Stroke
| Stroke | |
|---|---|
 CT scan of the brain showing a right-hemispheric ischemic stroke. | |
| Classification and external resources | |
| ICD-10 | I61-I64ner |
| ICD-9 | 434.91 |
| OMIM | 601367 |
| DiseasesDB | 2247 |
| MedlinePlus | 000726 |
| eMedicine | neuro/9 emerg/558 emerg/557 pmr/187 |
| Patient UK | Stroke |
| MeSH | D020521 |
Stroke, also known as cerebrovascular accident (CVA), cerebrovascular insult (CVI), or brain attack, is when poor blood flow to the brain results in cell death. There are two main types of stroke: ischemic due to lack of blood flow and hemorrhagic due to bleeding. They result in part of the brain not functioning properly.[1] Signs and symptoms of a stroke may include an inability to move or feel on one side of the body, problems understanding or speaking, feeling like the world is spinning, or loss of one vision to one side among others.[2][3] Signs and symptoms often appear soon after the stroke has occurred. If symptoms last less than one or two hours it is known as a transient ischemic attack (TIA).[3] Hemorrhagic strokes may also be associated with a severe headache.[3] The symptoms of a stroke can be permanent.[1] Long term complications may include pneumonia or loss of bladder control.[3]
The main risk factor for stroke is high blood pressure.[4] Other risk factors include tobacco smoking, obesity, high blood cholesterol, diabetes mellitus, previous TIA, and atrial fibrillation among others.[2][4] An ischemic stroke is typically caused by blockage of a blood vessel.[5] A hemorrhagic stroke is caused by bleeding either directly into the brain or into the space surrounding the brain.[5][6] Bleeding may occur due to a brain aneurysm.[5] Diagnosis is typically with medical imaging such as a CT scan or MRI scan along with a physical exam. Other tests such as an electrocardiogram (ECG) and blood tests are done to determine risk factors and rule out other possible causes. Low blood sugar may cause similar symptoms.[7]
Prevention includes decreasing risk factors as well as possibly aspirin, statins, surgery to open up the arteries to the brain in those with problematic narrowing, and warfarin in those with atrial fibrillation.[2] A stroke often requires emergency care.[1] An ischemic stroke, if detected within three to four and half hours, may be treatable with a medication that can break down the clot. Aspirin should be used. Some hemorrhagic strokes benefit from surgery. Treatment to try recover lost function is called stroke rehabilitation and ideally takes place in a stroke unit; however, these are not available in much of the world.[2]
In 2010 approximately 17 million people had a stroke and 33 million people had previously had a stroke and were still alive. Between 1990 and 2010 the number of strokes which occurred each year decreased by approximately 10% in the developed world and increased by 10% in the developing world.[8] In 2013, stroke was the second most frequent cause of death after coronary artery disease, accounting for 6.4 million deaths (12% of the total).[9] About 3.3 million deaths resulted from ischemic stroke while 3.2 million deaths resulted from hemorrhagic stroke.[9] About half of people who have had a stroke live less than one year.[2] Overall, two thirds of strokes occurred in those over 65 years old.[8]
Classification
Strokes can be classified into two major categories: ischemic and hemorrhagic.[10] Ischemic strokes are caused by interruption of the blood supply to the brain, while hemorrhagic strokes result from the rupture of a blood vessel or an abnormal vascular structure. About 87% of strokes are ischemic, the rest being hemorrhagic. Bleeding can develop inside areas of ischemia, a condition known as "hemorrhagic transformation." It is unknown how many hemorrhagic strokes actually start as ischemic strokes.[2]
Definition
In the 1970s the World Health Organization defined stroke as a "neurological deficit of cerebrovascular cause that persists beyond 24 hours or is interrupted by death within 24 hours",[11] although the word "stroke" is centuries old. This definition was supposed to reflect the reversibility of tissue damage and was devised for the purpose, with the time frame of 24 hours being chosen arbitrarily. The 24-hour limit divides stroke from transient ischemic attack, which is a related syndrome of stroke symptoms that resolve completely within 24 hours.[2] With the availability of treatments which can reduce stroke severity when given early, many now prefer alternative terminology, such as brain attack and acute ischemic cerebrovascular syndrome (modeled after heart attack and acute coronary syndrome, respectively), to reflect the urgency of stroke symptoms and the need to act swiftly.[12]
Ischemic
In an ischemic stroke, blood supply to part of the brain is decreased, leading to dysfunction of the brain tissue in that area. There are four reasons why this might happen:
- Thrombosis (obstruction of a blood vessel by a blood clot forming locally)
- Embolism (obstruction due to an embolus from elsewhere in the body, see below),[2]
- Systemic hypoperfusion (general decrease in blood supply, e.g., in shock)[13]
- Venous thrombosis.[14]
Stroke without an obvious explanation is termed "cryptogenic" (of unknown origin); this constitutes 30-40% of all ischemic strokes.[2][15]
There are various classification systems for acute ischemic stroke. The Oxford Community Stroke Project classification (OCSP, also known as the Bamford or Oxford classification) relies primarily on the initial symptoms; based on the extent of the symptoms, the stroke episode is classified as total anterior circulation infarct (TACI), partial anterior circulation infarct (PACI), lacunar infarct (LACI) or posterior circulation infarct (POCI). These four entities predict the extent of the stroke, the area of the brain that is affected, the underlying cause, and the prognosis.[16][17] The TOAST (Trial of Org 10172 in Acute Stroke Treatment) classification is based on clinical symptoms as well as results of further investigations; on this basis, a stroke is classified as being due to (1) thrombosis or embolism due to atherosclerosis of a large artery, (2) an embolism originating in the heart, (3) complete blockage of a small blood vessel, (4) other determined cause, (5) undetermined cause (two possible causes, no cause identified, or incomplete investigation).[18] Users of stimulant drugs such as cocaine and methamphetamine are at a high risk for ischemic strokes.[19]
Hemorrhagic

An intracranial hemorrhage is the accumulation of blood anywhere within the cranial vault. The main types of intracranial hemorrhage are epidural hematoma (bleeding between the dura mater and the skull), subdural hematoma (in the subdural space) and subarachnoid hemorrhage (between the arachnoid mater and pia mater).
A cerebral hemorrhage is bleeding within the brain tissue. A cerebral hemorrhage can be due to either intraparenchymal hemorrhage or intraventricular hemorrhage (blood in the ventricular system). Most of the hemorrhagic stroke syndromes have specific symptoms particularly headaches, or have evidence of a previous head injury).
Signs and symptoms
Stroke symptoms typically start suddenly, over seconds to minutes, and in most cases do not progress further. The symptoms depend on the area of the brain affected. The more extensive the area of brain affected, the more functions that are likely to be lost. Some forms of stroke can cause additional symptoms. For example, in intracranial hemorrhage, the affected area may compress other structures. Most forms of stroke are not associated with headache, apart from subarachnoid hemorrhage and cerebral venous thrombosis and occasionally intracerebral hemorrhage.
Early recognition
Various systems have been proposed to increase recognition of stroke. Different findings are able to predict the presence or absence of stroke to different degrees. Sudden-onset face weakness, arm drift (i.e., if a person, when asked to raise both arms, involuntarily lets one arm drift downward) and abnormal speech are the findings most likely to lead to the correct identification of a case of stroke increasing the likelihood by 5.5 when at least one of these is present). Similarly, when all three of these are absent, the likelihood of stroke is significantly decreased (– likelihood ratio of 0.39).[20] While these findings are not perfect for diagnosing stroke, the fact that they can be evaluated relatively rapidly and easily make them very valuable in the acute setting.
Proposed systems include FAST (face, arm, speech, and time),[21] as advocated by the Department of Health (United Kingdom) and the Stroke Association, the American Stroke Association, the National Stroke Association (US), the Los Angeles Prehospital Stroke Screen (LAPSS)[22] and the Cincinnati Prehospital Stroke Scale (CPSS).[23] Use of these scales is recommended by professional guidelines.[24]
For people referred to the emergency room, early recognition of stroke is deemed important as this can expedite diagnostic tests and treatments. A scoring system called ROSIER (recognition of stroke in the emergency room) is recommended for this purpose; it is based on features from the medical history and physical examination.[24][25]
Subtypes
If the area of the brain affected contains one of the three prominent central nervous system pathways—the spinothalamic tract, corticospinal tract, and dorsal column (medial lemniscus), symptoms may include:
- hemiplegia and muscle weakness of the face
- numbness
- reduction in sensory or vibratory sensation
- initial flaccidity (reduced muscle tone), replaced by spasticity (increased muscle tone), excessive reflexes, and obligatory synergies.[26]
In most cases, the symptoms affect only one side of the body (unilateral). Depending on the part of the brain affected, the defect in the brain is usually on the opposite side of the body. However, since these pathways also travel in the spinal cord and any lesion there can also produce these symptoms, the presence of any one of these symptoms does not necessarily indicate a stroke.
