strychnos family of Corynanthe alkaloids, and it is derived from tryptamine and secologanin.[6][7] The enzyme, strictosidine synthase, catalyzes the condensation of tryptamine and secologanin, followed by a Pictet-Spengler reaction to form strictosidine.[8] While the enzymes that catalyze the following steps have not been identified, the steps have been inferred by isolation of intermediates from Strychnos nux vomica.[9] The next step is hydrolysis of the acetal, which opens the ring by elimination of glucose (O-Glu) and provides a reactive aldehyde. The nascent aldehyde is then attacked by a secondary amine to afford geissoschizine, a common intermediate of many related compounds in the Strychnos family.[6]
A reverse Pictet-Spengler reaction cleaves the C2-C3 bond, while a subsequent Mannich reaction forms the C3-C7 bond, and a Michael addition forms the C2-C16 bond to provide dehydropreakuammicine. Hydrolysis of the methyl ester and decarboxylation leads to norfluorocurarine. Stereospecific reduction of the endocyclic double bond by NADPH and hydroxylation provides the Wieland-Gumlich aldehyde, which was first isolated by Heimberger and Scott in 1973, although previously synthesized by Wieland and Gumlich in 1932.[9][10] To elongate the appendage by 2 carbons, acetyl-CoA is added to the aldehyde in an aldol reaction to afford prestrychnine. Strychnine is then formed by a facile addition of the amine with the carboxylic acid or its activated CoA thioester, followed by ring-closure via displacement of an activated alcohol.
Chemical synthesis
As early researchers have noted, the strychnine molecular structure, with its specific array of rings, stereocenters, and nitrogen functional groups is a complex synthetic target, and has stimulated interest for that reason and for interest in the structure-activity relationships underlying its pharmacologic activities.[11] An early synthetic chemist targeting strychnine, R.B. Woodward, quoted the chemist who determined its structure through chemical decomposition and related physical studies as saying that "for its molecular size it is the most complex [organic] substance known" (attributed to Sir Robert Robinson).[12]
The first total synthesis of strychnine was reported by the research group of R.B. Woodward in 1954, and is considered a classic in this field.[13][14] The Woodward account published in 1954 was very brief (3 pp.),[15] but was followed by a 42-page report in 1963.[16] The molecule has since received continuing wide attention in the years since for the challenges to synthetic organic strategy and tactics presented by its complexity; its synthesis has been targeted and its stereocontrolled preparation independently achieved by more than a dozen research groups since the first success (see main strychnine total synthesis article).
ADME
Absorption
Strychnine may be introduced into the body orally, by inhalation, or by injection. It is a potently bitter substance, and in humans has been shown to activate bitter taste receptors TAS2R10 and TAS2R46.[17][18][19] Strychnine is rapidly absorbed from the gastrointestinal tract.
Distribution
Strychnine is transported by plasma and erythrocytes. Due to slight protein binding, strychnine leaves the bloodstream quickly and distributes to the tissues. Approximately 50% of the ingested dose can enter the tissues in 5 minutes. Also within a few minutes of ingestion, strychnine can be detected in the urine. Little difference was noted between oral and intramuscular administration of strychnine. In persons killed by strychnine, the highest concentrations are found in the blood, liver, kidney and stomach wall. The usual fatal dose is 60–100 mg strychnine and is fatal after a period of 1–2 hours, though lethal doses vary depending on the individual.
Metabolism
Strychnine is rapidly metabolized by the liver microsomal enzyme system requiring NADPH and O2. Strychnine competes with the inhibitory neurotransmitter glycine resulting in an excitatory state. However, the toxicokinetics after overdose have not been well described. In most severe cases of strychnine poisoning, the patient dies before reaching the hospital. The biological half-life of strychnine is about 10 hours. This half-life suggests that normal hepatic function can efficiently degrade strychnine even when the quantity ingested is high enough to cause severe poisoning.