In addition to the above CNS pathways, the brainstem gives rise to most of the twelve cranial nerves. A stroke affecting the brainstem and brain therefore can produce symptoms relating to deficits in these cranial nerves:
- altered smell, taste, hearing, or vision (total or partial)
- drooping of eyelid (ptosis) and weakness of ocular muscles
- decreased reflexes: gag, swallow, pupil reactivity to light
- decreased sensation and muscle weakness of the face
- balance problems and nystagmus
- altered breathing and heart rate
- weakness in sternocleidomastoid muscle with inability to turn head to one side
- weakness in tongue (inability to stick out the tongue and/or move it from side to side)
If the cerebral cortex is involved, the CNS pathways can again be affected, but also can produce the following symptoms:
- aphasia (difficulty with verbal expression, auditory comprehension, reading and/or writing; Broca's or Wernicke's area typically involved)
- dysarthria (motor speech disorder resulting from neurological injury)
- apraxia (altered voluntary movements)
- visual field defect
- memory deficits (involvement of temporal lobe)
- hemineglect (involvement of parietal lobe)
- disorganized thinking, confusion, hypersexual gestures (with involvement of frontal lobe)
- lack of insight of his or her, usually stroke-related, disability
If the cerebellum is involved, the patient may have the following:
- altered walking gait
- altered movement coordination
- vertigo and or disequilibrium
Associated symptoms
Loss of consciousness, headache, and vomiting usually occurs more often in hemorrhagic stroke than in thrombosis because of the increased intracranial pressure from the leaking blood compressing the brain.
If symptoms are maximal at onset, the cause is more likely to be a subarachnoid hemorrhage or an embolic stroke.
Causes
Thrombotic stroke

In thrombotic stroke a thrombus[27] (blood clot) usually forms around atherosclerotic plaques. Since blockage of the artery is gradual, onset of symptomatic thrombotic strokes is slower than that of a hemorrhagic stroke. A thrombus itself (even if it does not completely block the blood vessel) can lead to an embolic stroke (see below) if the thrombus breaks off and travels in the bloodstream, at which point it is called an "embolus." Two types of thrombosis can cause stroke:
- Large vessel disease involves the common and internal carotid arteries, the vertebral artery, and the Circle of Willis.[28] Diseases that may form thrombi in the large vessels include (in descending incidence): atherosclerosis, vasoconstriction (tightening of the artery), aortic, carotid or vertebral artery dissection, various inflammatory diseases of the blood vessel wall (Takayasu arteritis, giant cell arteritis, vasculitis), noninflammatory vasculopathy, Moyamoya disease and fibromuscular dysplasia.
- Small vessel disease involves the smaller arteries inside the brain: branches of the circle of Willis, middle cerebral artery, stem, and arteries arising from the distal vertebral and basilar artery.[29] Diseases that may form thrombi in the small vessels include (in descending incidence): lipohyalinosis (build-up of fatty hyaline matter in the blood vessel as a result of high blood pressure and aging) and fibrinoid degeneration (a stroke involving these vessels are known as a lacunar stroke) and microatheroma (small atherosclerotic plaques).[30]
Sickle-cell anemia, which can cause blood cells to clump up and block blood vessels, can also lead to stroke. A stroke is the second leading cause of death in people under 20 with sickle-cell anemia.[31] Air pollution may also increase stroke risk.[32]
Embolic stroke
An embolic stroke refers to an arterial embolism (a blockage of an artery) by an embolus, a traveling particle or debris in the arterial bloodstream originating from elsewhere. An embolus is most frequently a thrombus, but it can also be a number of other substances including fat (e.g., from bone marrow in a broken bone), air, cancer cells or clumps of bacteria (usually from infectious endocarditis).[33]
Because an embolus arises from elsewhere, local therapy solves the problem only temporarily. Thus, the source of the embolus must be identified. Because the embolic blockage is sudden in onset, symptoms usually are maximal at start. Also, symptoms may be transient as the embolus is partially resorbed and moves to a different location or dissipates altogether.
Emboli most commonly arise from the heart (especially in atrial fibrillation) but may originate from elsewhere in the arterial tree. In paradoxical embolism, a deep vein thrombosis embolizes through an atrial or ventricular septal defect in the heart into the brain.[33]
Causes of stroke related to the heart can be distinguished between high and low-risk:[34]
- High risk: atrial fibrillation and paroxysmal atrial fibrillation, rheumatic disease of the mitral or aortic valve disease, artificial heart valves, known cardiac thrombus of the atrium or ventricle, sick sinus syndrome, sustained atrial flutter, recent myocardial infarction, chronic myocardial infarction together with ejection fraction <28 percent, symptomatic congestive heart failure with ejection fraction <30 percent, dilated cardiomyopathy, Libman-Sacks endocarditis, Marantic endocarditis, infective endocarditis, papillary fibroelastoma, left atrial myxoma and coronary artery bypass graft (CABG) surgery.
- Low risk/potential: calcification of the annulus (ring) of the mitral valve, patent foramen ovale (PFO), atrial septal aneurysm, atrial septal aneurysm with patent foramen ovale, left ventricular aneurysm without thrombus, isolated left atrial "smoke" on echocardiography (no mitral stenosis or atrial fibrillation), complex atheroma in the ascending aorta or proximal arch.
Cerebral hypoperfusion
Cerebral hypoperfusion is the reduction of blood flow to all parts of the body. It is most commonly due to heart failure from cardiac arrest or arrhythmias, or from reduced cardiac output as a result of myocardial infarction, pulmonary embolism, pericardial effusion, or bleeding. Hypoxemia (low blood oxygen content) may precipitate the hypoperfusion. Because the reduction in blood flow is global, all parts of the brain may be affected, especially vulnerable "watershed" areas - border zone regions supplied by the major cerebral arteries. A watershed stroke refers to the condition when blood supply to these areas is compromised. Blood flow to these areas does not necessarily stop, but instead it may lessen to the point where brain damage can occur.
Venous thrombosis
Cerebral venous sinus thrombosis leads to stroke due to locally increased venous pressure, which exceeds the pressure generated by the arteries. Infarcts are more likely to undergo hemorrhagic transformation (leaking of blood into the damaged area) than other types of ischemic stroke.[14]
Intracerebral hemorrhage
It generally occurs in small arteries or arterioles and is commonly due to hypertension,[35] intracranial vascular malformations (including cavernous angiomas or arteriovenous malformations), cerebral amyloid angiopathy, or infarcts into which secondary hemorrhage has occurred.[2] Other potential causes are trauma, bleeding disorders, amyloid angiopathy, illicit drug use (e.g., amphetamines or cocaine). The hematoma enlarges until pressure from surrounding tissue limits its growth, or until it decompresses by emptying into the ventricular system, CSF or the pial surface. A third of intracerebral bleed is into the brain's ventricles. ICH has a mortality rate of 44 percent after 30 days, higher than ischemic stroke or subarachnoid hemorrhage (which technically may also be classified as a type of stroke[2]).
Silent stroke
A silent stroke is a stroke that does not have any outward symptoms, and the patients are typically unaware they have had a stroke. Despite not causing identifiable symptoms, a silent stroke still damages the brain, and places the patient at increased risk for both transient ischemic attack and major stroke in the future. Conversely, those who have had a major stroke are also at risk of having silent strokes.[36] In a broad study in 1998, more than 11 million people were estimated to have experienced a stroke in the United States. Approximately 770,000 of these strokes were symptomatic and 11 million were first-ever silent MRI infarcts or hemorrhages. Silent strokes typically cause lesions which are detected via the use of neuroimaging such as MRI. Silent strokes are estimated to occur at five times the rate of symptomatic strokes.[37][38] The risk of silent stroke increases with age, but may also affect younger adults and children, especially those with acute anemia.[37][39]
Pathophysiology
Ischemic

Ischemic stroke occurs because of a loss of blood supply to part of the brain, initiating the ischemic cascade.[40] Brain tissue ceases to function if deprived of oxygen for more than 60 to 90 seconds, and after approximately three hours will suffer irreversible injury possibly leading to death of the tissue, i.e., infarction. (This is why fibrinolytics such as alteplase are given only until three hours since the onset of the stroke.) Atherosclerosis may disrupt the blood supply by narrowing the lumen of blood vessels leading to a reduction of blood flow, by causing the formation of blood clots within the vessel, or by releasing showers of small emboli through the disintegration of atherosclerotic plaques.[41] Embolic infarction occurs when emboli formed elsewhere in the circulatory system, typically in the heart as a consequence of atrial fibrillation, or in the carotid arteries, break off, enter the cerebral circulation, then lodge in and block brain blood vessels. Since blood vessels in the brain are now blocked, the brain becomes low in energy, and thus it resorts into using anaerobic metabolism within the region of brain tissue affected by ischemia. Anaerobic metabolism produces less adenosine triphosphate (ATP) but releases a by-product called lactic acid. Lactic acid is an irritant which could potentially destroy cells since it is an acid and disrupts the normal acid-base balance in the brain. The ischemia area is referred to as the "ischemic penumbra".[42]
As oxygen or glucose becomes depleted in ischemic brain tissue, the production of high energy phosphate compounds such as adenosine triphosphate (ATP) fails, leading to failure of energy-dependent processes (such as ion pumping) necessary for tissue cell survival. This sets off a series of interrelated events that result in cellular injury and death. A major cause of neuronal injury is release of the excitatory neurotransmitter glutamate. The concentration of glutamate outside the cells of the nervous system is normally kept low by so-called uptake carriers, which are powered by the concentration gradients of ions (mainly Na+) across the cell membrane. However, stroke cuts off the supply of oxygen and glucose which powers the ion pumps maintaining these gradients. As a result the transmembrane ion gradients run down, and glutamate transporters reverse their direction, releasing glutamate into the extracellular space. Glutamate acts on receptors in nerve cells (especially NMDA receptors), producing an influx of calcium which activates enzymes that digest the cells' proteins, lipids and nuclear material. Calcium influx can also lead to the failure of mitochondria, which can lead further toward energy depletion and may trigger cell death due to programmed cell death.