Excretion
A few minutes after ingestion, strychnine is excreted unchanged in the urine, and accounts for about 5 to 15% of a sublethal dose given over 6 hours. Approximately 10 to 20% of the dose will be excreted unchanged in the urine in the first 24 hours. The percentage excreted decreases with the increasing dose. Of the amount excreted by the kidneys, about 70% is excreted in the first 6 hours, and almost 90% in the first 24 hours. Excretion is almost complete in 48 to 72 hours.[5]
Mechanism of action
Strychnine is a neurotoxin which acts as an antagonist of glycine and acetylcholine receptors. It primarily affects the motor nerves in the spinal cord which control muscle contraction. An impulse is triggered at one end of a nerve by the binding of neurotransmitters to the receptors. In the presence of a neuroinhibitor, such as glycine, a greater quantity of excitatory neurotransmitters must bind to receptors before there will be an action potential generated. Glycine acts primarily as an agonist of the glycine receptor, which is a ligand-gated chloride channel in neurons located in the spinal cord and in the brain. This chloride channel will allow the negatively charged chloride ions into the neuron, causing a hyperpolarization which pushes the membrane potential further from threshold. Strychnine is an antagonist of glycine, which means it binds to the same receptor, preventing the inhibitory effects of glycine on the postsynaptic neuron. Therefore, action potentials are triggered with lower levels of excitatory neurotransmitters. When the inhibitory signals are prevented, the motor neurons are more easily activated and the victim will have spastic muscle contractions, resulting in death by asphyxiation.[3][20] Structure of strychnine in complex with ACh binding protein (AChBP).[21]
Toxicity
Strychnine is very toxic to humans and many other animals, and poisoning by inhalation, swallowing or absorption through eyes or mouth can be fatal. S. nux-vomica seeds are generally effective only when they are crushed or chewed before swallowing because the pericarp is quite hard and indigestible; poisoning symptoms may therefore not appear if the seeds are ingested whole.
Animal toxicity
Strychnine poisoning in animals usually occurs from ingestion of baits designed for use against gophers, moles and coyotes. Strychnine is also used as a rodenticide, but is not specific for such unwanted pests and may kill other small animals. In the United States, most baits containing strychnine have been replaced with zinc phosphide baits since 1990. In the Netherlands rodenticides with strychnine are forbidden.
Strychnine toxicity in rats is dependent on sex. It is more toxic to females than to males when administered via subcutaneous injection or intraperitoneal injection. Differences are due to higher rates of metabolism by male rat liver microsomes. Dogs and cats are more susceptible among domestic animals, pigs are believed to be as susceptible as dogs, and horses are able to tolerate relatively large amounts of strychnine. Birds affected by strychnine poisoning exhibit wing droop, salivation, tremors, muscle tenseness and convulsions. Death occurs as a result of respiratory arrest. The clinical signs of strychnine poisoning relate to its effects on the central nervous system. The first clinical signs of poisoning include nervousness, restlessness, twitching of the muscles, and stiffness of the neck. As the poisoning progresses, the muscular twitching becomes more pronounced and convulsions suddenly appear in all the skeletal muscles. The limbs are extended and the neck is curved to opisthotonus. The pupils are widely dilated. As death approaches, the convulsions follow one another with increased rapidity, severity, and duration. Death results from asphyxia due to prolonged paralysis of the respiratory muscles. Following the ingestion of strychnine, symptoms of poisoning usually appear within 15 to 60 min. The LD50-values for strychnine in animals are listed below in table 1.
| The LD50 values for strychnine in animals | ||
|---|---|---|
| Organism | Route | LD50 (mg/kg) |
| Bird-wild[22] | Oral | 16 |
| Cat[23] | Intravenous | 0.33 |
| Cat[24] | Oral | 0.5 |
| Dog[25] | Intravenous | 0.8 |
| Dog[23] | Subcutaneous | 0.35 |
| Dog[24] | Oral | 0.5 |
| Duck[22] | Oral | 3.0 |
| Mouse[26] | Intraperitoneal | 0.98 |
| Mouse[27] | Intravenous | 0.41 |
| Mouse[28] | Oral | 2.0 |
| Mouse[29] | Parenteral | 1.06 |
| Mouse[30] | Subcutaneous | 0.47 |
| Pigeon[22] | Oral | 21.0 |
| Quail[22] | Oral | 23.0 |
| Rabbit[25] | Intravenous | 0.4 |
| Rabbit[23] | Oral | 0.6 |
| Rat[31] | Oral | 16.0 |
| Rat[32] | Oral | 2.35 |
Human toxicity
The symptoms of poisoning in humans are generally similar to those as in other animals, because the mechanism of action is apparently similar across species. The toxicity of strychnine in humans is not ethically studied, so most information known comes from cases of strychnine poisoning, unintentional and deliberate.
The following symptoms are indicative of a lethal dose:
- Severe nausea, including vomiting
- Convulsions of all muscle groups, which become longer and more closely spaced with time
- Spasms of the facial muscles, causing cyanosis of the face, dilated pupils, prominent eyeballs, and frothing at the mouth
- The body may exhibit the following "arching"/"bridging" postures:
- Opisthotonus: Hyperextension. The person may be resting on heels and occiput.
- Emprosthotonos: The spasm of abdominal muscles may bend the body forward.
- Pleurothotonus: The body may be flexed to one side.
- Loss of consciousness and a clear mind
- Immense reflex sensitivity (dramatic exaggeration of normal reflexes)
- Death due to asphyxiation, caused by muscle spasms[3]
The LD50-values estimated from different cases of strychnine poisoning are listed below in table 2.
| The LD50 values for strychnine in humans | ||
|---|---|---|
| Route | LD50 (mg) | |
| Human[33][34] | Oral | 100–120 |
| Human[35] | Oral | 30–60 |
| Human (child)[36][37][38] | Oral | 15 |
| Human (adult)[39] | Oral | 50–100 |
| Human (adult)[38] | Oral | 30–100 |
| Human (adult)[37] | Oral | 30 |
| Human[40] | Intravenously | 5–10 (approximate) |
For occupational exposures to strychnine, the Occupational Safety and Health Administration and National Institute for Occupational Safety and Health have set exposure limits at 0.15 mg/m3 over an 8-hour work day.[41]
Because strychnine produces some of the most dramatic and painful symptoms of any known toxic reaction, strychnine poisoning is often portrayed in literature and film.
Treatment
There is no specific antidote for strychnine but recovery from strychnine exposure is possible with early hospital treatment. Treatment consists of removing the drug from the body (decontamination) and getting supportive medical care in a hospital setting. Supportive care includes intravenous fluids, medications against convulsions and spasms, and cooling measures for high temperature. The patient should be kept in a quiet and darkened room, because excessive manipulation and loud noises may cause convulsions. Because these convulsions are extremely painful, an appropriate painkiller should be given. Treatment of strychnine poisoning involves an oral administration of activated charcoal which adsorbs any strychnine within the digestive tract. Unabsorbed strychnine can be removed from the stomach by gastric lavage with tannic acid or potassium permanganate solutions to oxidize strychnine. Seizures are controlled by anticonvulsants, such as phenobarbital or diazepam, along with muscle relaxants such as dantrolene to combat muscle rigidity. Chloroform or heavy doses of chloral, bromide, urethane or amyl nitrate can also be used to restrain the convulsions. Because diazepam, as the anticonvulsant of choice, is not effective in all cases, a combination with midazolam, fentanyl, or pancuronium is recommended for controlling the convulsions. Strychnine poisoning demands an aggressive management with early intubation, control of muscle tremors, and prevention of rhabdomyolysis and renal failure. If the patient survives the first 24 hours after poisoning then recovery is probable. Also, George Harley (1829–1896) showed in 1850 that Curare (wourali) was effective for the treatment of tetanus and strychnine poisoning.
See also
- Notable strychnine poisonings
- Fictional strychnine poisonings
- Avicide
- Denatonium
- "Poisoning Pigeons in the Park"
- Strychnine poisoning
- The Mysterious Affair at Styles
- Wieland-Gumlich aldehyde
- William Palmer
References
- ↑ Everett, A. J.; Openshaw, H. T.; Smith, G. F. (1957). "221. The constitution of aspidospermine. Part III. Reactivity at the nitrogen atoms, and biogenetic considerations". Journal of the Chemical Society (Resumed): 1120. doi:10.1039/JR9570001120.
- ↑ INCHEM: Chemical Safety Information from Intergovernmental Organizations:Strychnine. http://www.inchem.org/documents/pims/chemical/pim507.htm
- ↑ 3.0 3.1 3.2 Sharma, R.K., Consice textbook of forensic medicine & toxicology, Elsevier, 2008
- ↑ Pelletier and Caventou (1818) "Note sur un nouvel alkalai" (Note on a new alkali), Annales de Chimie et de Physique, vol. 8, pages 323-324. See also: Pelletier and Caventou (1819) "Mémoire sur un nouvel alcali vegetal (la strychnine) trouvé dans la feve de Saint-Ignace, la noix vomique, etc." (Memoir on a new vegetable alkali (strychnine) found in the St. Ignatius bean, the nux vomica, etc), Annales de Chimie et de Physique, vol. 10, pages 142 - 176.