Ischemia also induces production of oxygen free radicals and other reactive oxygen species. These react with and damage a number of cellular and extracellular elements. Damage to the blood vessel lining or endothelium is particularly important. In fact, many antioxidant neuroprotectants such as uric acid and NXY-059 work at the level of the endothelium and not in the brain per se. Free radicals also directly initiate elements of the programmed cell death cascade by means of redox signaling.
These processes are the same for any type of ischemic tissue and are referred to collectively as the ischemic cascade. However, brain tissue is especially vulnerable to ischemia since it has little respiratory reserve and is completely dependent on aerobic metabolism, unlike most other organs.
In addition to damaging effects on brain cells, ischemia and infarction can result in loss of structural integrity of brain tissue and blood vessels, partly through the release of matrix metalloproteases, which are zinc- and calcium-dependent enzymes that break down collagen, hyaluronic acid, and other elements of connective tissue. Other proteases also contribute to this process. The loss of vascular structural integrity results in a breakdown of the protective blood brain barrier that contributes to cerebral edema, which can cause secondary progression of the brain injury.
Hemorrhagic
Bleeding within the skull cavity can occur from various causes. Subdural and epidural bleeding mostly are the result of trauma.[43] Hemorrhagic strokes arise from bleeding within the brain parenchyma or intraventricular spaces, and are classified based on their underlying pathology. Some examples of hemorrhagic stroke are hypertensive hemorrhage, ruptured aneurysm, ruptured AV fistula, transformation of prior ischemic infarction, and drug induced bleeding.[44] They result in tissue injury by causing compression of tissue from an expanding hematoma or hematomas. This can distort and injure tissue. In addition, the pressure may lead to a loss of blood supply to affected tissue with resulting infarction, and the blood released by brain hemorrhage appears to have direct toxic effects on brain tissue and vasculature.[31][45] Inflammation contributes to the secondary brain injury after hemorrhage.[45]
Diagnosis

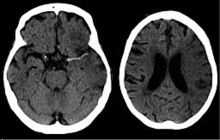
Stroke is diagnosed through several techniques: a neurological examination (such as the NIHSS), CT scans (most often without contrast enhancements) or MRI scans, Doppler ultrasound, and arteriography. The diagnosis of stroke itself is clinical, with assistance from the imaging techniques. Imaging techniques also assist in determining the subtypes and cause of stroke. There is yet no commonly used blood test for the stroke diagnosis itself, though blood tests may be of help in finding out the likely cause of stroke.[46]
Physical examination
A physical examination, including taking a medical history of the symptoms and a neurological status, helps giving an evaluation of the location and severity of a stroke. It can give a standard score on e.g., the NIH stroke scale.
Imaging
For diagnosing ischemic stroke in the emergency setting:[47]
- CT scans (without contrast enhancements)
- sensitivity= 16%
- specificity= 96%
- MRI scan
- sensitivity= 83%
- specificity= 98%
For diagnosing hemorrhagic stroke in the emergency setting:
- CT scans (without contrast enhancements)
- sensitivity= 89%
- specificity= 100%
- MRI scan
- sensitivity= 81%
- specificity= 100%
For detecting chronic hemorrhages, MRI scan is more sensitive.[48]
For the assessment of stable stroke, nuclear medicine scans SPECT and PET/CT may be helpful. SPECT documents cerebral blood flow and PET with FDG isotope the metabolic activity of the neurons.
Underlying cause

When a stroke has been diagnosed, various other studies may be performed to determine the underlying cause. With the current treatment and diagnosis options available, it is of particular importance to determine whether there is a peripheral source of emboli. Test selection may vary, since the cause of stroke varies with age, comorbidity and the clinical presentation. The following are commonly used techniques:
- an ultrasound/doppler study of the carotid arteries (to detect carotid stenosis) or dissection of the precerebral arteries;
- an electrocardiogram (ECG) and echocardiogram (to identify arrhythmias and resultant clots in the heart which may spread to the brain vessels through the bloodstream);
- a Holter monitor study to identify intermittent abnormal heart rhythms;
- an angiogram of the cerebral vasculature (if a bleed is thought to have originated from an aneurysm or arteriovenous malformation);
- blood tests to determine if blood cholesterol is high, if there is an abnormal tendency to bleed, and if some rarer processes such as homocysteinuria might be involved.
Prevention
Given the disease burden of strokes, prevention is an important public health concern.[49] Primary prevention is less effective than secondary prevention (as judged by the number needed to treat to prevent one stroke per year).[49] Recent guidelines detail the evidence for primary prevention in stroke.[50] In those who are otherwise healthy, aspirin does not appear beneficial and thus is not recommended.[51] In people who have had a myocardial infarction or those with a high cardiovascular risk, it provides some protection against a first stroke.[52][53] In those who have previously had a stroke, treatment with medications such as aspirin, clopidogrel and dipyridamole may be beneficial.[52] The U.S. Preventive Services Task Force (USPSTF) recommends against screening for carotid artery stenosis in those without symptoms.[54]
Risk factors
The most important modifiable risk factors for stroke are high blood pressure and atrial fibrillation (although magnitude of this effect is small: the evidence from the Medical Research Council trials is that 833 patients have to be treated for 1 year to prevent one stroke[55][56]). Other modifiable risk factors include high blood cholesterol levels, diabetes mellitus, cigarette smoking[57][58] (active and passive), heavy alcohol consumption[59] and drug use,[60] lack of physical activity, obesity, processed red meat consumption[61] and unhealthy diet.[62] Alcohol use could predispose to ischemic stroke, and intracerebral and subarachnoid hemorrhage via multiple mechanisms (for example via hypertension, atrial fibrillation, rebound thrombocytosis and platelet aggregation and clotting disturbances).[63] Drugs, most commonly amphetamines and cocaine, can induce stroke through damage to the blood vessels in the brain and/or acute hypertension.[64][65]
No high-quality studies have shown the effectiveness of interventions aimed at weight reduction, promotion of regular exercise, reducing alcohol consumption or smoking cessation.[66] Nonetheless, given the large body of circumstantial evidence, best medical management for stroke includes advice on diet, exercise, smoking and alcohol use.[67] Medication or drug therapy is the most common method of stroke prevention; carotid endarterectomy can be a useful surgical method of preventing stroke.