- ↑ 5.0 5.1 Gupta, R.C., Handbook of Toxicology of Chemical Warfare Agents, Elsevier Inc, 2009, Chapter 14
- ↑ 6.0 6.1 Bonjoch, Josep; Solé, Daniel (1 September 2000). "Synthesis of Strychnine". Chemical Reviews 100 (9): 3455–3482. doi:10.1021/cr9902547.
- ↑ Dewick, Paul M. (2009). Medicinal natural products : a biosynthetic approach (3rd ed. ed.). Chichester: A John Wiley & Sons. pp. 377–378. ISBN 978-0-470-74167-2.
- ↑ Treimer, Johannes F.; Zenk, Meinhart H. (1 November 1979). "Purification and Properties of Strictosidine Synthase, the Key Enzyme in Indole Alkaloid Formation". European Journal of Biochemistry 101 (1): 225–233. doi:10.1111/j.1432-1033.1979.tb04235.x. PMID 510306.
- ↑ 9.0 9.1 Heimberger, Stanley I.; Scott, A. Ian (1 January 1973). "Biosynthesis of strychnine". Journal of the Chemical Socie ty, Chemical Communications (6): 217. doi:10.1039/C39730000217.
- ↑ Wieland, Heinrich; Gumlich, Walter (1 January 1932). "Über einige neue Reaktionen der Strychnos - Alkaloide. XI". Justus Liebig's Annalen der Chemie 494 (1): 191–200. doi:10.1002/jlac.19324940116.
- ↑ K. C. Nicolaou, Dionisios Vourloumis, Nicolas Winssinger & Phil S. Baran, 2000, The Art and Science of Total Synthesis at the Dawn of the Twenty-First Century, Angewandte Chemie Int. Ed. 39(1):44-122
- ↑ R. Robinson, 1952, Molecular structure of Strychnine, Brucine and Vomicine, Prog. Org. Chem. 1:2
- ↑ K.C. Nicolaou & E.J. Sorensen, 1996, Classics in Total Synthesis: Targets, Strategies, Methods. Wiley. ISBN 978-3-527-29231-8.
- ↑ Josep Bonjoch & Daniel Sole, 2000, Synthesis of Strychnine, Chem. Rev. 100:3455-3482. DOI 10.1021/cr9902547
- ↑ R. B. Woodward, Michael P. Cava, W. D. Ollis, A. Hunger, H. U. Daeniker, & K. Schenker, 1954, J. Am. Chem. Soc. 76(18):4749–4751, DOI 10.1021/ja01647a088
- ↑ R. B. Woodward, M. P. Cava, W. D. Ollis, A. Hunger, H. U. Daeniker, & K. Schenker, 1963, The total synthesis of strychnine, Tetrahedron 19(2):247-288
- ↑ Meyerhof, W.; Batram, C.; Kuhn, C.; Brockhoff, A.; Chudoba, E.; Bufe, B.; Appendino, G.; Behrens, M. (2009). "The Molecular Receptive Ranges of Human TAS2R Bitter Taste Receptors". Chemical Senses 35 (2): 157–170. doi:10.1093/chemse/bjp092. PMID 20022913.
- ↑ Born, S.; Levit, A.; Niv, M. Y.; Meyerhof, W.; Behrens, M. (2013). "The Human Bitter Taste Receptor TAS2R10 is Tailored to Accommodate Numerous Diverse Ligands". Journal of Neuroscience 33 (1): 201–13. doi:10.1523/JNEUROSCI.3248-12.2013. PMID 23283334.
- ↑ Meyerhof, W.; Born, S.; Brockhoff, A.; Behrens, M. (2011). "Molecular biology of mammalian bitter taste receptors. A review". Flavour and Fragrance Journal 26 (4): 260. doi:10.1002/ffj.2041.
- ↑ Waring, R.H., Steventon, G.B, Mitchell, S.C, Molecules of death, Imperial College Press, 2007
- ↑ Brams et al. (2011). "A structural and mutagenic blueprint for molecular recognition of strychnine and d-tubocurarine by different cys-loop receptors". PLoS Biol 9 (3). doi:10.1371/journal.pbio.1001034.