Blood pressure
Hypertension (high blood pressure) accounts for 35-50% of stroke risk.[68] Blood pressure reduction of 10 mmHg systolic or 5 mmHg diastolic reduces the risk of stroke by ~40%.[69] Lowering blood pressure has been conclusively shown to prevent both ischemic and hemorrhagic strokes.[70][71] It is equally important in secondary prevention.[72] Even patients older than 80 years and those with isolated systolic hypertension benefit from antihypertensive therapy.[73][74][75] The available evidence does not show large differences in stroke prevention between antihypertensive drugs —therefore, other factors such as protection against other forms of cardiovascular disease and cost should be considered.[76][77] The routine use of beta-blockers following a stroke or TIA has not been shown to result in benefits.[78]
Blood lipids
High cholesterol levels have been inconsistently associated with (ischemic) stroke.[71][79] Statins have been shown to reduce the risk of stroke by about 15%.[80] Since earlier meta-analyses of other lipid-lowering drugs did not show a decreased risk,[81] statins might exert their effect through mechanisms other than their lipid-lowering effects.[80]
Diabetes mellitus
Diabetes mellitus increases the risk of stroke by 2 to 3 times. While intensive blood sugar control has been shown to reduce small blood vessel complications such as kidney damage and damage to the retina of the eye it has not been shown to reduce large blood vessel complications such as stroke.[82][83]
Anticoagulation drugs
Oral anticoagulants such as warfarin have been the mainstay of stroke prevention for over 50 years. However, several studies have shown that aspirin and antiplatelet drugs are highly effective in secondary prevention after a stroke or transient ischemic attack.[52] Low doses of aspirin (for example 75–150 mg) are as effective as high doses but have fewer side effects; the lowest effective dose remains unknown.[84] Thienopyridines (clopidogrel, ticlopidine) "might be slightly more effective" than aspirin and have a decreased risk of gastrointestinal bleeding, but are more expensive.[85] Their exact role remains controversial. Ticlopidine is associated with higher rates of skin rash, diarrhea, low blood neutrophil count and thrombotic thrombocytopenic purpura.[85] Dipyridamole can be added to aspirin therapy to provide a small additional benefit, even though headache is a common side effect.[86] Low-dose aspirin is also effective for stroke prevention after having a myocardial infarction.[53]
Those with atrial fibrillation have a 5% a year risk of stroke, and this risk is higher in those with valvular atrial fibrillation.[87] Depending on the stroke risk, anticoagulation with medications such as warfarin or aspirin is useful for prevention.[88] Except in people with atrial fibrillation, oral anticoagulants are not advised for stroke prevention —any benefit is offset by bleeding risk.[89]
In primary prevention however, antiplatelet drugs did not reduce the risk of ischemic stroke but increased the risk of major bleeding.[90][91] Further studies are needed to investigate a possible protective effect of aspirin against ischemic stroke in women.[92][93]
Surgery
Carotid endarterectomy or carotid angioplasty can be used to remove atherosclerotic narrowing (stenosis) of the carotid artery. There is evidence supporting this procedure in selected cases.[67] Endarterectomy for a significant stenosis has been shown to be useful in the prevention of further strokes in those who have already had one.[94] Carotid artery stenting has not been shown to be equally useful.[95][96] Patients are selected for surgery based on age, gender, degree of stenosis, time since symptoms and patients' preferences.[67] Surgery is most efficient when not delayed too long —the risk of recurrent stroke in a patient who has a 50% or greater stenosis is up to 20% after 5 years, but endarterectomy reduces this risk to around 5%. The number of procedures needed to cure one patient was 5 for early surgery (within two weeks after the initial stroke), but 125 if delayed longer than 12 weeks.[97][98]
Screening for carotid artery narrowing has not been shown to be a useful screening test in the general population.[99] Studies of surgical intervention for carotid artery stenosis without symptoms have shown only a small decrease in the risk of stroke.[100][101] To be beneficial, the complication rate of the surgery should be kept below 4%. Even then, for 100 surgeries, 5 patients will benefit by avoiding stroke, 3 will develop stroke despite surgery, 3 will develop stroke or die due to the surgery itself, and 89 will remain stroke-free but would also have done so without intervention.[67]
Diet
Nutrition, specifically the Mediterranean-style diet, has the potential for decreasing the risk of having a stroke by more than half.[102] It does not appear that lowering levels of homocysteine with folic acid affects the risk of stroke.[103][104]
Women
A number of specific recommendations have been made for women including taking aspirin after the 11th week of pregnancy if there is a history of previous chronic high blood pressure and taking blood pressure medications during pregnancy if the blood pressure is greater than 150 mmHg systolic or greater than 100 mmHg diastolic. In those who have previously had preeclampsia other risk factors should be treated more aggressively.[105]
Previous stroke or TIA
Keeping blood pressure below 140/90 mmHg is recommended.[106] Anticoagulation can prevent recurrent ischemic strokes. Among people with nonvalvular atrial fibrillation, anticoagulation can reduce stroke by 60% while antiplatelet agents can reduce stroke by 20%.[107] However, a recent meta-analysis suggests harm from anti-coagulation started early after an embolic stroke.[108] Stroke prevention treatment for atrial fibrillation is determined according to the CHADS/CHADS2 system. The most widely used anticoagulant to prevent thromboembolic stroke in patients with nonvalvular atrial fibrillation is the oral agent warfarin while a number of newer agents including dabigatran are alternatives which do not require prothrombin time monitoring.[106]
Anticoagulants, when used following stroke, should not be stopped for dental procedures.[109]
If studies show carotid stenosis, and the person has residual function in the affected side, carotid endarterectomy (surgical removal of the stenosis) may decrease the risk of recurrence if performed rapidly after stroke.
Management
Ischemic stroke
Definitive therapy is aimed at removing the blockage by breaking the clot down (thrombolysis), or by removing it mechanically (thrombectomy). The philosophical premise underlying the importance of rapid stroke intervention was crystallized as Time is Brain! in the early 1990s.[110] Years later, that same idea, that rapid cerebral blood flow restoration results in fewer brain cells dying, has been proved and quantified.[111]
Tight blood sugar control in the first few hours does not improve outcomes and may cause harm.[112] High blood pressure is also not typically lowered as this has not been found to be helpful.[113]
Thrombolysis
Thrombolysis, such as with recombinant tissue plasminogen activator (rtPA), in acute ischemic stroke, when given within three hours of symptom onset results in an overall benefit of 10% with respect to living without disability.[114][115] It does not, however, improve chances of survival.[114] Benefit is greater the earlier it is used.[116] Between three and four and a half hours the effects are less clear.[117][118][119] A 2014 review found a 5% increase in the number of people living without disability at three to six months; however, there was a 2% increased risk of death in the short term.[115] After four and a half hours thrombolysis worsens outcomes.[117] These benefits or lack of benefits occurred regardless of the age of the person treated.[120] There is no reliable way to determine who will have an intracranial hemorrhage post treatment versus who will not.[121]
Its use is endorsed by the American Heart Association and the American Academy of Neurology as the recommended treatment for acute stroke within three hours of onset of symptoms as long as there are not other contraindications (such as abnormal lab values, high blood pressure, or recent surgery). This position for tPA is based upon the findings of two studies by one group of investigators[122] which showed that tPA improves the chances for a good neurological outcome. When administered within the first three hours thrombolysis improves functional outcome without affecting mortality.[123] 6.4% of people with large strokes developed substantial brain hemorrhage as a complication from being given tPA thus part of the reason for increased short term mortality.[124] Additionally, the American Academy of Emergency Medicine states that objective evidence regarding the efficacy, safety, and applicability of tPA for acute ischemic stroke is insufficient to warrant its classification as standard of care.[125] Intra-arterial fibrinolysis, where a catheter is passed up an artery into the brain and the medication is injected at the site of thrombosis, has been found to improve outcomes in people with acute ischemic stroke.[126]
Hemicraniectomy
Large territory strokes can cause significant brain swelling with secondary brain injury in surrounding tissue. This phenomenon is mainly encountered in strokes of the middle cerebral artery territory, and is also called "malignant cerebral infarction" because it carries a dismal prognosis. Relief of the pressure may be attempted with medication, but some require hemicraniectomy, the temporary surgical removal of the skull on one side of the head. This decreases the risk of death, although some more people survive with disability who would otherwise have died.[127]
Hemorrhagic stroke
People with intracerebral hemorrhage require neurosurgical evaluation to detect and treat the cause of the bleeding, although many may not need surgery. Anticoagulants and antithrombotics, key in treating ischemic stroke, can make bleeding worse. People are monitored for changes in the level of consciousness, and their blood pressure, blood sugar, and oxygenation are kept at optimum levels.
Stroke unit
Ideally, people who have had a stroke are admitted to a "stroke unit", a ward or dedicated area in hospital staffed by nurses and therapists with experience in stroke treatment. It has been shown that people admitted to a stroke unit have a higher chance of surviving than those admitted elsewhere in hospital, even if they are being cared for by doctors without experience in stroke.[2][128]
When an acute stroke is suspected by history and physical examination, the goal of early assessment is to determine the cause. Treatment varies according to the underlying cause of the stroke, thromboembolic (ischemic) or hemorrhagic.
Rehabilitation
Stroke rehabilitation is the process by which those with disabling strokes undergo treatment to help them return to normal life as much as possible by regaining and relearning the skills of everyday living. It also aims to help the survivor understand and adapt to difficulties, prevent secondary complications and educate family members to play a supporting role.
A rehabilitation team is usually multidisciplinary as it involves staff with different skills working together to help the patient. These include physicians trained in rehabilitation medicine, clinical pharmacists, nursing staff, physiotherapists, occupational therapists, speech and language therapists, and orthotists. Some teams may also include psychologists and social workers, since at least one third of the people manifest post stroke depression. Validated instruments such as the Barthel scale may be used to assess the likelihood of a stroke patient being able to manage at home with or without support subsequent to discharge from hospital.
Good nursing care is fundamental in maintaining skin care, feeding, hydration, positioning, and monitoring vital signs such as temperature, pulse, and blood pressure. Stroke rehabilitation begins almost immediately.
For most people with stroke, physical therapy (PT), occupational therapy (OT) and speech-language pathology (SLP) are the cornerstones of the rehabilitation process. Often, assistive technology such as wheelchairs, walkers and canes may be beneficial. Many mobility problems can be improved by the use of ankle foot orthoses.[129] PT and OT have overlapping areas of expertise, however PT focuses on joint range of motion and strength by performing exercises and re-learning functional tasks such as bed mobility, transferring, walking and other gross motor functions. Physiotherapists can also work with patients to improve awareness and use of the hemiplegic side. Rehabilitation involves working on the ability to produce strong movements or the ability to perform tasks using normal patterns. Emphasis is often concentrated on functional tasks and patient’s goals. One example physiotherapists employ to promote motor learning involves constraint-induced movement therapy. Through continuous practice the patient relearns to use and adapt the hemiplegic limb during functional activities to create lasting permanent changes.[130] OT is involved in training to help relearn everyday activities known as the Activities of daily living (ADLs) such as eating, drinking, dressing, bathing, cooking, reading and writing, and toileting. Speech and language therapy is appropriate for patients with the speech production disorders: dysarthria[131] and apraxia of speech,[132] aphasia,[133] cognitive-communication impairments and/or dysphagia (problems with swallowing).
Patients may have particular problems, such as dysphagia, which can cause swallowed material to pass into the lungs and cause aspiration pneumonia. The condition may improve with time, but in the interim, a nasogastric tube may be inserted, enabling liquid food to be given directly into the stomach. If swallowing is still deemed unsafe, then a percutaneous endoscopic gastrostomy (PEG) tube is passed and this can remain indefinitely.
Treatment of spasticity related to stroke often involves early mobilizations, commonly performed by a physiotherapist, combined with elongation of spastic muscles and sustained stretching through various positionings.[26] Gaining initial improvement in range of motion is often achieved through rhythmic rotational patterns associated with the affected limb.[26] After full range has been achieved by the therapist, the limb should be positioned in the lengthened positions to prevent against further contractures, skin breakdown, and disuse of the limb with the use of splints or other tools to stabilize the joint.[26] Cold in the form of ice wraps or ice packs have been proven to briefly reduce spasticity by temporarily dampening neural firing rates.[26] Electrical stimulation to the antagonist muscles or vibrations has also been used with some success.[26]
Stroke rehabilitation should be started as quickly as possible and can last anywhere from a few days to over a year. Most return of function is seen in the first few months, and then improvement falls off with the "window" considered officially by U.S. state rehabilitation units and others to be closed after six months, with little chance of further improvement. However, patients have been known to continue to improve for years, regaining and strengthening abilities like writing, walking, running, and talking. Daily rehabilitation exercises should continue to be part of the stroke patient's routine. Complete recovery is unusual but not impossible and most patients will improve to some extent: proper diet and exercise are known to help the brain to recover.
Some current and future therapy methods include the use of virtual reality and video games for rehabilitation. These forms of rehabilitation offer potential for motivating patients to perform specific therapy tasks that many other forms do not.[134] Many clinics and hospitals are adopting the use of these off-the-shelf devices for exercise, social interaction and rehabilitation because they are affordable, accessible and can be used within the clinic and home.[134]
Other novel non-invasive rehabilitation methods are currently being developed to augment physical therapy to improve motor function of stroke patients, such as transcranial magnetic stimulation (TMS) and transcranial direct-current stimulation (tDCS)[135] and robotic therapies.[136]
A stroke can also reduce people's general fitness.[137] Reduced fitness can reduce capacity for rehabilitation as well as general health.[138] A systematic review found that there are inadequate long-term data about the effects of exercise and training on death, dependence and disability after a stroke.[137] However, cardiorespiratory training added to walking programs in rehabilitation can improve speed, tolerance and independence during walking.[137]
Prognosis
Disability affects 75% of stroke survivors enough to decrease their employability.[139] Stroke can affect people physically, mentally, emotionally, or a combination of the three. The results of stroke vary widely depending on size and location of the lesion.[140] Dysfunctions correspond to areas in the brain that have been damaged.
Some of the physical disabilities that can result from stroke include muscle weakness, numbness, pressure sores, pneumonia, incontinence, apraxia (inability to perform learned movements), difficulties carrying out daily activities, appetite loss, speech loss, vision loss and pain. If the stroke is severe enough, or in a certain location such as parts of the brainstem, coma or death can result.
Emotional problems following a stroke can be due to direct damage to emotional centers in the brain or from frustration and difficulty adapting to new limitations. Post-stroke emotional difficulties include anxiety, panic attacks, flat affect (failure to express emotions), mania, apathy and psychosis. Other difficulties may include a decreased ability to communicate emotions through facial expression, body language and voice.[141]
Disruption in self-identity, relationships with others, and emotional well-being can lead to social consequences after stroke due to the lack of ability to communicate. Many people who experience communication impairments after a stroke find it more difficult to cope with the social issues rather than physical impairments. Broader aspects of care must address the emotional impact speech impairment has on those who experience difficulties with speech after a stroke.[142] Those who experience a stroke are at risk for paralysis which could result in a self disturbed body image which may also lead to other social issues.[143]
30 to 50% of stroke survivors suffer post-stroke depression, which is characterized by lethargy, irritability, sleep disturbances, lowered self-esteem and withdrawal.[144] Depression can reduce motivation and worsen outcome, but can be treated with antidepressants.
Emotional lability, another consequence of stroke, causes the person to switch quickly between emotional highs and lows and to express emotions inappropriately, for instance with an excess of laughing or crying with little or no provocation. While these expressions of emotion usually correspond to the person's actual emotions, a more severe form of emotional lability causes the affected person to laugh and cry pathologically, without regard to context or emotion.[139] Some people show the opposite of what they feel, for example crying when they are happy.[145] Emotional lability occurs in about 20% of those who have had a stroke.
Cognitive deficits resulting from stroke include perceptual disorders, aphasia,[146] dementia,[147] and problems with attention[148] and memory.[149] A stroke sufferer may be unaware of his or her own disabilities, a condition called anosognosia. In a condition called hemispatial neglect, the affected person is unable to attend to anything on the side of space opposite to the damaged hemisphere.
Cognitive and psychological outcome after a stroke can be affected by the age at which the stroke happened, pre-stroke baseline intellectual functioning, psychiatric history and whether there is pre-existing brain pathology.[150]
Up to 10% of people following a stroke develop seizures, most commonly in the week subsequent to the event; the severity of the stroke increases the likelihood of a seizure.[151][152]
Epidemiology

no data
<250
250-425
425-600
600-775
775-950
950-1125
|
1125-1300
1300-1475
1475-1650
1650-1825
1825-2000
>2000
|
Stroke was the second most frequent cause of death worldwide in 2011, accounting for 6.2 million deaths (~11% of the total).[154] Approximately 17 million people had a stroke in 2010 and 33 million people have previously had a stroke and were still alive.[8] Between 1990 and 2010 the number of strokes decrease by approximately 10% in the developed world and increased by 10% in the developing world.[8] Overall, two thirds of strokes occurred in those over 65 years old.[8]
It is ranked after heart disease and before cancer.[2] In the United States stroke is a leading cause of disability, and recently declined from the third leading to the fourth leading cause of death.[155] Geographic disparities in stroke incidence have been observed, including the existence of a "stroke belt" in the southeastern United States, but causes of these disparities have not been explained.
The incidence of stroke increases exponentially from 30 years of age, and etiology varies by age.[156] Advanced age is one of the most significant stroke risk factors. 95% of strokes occur in people age 45 and older, and two-thirds of strokes occur in those over the age of 65.[31][144] A person's risk of dying if he or she does have a stroke also increases with age. However, stroke can occur at any age, including in childhood.
Family members may have a genetic tendency for stroke or share a lifestyle that contributes to stroke. Higher levels of Von Willebrand factor are more common amongst people who have had ischemic stroke for the first time.[157] The results of this study found that the only significant genetic factor was the person's blood type. Having had a stroke in the past greatly increases one's risk of future strokes.
Men are 25% more likely to suffer strokes than women,[31] yet 60% of deaths from stroke occur in women.[145] Since women live longer, they are older on average when they have their strokes and thus more often killed.[31] Some risk factors for stroke apply only to women. Primary among these are pregnancy, childbirth, menopause, and the treatment thereof (HRT).
History

Episodes of stroke and familial stroke have been reported from the 2nd millennium BC onward in ancient Mesopotamia and Persia.[158] Hippocrates (460 to 370 BC) was first to describe the phenomenon of sudden paralysis that is often associated with ischemia. Apoplexy, from the Greek word meaning "struck down with violence," first appeared in Hippocratic writings to describe this phenomenon.[159][160] The word stroke was used as a synonym for apoplectic seizure as early as 1599,[161] and is a fairly literal translation of the Greek term.