- ↑ 22.0 22.1 22.2 22.3 Tucker, RK; Haegele, MA (1971). "Comparative acute oral toxicity of pesticides to six species of birds". Toxicology and applied pharmacology 20 (1): 57–65. doi:10.1016/0041-008X(71)90088-3. PMID 5110827.
- ↑ 23.0 23.1 23.2 RTECS (1935)
- ↑ 24.0 24.1 Moraillon, R.; Pinoult, L. (1978). "Diagnostic et traitement d'intoxications courantes des carnivores". Rec Med Vet (in French) 174 (1–2): 36–43.
- ↑ 25.0 25.1 Longo, V.G.; Silvestrini, B.; Bovet, D. (1959). "An investigation of convulsant properties of the 5,7-diphenyl-1,3-diazadamantan- 6-ol (IS 1757)". J. Pharmacol. Exp. Ther. 126 (1): 41–9. PMID 13642285.
- ↑ Setnikar, I; Murmann, W; Magistretti, MJ; Da Re, P (1960). "Amino-methylchromones, brain stem stimulants and pentobarbital antagonists". The Journal of Pharmacology and Experimental Therapeutics 128: 176–81. PMID 14445192.
- ↑ Haas, H (1960). "On 3-piperidino-1-phenyl-1-bicycloheptenyl-1-propanol (Akineton). 2". Archives internationales de pharmacodynamie et de therapie 128: 204–38. PMID 13710192.
- ↑ Prasad, CR; Patnaik, GK; Gupta, RC; Anand, N; Dhawan, BN (1981). "Central nervous system stimulant activity of n-(delta 3-chromene-3-carbonyl)-4 iminopyridine (compound 69/224)". Indian journal of experimental biology 19 (11): 1075–6. PMID 7338366.
- ↑ Zapata-Ortiz, V; CASTRO DE LA MATA R; Barantes-Campos, R (1961). "The anticonvulsive action of cocaine". Arzneimittel-Forschung 11: 657–62. PMID 13787891.
- ↑ Sandberg, F; Kristianson, K (1970). "A comparative study of the convulsant effects of strychnos alkaloids". Acta pharmaceutica Suecica 7 (4): 329–36. PMID 5480076.
- ↑ Spector, W.S. (1956). Handbook of Toxicology, Vol. 1, p. 286. W.B. Saunders Company, Philadelphia.
- ↑ Ward, Justus C.; Crabtree, D. Glen (2006). "Strychnine X. Comparative accuracies of stomach tube and intraperitoneal injection methods of bioassay". Journal of the American Pharmaceutical Association 31 (4): 113–115. doi:10.1002/jps.3030310406.
- ↑ Zenz, C., Dickerson, O. B., Horvath, E. P. (1994). Occupational Medicine, 3rd edition, p. 640. St Louis.
- ↑ Palatnick, W; Meatherall, R; Sitar, D; Tenenbein, M (1997). "Toxicokinetics of acute strychnine poisoning". Journal of toxicology. Clinical toxicology 35 (6): 617–20. doi:10.3109/15563659709001242. PMID 9365429.
- ↑ Lewis, R.J. (1996). Sax’s Dangerous Properties of Industrial Materials. 9th edition, Vols. 1–3, p. 3025. Van Nostrand Reinhold, New York.
- ↑ Goodman, L. S., Gilman, A. G., Gilman, A. The pharmalogical basis of therapeutics, 1985, New York Macmillan Publishing & Co., Inc.
- ↑ 37.0 37.1 Bennett, S. M. http://www.the-piedpiper.co.uk/th15\%28f\%29.htm
- ↑ 38.0 38.1 Gossel, T. A., Bricker J. D. (1994). Principles of Clinical Toxicology, 3rd edition, p. 351. Raven Press, New York.
- ↑ Migliaccio, E; Celentano, R; Viglietti, A; Viglietti, G (1990). "Strychnine poisoning. A clinical case". Minerva anestesiologica 56 (1–2): 41–2. PMID 2215981.
- ↑ Ellenhorn, M.J., Schonwald, S., Ordog, G. (1997). J. Wasserberger. Ellenhorn’s Medical Toxicology: Diagnosis and Treatment of Human Poisoning, 2nd edition, p. 1660. Williams and Wilkins, Baltimore.
- ↑ CDC - NIOSH Pocket Guide to Chemical Hazards
| ||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||