In 1658, in his Apoplexia, Johann Jacob Wepfer (1620–1695) identified the cause of hemorrhagic stroke when he suggested that people who had died of apoplexy had bleeding in their brains.[31][159] Wepfer also identified the main arteries supplying the brain, the vertebral and carotid arteries, and identified the cause of a type of ischemic stroke known as a cerebral infarction when he suggested that apoplexy might be caused by a blockage to those vessels.[31] Rudolf Virchow first described the mechanism of thromboembolism as a major factor.[162]
The term cerebrovascular accident was introduced in 1927, reflecting a "growing awareness and acceptance of vascular theories and (...) recognition of the consequences of a sudden disruption in the vascular supply of the brain".[163] Its use is now discouraged by a number of neurology textbooks, reasoning that the connotation of fortuitousness carried by the word accident insufficiently highlights the modifiability of the underlying risk factors.[164][165][166] Cerebrovascular insult may be used interchangeably.[167]
The term brain attack was introduced for use to underline the acute nature of stroke according to the American Stroke Association,[167] who since 1990 have used the term,[168] and is used colloquially to refer to both ischemic as well as hemorrhagic stroke.[169]
Research
Angioplasty and stenting
Angioplasty and stenting have begun to be looked at as possible viable options in treatment of acute ischemic stroke. Intra-cranial stenting in symptomatic intracranial arterial stenosis, the rate of technical success (reduction to stenosis of <50%) ranged from 90-98%, and the rate of major peri-procedural complications ranged from 4-10%. The rates of restenosis and/or stroke following the treatment were also favorable. This data suggests that a randomized controlled trial is needed to more completely evaluate the possible therapeutic advantage of this preventative measure.[170]
Mechanical thrombectomy

Removal of the clot may be attempted in those where it occurs within a large blood vessel and may be an option for those who either are not eligible for or do not improve with intravenous thrombolytics.[171] Significant complications occur in about 7%.[172]
Neuroprotection
Drugs that scavenge reactive oxygen species, inhibit programmed cell death, or inhibit excitatory neurotransmitters have been shown experimentally to reduce tissue injury caused by ischemia. Agents that work in this way are referred to as being neuroprotective. Until recently, human clinical trials with neuroprotective agents have failed, with the probable exception of deep barbiturate coma. However, more recently NXY-059, the disulfonyl derivative of the radical-scavenging phenylbutylnitrone, is reported to be neuroprotective in stroke.[173] This agent appears to work at the level of the blood vessel lining or endothelium. Unfortunately, after producing favorable results in one large-scale clinical trial, a second trial failed to show favorable results.[31] Benefit of NXY-059 is questionable.[174]
Hyperbaric oxygen therapy has been studied as a possible protective measure, but is currently not thought to be beneficial.[175]
See also
References
- ↑ 1.0 1.1 1.2 "What Is a Stroke?". http://www.nhlbi.nih.gov/''. March 26, 2014. Retrieved 26 February 2015.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 2.10 2.11 2.12 Donnan GA, Fisher M, Macleod M, Davis SM (May 2008). "Stroke". Lancet 371 (9624): 1612–23. doi:10.1016/S0140-6736(08)60694-7. PMID 18468545.
- ↑ 3.0 3.1 3.2 3.3 "What Are the Signs and Symptoms of a Stroke?". http://www.nhlbi.nih.gov''. March 26, 2014. Retrieved 27 February 2015.
- ↑ 4.0 4.1 "Who Is at Risk for a Stroke?". http://www.nhlbi.nih.gov''. March 26, 2014. Retrieved 27 February 2015.
- ↑ 5.0 5.1 5.2 "Types of Stroke". http://www.nhlbi.nih.gov''. March 26, 2014. Retrieved 27 February 2015.
- ↑ Feigin VL, Rinkel GJ, Lawes CM, Algra A, Bennett DA, van Gijn J, Anderson CS (2005). "Risk factors for subarachnoid hemorrhage: an updated systematic review of epidemiological studies". Stroke 36 (12): 2773–80. doi:10.1161/01.STR.0000190838.02954.e8. PMID 16282541.
- ↑ "How Is a Stroke Diagnosed?". http://www.nhlbi.nih.gov''. March 26, 2014. Retrieved 27 February 2015.
- ↑ 8.0 8.1 8.2 8.3 8.4 Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson L, Truelsen T, O'Donnell M, Venketasubramanian N, Barker-Collo S, Lawes CM, Wang W, Shinohara Y, Witt E, Ezzati M, Naghavi M, Murray C (2014). "Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010". Lancet 383 (9913): 245–54. doi:10.1016/S0140-6736(13)61953-4. PMID 24449944.
- ↑ 9.0 9.1 GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013.". Lancet 385: 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ↑ "Brain Basics: Preventing Stroke". National Institute of Neurological Disorders and Stroke. Retrieved 2009-10-24.
- ↑ World Health Organisation (1978). Cerebrovascular Disorders (Offset Publications). Geneva: World Health Organization. ISBN 92-4-170043-2. OCLC 4757533.
- ↑ Kidwell CS, Warach S (December 2003). "Acute ischemic cerebrovascular syndrome: diagnostic criteria". Stroke 34 (12): 2995–8. doi:10.1161/01.STR.0000098902.69855.A9. PMID 14605325.
- ↑ Shuaib A, Hachinski VC (September 1991). "Mechanisms and management of stroke in the elderly". CMAJ 145 (5): 433–43. PMC 1335826. PMID 1878825.
- ↑ 14.0 14.1 Stam J (April 2005). "Thrombosis of the cerebral veins and sinuses". The New England Journal of Medicine 352 (17): 1791–8. doi:10.1056/NEJMra042354. PMID 15858188.
- ↑ Guercini F, Acciarresi M, Agnelli G, Paciaroni M (April 2008). "Cryptogenic stroke: time to determine aetiology". Journal of Thrombosis and Haemostasis 6 (4): 549–54. doi:10.1111/j.1538-7836.2008.02903.x. PMID 18208534.
- ↑ Bamford J, Sandercock P, Dennis M, Burn J, Warlow C (June 1991). "Classification and natural history of clinically identifiable subtypes of cerebral infarction". Lancet 337 (8756): 1521–6. doi:10.1016/0140-6736(91)93206-O. PMID 1675378. Later publications distinguish between "syndrome" and "infarct", based on evidence from imaging. "Syndrome" may be replaced by "hemorrhage" if imaging demonstrates a bleed. See Internet Stroke Center. "Oxford Stroke Scale". Retrieved 2008-11-14.
- ↑ Bamford JM (2000). "The role of the clinical examination in the subclassification of stroke". Cerebrovascular Diseases. 10 Suppl 4: 2–4. doi:10.1159/000047582. PMID 11070389.
- ↑ Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE (January 1993). "Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment". Stroke 24 (1): 35–41. doi:10.1161/01.STR.24.1.35. PMID 7678184.
- ↑ Osterweil,, Neil. "Methamphetamine induced ischemic strokes". Medpagetoday. Retrieved 24 August 2013.
- ↑ Goldstein LB, Simel DL (May 2005). "Is this patient having a stroke?". JAMA 293 (19): 2391–402. doi:10.1001/jama.293.19.2391. PMID 15900010.
- ↑ Harbison J, Massey A, Barnett L, Hodge D, Ford GA (June 1999). "Rapid ambulance protocol for acute stroke". Lancet 353 (9168): 1935. doi:10.1016/S0140-6736(99)00966-6. PMID 10371574.
- ↑ Kidwell CS, Saver JL, Schubert GB, Eckstein M, Starkman S (1998). "Design and retrospective analysis of the Los Angeles Prehospital Stroke Screen (LAPSS)". Prehospital Emergency Care 2 (4): 267–73. doi:10.1080/10903129808958878. PMID 9799012.
- ↑ Kothari RU, Pancioli A, Liu T, Brott T, Broderick J (April 1999). "Cincinnati Prehospital Stroke Scale: reproducibility and validity". Annals of Emergency Medicine 33 (4): 373–8. doi:10.1016/S0196-0644(99)70299-4. PMID 10092713.
- ↑ 24.0 24.1 National Institute for Health and Clinical Excellence. Clinical guideline 68: Stroke. London, 2008.
- ↑ Nor AM, Davis J, Sen B, Shipsey D, Louw SJ, Dyker AG, Davis M, Ford GA (November 2005). "The Recognition of Stroke in the Emergency Room (ROSIER) scale: development and validation of a stroke recognition instrument". Lancet Neurology 4 (11): 727–34. doi:10.1016/S1474-4422(05)70201-5. PMID 16239179.
- ↑ 26.0 26.1 26.2 26.3 26.4 26.5 O'Sullivan, Susan.B (2007). "Stroke". In O'Sullivan, S.B., and Schmitz, T.J. Physical Rehabilitation 5. Philadelphia: F.A. Davis Company. p. 719.
- ↑ "Thrombus". MedlinePlus. U.S. National Library of Medicine.
- ↑ "Circle of Willis". The Internet Stroke Center.
- ↑ "Brain anaurysm - Introduction". NHS Choices.
- ↑ Fisher CM (1968-12-18). "The arterial lesions underlying lacunes". Acta Neuropathologica 12 (1): 1–15. doi:10.1007/BF00685305. PMID 5708546.
- ↑ 31.0 31.1 31.2 31.3 31.4 31.5 31.6 31.7 National Institute of Neurological Disorders and Stroke (NINDS) (1999). "Stroke: Hope Through Research". National Institutes of Health.
- ↑ Shah, A. S. V.; Lee, K. K.; McAllister, D. A.; Hunter, A.; Nair, H.; Whiteley, W.; Langrish, J. P.; Newby, D. E.; Mills, N. L. (24 March 2015). "Short term exposure to air pollution and stroke: systematic review and meta-analysis". BMJ 350 (mar23 11): h1295–h1295. doi:10.1136/bmj.h1295.
- ↑ 33.0 33.1 Robbins and Cotran Pathologic Basis of Disease, Professional Edition. (8th ed. ed.). Philadelphia, Pa: Elsevier. 2009. ISBN 978-1-4377-0792-2.
|first1=missing|last1=in Authors list (help) - ↑ Ay H, Furie KL, Singhal A, Smith WS, Sorensen AG, Koroshetz WJ (November 2005). "An evidence-based causative classification system for acute ischemic stroke". Annals of Neurology 58 (5): 688–97. doi:10.1002/ana.20617. PMID 16240340.
- ↑ "Hypertension".
- ↑ Miwa K, Hoshi T, Hougaku H, Tanaka M, Furukado S, Abe Y, Okazaki S, Sakaguchi M, Sakoda S, Kitagawa K (2010). "Silent cerebral infarction is associated with incident stroke and TIA independent of carotid intima-media thickness". Intern. Med. 49 (9): 817–22. doi:10.2169/internalmedicine.49.3211. PMID 20453400.
- ↑ 37.0 37.1 Herderscheê D, Hijdra A, Algra A, Koudstaal PJ, Kappelle LJ, van Gijn J (September 1992). "Silent stroke in patients with transient ischemic attack or minor ischemic stroke. The Dutch TIA Trial Study Group". Stroke 23 (9): 1220–4. doi:10.1161/01.STR.23.9.1220. PMID 1519274.
- ↑ Leary MC, Saver JL (2003). "Annual incidence of first silent stroke in the United States: a preliminary estimate". Cerebrovasc. Dis. 16 (3): 280–5. doi:10.1159/000071128. PMID 12865617.
- ↑ Vermeer SE, Koudstaal PJ, Oudkerk M, Hofman A, Breteler MM (January 2002). "Prevalence and risk factors of silent brain infarcts in the population-based Rotterdam Scan Study". Stroke 33 (1): 21–5. doi:10.1161/hs0102.101629. PMID 11779883.
- ↑ Deb P, Sharma S, Hassan KM (June 2010). "Pathophysiologic mechanisms of acute ischemic stroke: An overview with emphasis on therapeutic significance beyond thrombolysis". Pathophysiology : the official journal of the International Society for Pathophysiology / ISP 17 (3): 197–218. doi:10.1016/j.pathophys.2009.12.001. PMID 20074922.
- ↑ Richard S. Snell (2006). Clinical neuroanatomy, 6. ed. Lippincott Williams & Wilkins, Philadelphia. pp. 478–485. ISBN 978-963-226-293-2.
- ↑ Brunner and Suddarth's Textbook on Medical-Surgical Nursing, 11th Edition
- ↑ Longo, ed. Dan L. Longo ... [et et al. (2012). Harrison's principles of internal medicine. (18th ed. ed.). New York: McGraw-Hill. pp. Chapter 370. ISBN 978-0071748896.
- ↑ Longo, ed. Dan L. Longo ... [et et al. (2012). Harrison's principles of internal medicine. (18th ed. ed.). New York: McGraw-Hill. pp. Chapter 370. ISBN 978-0071748896.
- ↑ 45.0 45.1 Wang J (December 2010). "Preclinical and clinical research on inflammation after intracerebral hemorrhage". Prog. Neurobiol. 92 (4): 463–77. doi:10.1016/j.pneurobio.2010.08.001. PMC 2991407. PMID 20713126.
- ↑ Hill MD (November 2005). "Diagnostic biomarkers for stroke: a stroke neurologist's perspective". Clinical Chemistry 51 (11): 2001–2. doi:10.1373/clinchem.2005.056382. PMID 16244286.
- ↑ Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, Hill MD, Patronas N, Latour L, Warach S (January 2007). "Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison". Lancet 369 (9558): 293–8. doi:10.1016/S0140-6736(07)60151-2. PMC 1859855. PMID 17258669.
- ↑ Kidwell CS, Chalela JA, Saver JL, Starkman S, Hill MD, Demchuk AM, Butman JA, Patronas N, Alger JR, Latour LL, Luby ML, Baird AE, Leary MC, Tremwel M, Ovbiagele B, Fredieu A, Suzuki S, Villablanca JP, Davis S, Dunn B, Todd JW, Ezzeddine MA, Haymore J, Lynch JK, Davis L, Warach S (October 2004). "Comparison of MRI and CT for detection of acute intracerebral hemorrhage". JAMA 292 (15): 1823–30. doi:10.1001/jama.292.15.1823. PMID 15494579.
- ↑ 49.0 49.1 Straus SE, Majumdar SR, McAlister FA (September 2002). "New evidence for stroke prevention: scientific review". JAMA 288 (11): 1388–95. doi:10.1001/jama.288.11.1388. PMID 12234233.
- ↑ Goldstein LB, Adams R, Alberts MJ, Appel LJ, Brass LM, Bushnell CD, Culebras A, Degraba TJ, Gorelick PB, Guyton JR, Hart RG, Howard G, Kelly-Hayes M, Nixon JV, Sacco RL (June 2006). "Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group: the American Academy of Neurology affirms the value of this guideline". Stroke 37 (6): 1583–633. doi:10.1161/01.STR.0000223048.70103.F1. PMID 16675728.
- ↑ "Use of Aspirin for Primary Prevention of Heart Attack and Stroke". FDA. 05/02/2014. Retrieved 11 June 2014. Check date values in:
|date=(help) - ↑ 52.0 52.1 52.2 NPS Prescribing Practice Review 44: Antiplatelets and anticoagulants in stroke prevention (2009). Available at nps.org.au
- ↑ 53.0 53.1 Antithrombotic Trialists' Collaboration (January 2002). "Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients". BMJ 324 (7329): 71–86. doi:10.1136/bmj.324.7329.71. PMC 64503. PMID 11786451.
- ↑ Jonas, Daniel E.; Feltner, Cynthia; Amick, Halle R.; Sheridan, Stacey; Zheng, Zhi-Jie; Watford, Daniel J.; Carter, Jamie L.; Rowe, Cassandra J.; Harris, Russell (Jul 8, 2014). "Screening for Asymptomatic Carotid Artery Stenosis: A Systematic Review and Meta-analysis for the U.S. Preventive Services Task Force.". Annals of internal medicine 161: 336. doi:10.7326/M14-0530. PMID 25004169.
- ↑ Medical Research Council Working Party (July 1985). "MRC trial of treatment of mild hypertension: principal results". British Medical Journal 291 (6488): 97–104. doi:10.1136/bmj.291.6488.97. PMC 1416260. PMID 2861880.
- ↑ Thomson R (2009). "Evidence based implementation of complex interventions". BMJ 339: b3124. doi:10.1136/bmj.b3124. PMID 19675081.
- ↑ Hankey GJ (August 1999). "Smoking and risk of stroke". Journal of Cardiovascular Risk 6 (4): 207–11. PMID 10501270.
- ↑ Wannamethee SG, Shaper AG, Whincup PH, Walker M (July 1995). "Smoking cessation and the risk of stroke in middle-aged men". JAMA 274 (2): 155–60. doi:10.1001/jama.274.2.155. PMID 7596004.
- ↑ Reynolds K, Lewis B, Nolen JD, Kinney GL, Sathya B, He J, Lewis BL (February 2003). "Alcohol consumption and risk of stroke: a meta-analysis". JAMA 289 (5): 579–88. doi:10.1001/jama.289.5.579. PMID 12578491.
- ↑ Sloan MA, Kittner SJ, Rigamonti D, Price TR (September 1991). "Occurrence of stroke associated with use/abuse of drugs". Neurology 41 (9): 1358–64. doi:10.1212/WNL.41.9.1358. PMID 1891081.
- ↑ Larsson SC, Virtamo J, Wolk A (2011). "Red meat consumption and risk of stroke in Swedish men". American Journal of Clinical Nutrition 94 (2): 417–421. doi:10.3945/ajcn.111.015115. PMID 21653800.
- ↑ "Stroke Risk Factors". American Heart Association. 2007. Retrieved January 22, 2007.
- ↑ Gorelick PB (1987). "Alcohol and stroke". Stroke; a Journal of Cerebral Circulation 18 (1): 268–71. doi:10.1161/01.STR.18.1.268. PMID 3810763.
- ↑ al.], ed. Dan L. Longo ... [et (2012). Harrison's principles of internal medicine. (18th ed. ed.). New York: McGraw-Hill. pp. Chapter 370. ISBN 007174889X.
- ↑ Westover AN, McBride S, Haley RW (April 2007). "Stroke in young adults who abuse amphetamines or cocaine: a population-based study of hospitalized patients". Archives of General Psychiatry 64 (4): 495–502. doi:10.1001/archpsyc.64.4.495. PMID 17404126.
- ↑ Ezekowitz JA, Straus SE, Majumdar SR, McAlister FA (December 2003). "Stroke: strategies for primary prevention". American Family Physician 68 (12): 2379–86. PMID 14705756.
- ↑ 67.0 67.1 67.2 67.3 Ederle J, Brown MM (October 2006). "The evidence for medicine versus surgery for carotid stenosis". European Journal of Radiology 60 (1): 3–7. doi:10.1016/j.ejrad.2006.05.021. PMID 16920313.
- ↑ Whisnant JP (1996). "Effectiveness versus efficacy of treatment of hypertension for stroke prevention". Neurology 46 (2): 301–7. doi:10.1212/WNL.46.2.301. PMID 8614485.
- ↑ Law MR, Morris JK, Wald NJ (May 19, 2009). "Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies". BMJ (Clinical research ed.) 338: b1665. doi:10.1136/bmj.b1665. PMC 2684577. PMID 19454737.
- ↑ Psaty BM, Lumley T, Furberg CD, Schellenbaum G, Pahor M, Alderman MH, Weiss NS (2003). "Health outcomes associated with various antihypertensive therapies used as first-line agents: a network meta-analysis". JAMA 289 (19): 2534–44. doi:10.1001/jama.289.19.2534. PMID 12759325.
- ↑ 71.0 71.1 "Cholesterol, diastolic blood pressure, and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts. Prospective studies collaboration". Lancet 346 (8991–8992): 1647–53. 1995. doi:10.1016/S0140-6736(95)92836-7. PMID 8551820.
- ↑ Gueyffier F, Boissel JP, Boutitie F, Pocock S, Coope J, Cutler J, Ekbom T, Fagard R, Friedman L, Kerlikowske K, Perry M, Prineas R, Schron E (1997). "Effect of antihypertensive treatment in patients having already suffered from stroke. Gathering the evidence. The INDANA (INdividual Data ANalysis of Antihypertensive intervention trials) Project Collaborators". Stroke 28 (12): 2557–62. doi:10.1161/01.STR.28.12.2557. PMID 9412649.
- ↑ Gueyffier F, Bulpitt C, Boissel JP, Schron E, Ekbom T, Fagard R, Casiglia E, Kerlikowske K, Coope J (1999). "Antihypertensive drugs in very old people: a subgroup meta-analysis of randomised controlled trials. INDANA Group". Lancet 353 (9155): 793–6. doi:10.1016/S0140-6736(98)08127-6. PMID 10459960.
- ↑ Staessen JA, Gasowski J, Wang JG, Thijs L, Den Hond E, Boissel JP, Coope J, Ekbom T, Gueyffier F, Liu L, Kerlikowske K, Pocock S, Fagard RH (2000). "Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials". Lancet 355 (9207): 865–72. doi:10.1016/S0140-6736(99)07330-4. PMID 10752701.
- ↑ Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, Stoyanovsky V, Antikainen RL, Nikitin Y, Anderson C, Belhani A, Forette F, Rajkumar C, Thijs L, Banya W, Bulpitt CJ (2008). "Treatment of Hypertension in Patients 80 Years of Age or Older". N. Engl. J. Med. 358 (18): 1887–98. doi:10.1056/NEJMoa0801369. PMID 18378519.
- ↑ Neal B, MacMahon S, Chapman N (2000). "Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists' Collaboration". Lancet 356 (9246): 1955–64. doi:10.1016/S0140-6736(00)03307-9. PMID 11130523.
- ↑ The Allhat Officers And Coordinators For The Allhat Collaborative Research Group, (2002). "Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)". JAMA 288 (23): 2981–97. doi:10.1001/jama.288.23.2981. PMID 12479763.
- ↑ De Lima, LG; Saconato, H; Atallah, AN; da Silva, EM (Oct 15, 2014). "Beta-blockers for preventing stroke recurrence.". The Cochrane database of systematic reviews 10: CD007890. doi:10.1002/14651858.CD007890.pub3. PMID 25317988.
- ↑ Iso H, Jacobs DR, Wentworth D, Neaton JD, Cohen JD (1989). "Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial". N. Engl. J. Med. 320 (14): 904–10. doi:10.1056/NEJM198904063201405. PMID 2619783.
- ↑ 80.0 80.1 O'Regan C, Wu P, Arora P, Perri D, Mills EJ (2008). "Statin therapy in stroke prevention: a meta-analysis involving 121,000 patients". Am. J. Med. 121 (1): 24–33. doi:10.1016/j.amjmed.2007.06.033. PMID 18187070.
- ↑ Hebert PR, Gaziano JM, Hennekens CH (1995). "An overview of trials of cholesterol lowering and risk of stroke". Arch. Intern. Med. 155 (1): 50–5. doi:10.1001/archinte.155.1.50. PMID 7802520.
- ↑ "Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group". Lancet 352 (9131): 837–53. 1998. doi:10.1016/S0140-6736(98)07019-6. PMID 9742976.
- ↑ Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, Skene AM, Tan MH, Lefèbvre PJ, Murray GD, Standl E, Wilcox RG, Wilhelmsen L, Betteridge J, Birkeland K, Golay A, Heine RJ, Korányi L, Laakso M, Mokán M, Norkus A, Pirags V, Podar T, Scheen A, Scherbaum W, Schernthaner G, Schmitz O, Skrha J, Smith U, Taton J (2005). "Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial". Lancet 366 (9493): 1279–89. doi:10.1016/S0140-6736(05)67528-9. PMID 16214598.
- ↑ Johnson ES, Lanes SF, Wentworth CE, Satterfield MH, Abebe BL, Dicker LW (1999). "A metaregression analysis of the dose-response effect of aspirin on stroke". Arch. Intern. Med. 159 (11): 1248–53. doi:10.1001/archinte.159.11.1248. PMID 10371234.
- ↑ 85.0 85.1 Hankey GJ, Sudlow CL, Dunbabin DW (2000). Hankey, Graeme, ed. "Thienopyridine derivatives (ticlopidine, clopidogrel) versus aspirin for preventing stroke and other serious vascular events in high vascular risk patients". Cochrane Database Syst Rev (2): CD001246. doi:10.1002/14651858.CD001246. PMID 10796426.
- ↑ Halkes PH, van Gijn J, Kappelle LJ, Koudstaal PJ, Algra A (2006). "Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial". Lancet 367 (9523): 1665–73. doi:10.1016/S0140-6736(06)68734-5. PMID 16714187.
- ↑ Wolf PA, Abbott RD, Kannel WB (1987). "Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study". Arch. Intern. Med. 147 (9): 1561–4. doi:10.1001/archinte.147.9.1561. PMID 3632164.
- ↑ Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Smith SC, Jacobs AK, Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo JL, Zamorano JL (2006). "ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation 114 (7): e257–354. doi:10.1161/CIRCULATIONAHA.106.177292. PMID 16908781.
- ↑ Halkes PH, van Gijn J, Kappelle LJ, Koudstaal PJ, Algra A (2007). "Medium intensity oral anticoagulants versus aspirin after cerebral ischaemia of arterial origin (ESPRIT): a randomised controlled trial". Lancet Neurol 6 (2): 115–24. doi:10.1016/S1474-4422(06)70685-8. PMID 17239798.
- ↑ Hart RG, Halperin JL, McBride R, Benavente O, Man-Son-Hing M, Kronmal RA (2000). "Aspirin for the primary prevention of stroke and other major vascular events: meta-analysis and hypotheses". Arch. Neurol. 57 (3): 326–32. doi:10.1001/archneur.57.3.326. PMID 10714657.
- ↑ Bartolucci AA, Howard G (2006). "Meta-analysis of data from the six primary prevention trials of cardiovascular events using aspirin". Am. J. Cardiol. 98 (6): 746–50. doi:10.1016/j.amjcard.2006.04.012. PMID 16950176.
- ↑ Berger JS, Roncaglioni MC, Avanzini F, Pangrazzi I, Tognoni G, Brown DL (2006). "Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials". JAMA 295 (3): 306–13. doi:10.1001/jama.295.3.306. PMID 16418466.
- ↑ Yerman T, Gan WQ, Sin DD (2007). "The influence of gender on the effects of aspirin in preventing myocardial infarction". BMC Med 5: 29. doi:10.1186/1741-7015-5-29. PMC 2131749. PMID 17949479.
- ↑ Rothwell PM, Eliasziw M, Gutnikov SA, Fox AJ, Taylor DW, Mayberg MR, Warlow CP, Barnett HJ (2003). "Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis". Lancet 361 (9352): 107–16. doi:10.1016/S0140-6736(03)12228-3. PMID 12531577.
- ↑ Ringleb PA, Chatellier G, Hacke W, Favre JP, Bartoli JM, Eckstein HH, Mas JL (2008). "Safety of endovascular treatment of carotid artery stenosis compared with surgical treatment: a meta-analysis". J. Vasc. Surg. 47 (2): 350–5. doi:10.1016/j.jvs.2007.10.035. PMID 18241759.
- ↑ Ederle J, Featherstone RL, Brown MM (2007). Brown, Martin M, ed. "Percutaneous transluminal angioplasty and stenting for carotid artery stenosis". Cochrane Database Syst Rev (4): CD000515. doi:10.1002/14651858.CD000515.pub3. PMID 17943745.
- ↑ Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ (2004). "Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery". Lancet 363 (9413): 915–24. doi:10.1016/S0140-6736(04)15785-1. PMID 15043958.
- ↑ Fairhead JF, Mehta Z, Rothwell PM (2005). "Population-based study of delays in carotid imaging and surgery and the risk of recurrent stroke". Neurology 65 (3): 371–5. doi:10.1212/01.wnl.0000170368.82460.b4. PMID 16087900.
- ↑ U.S. Preventive Services Task Force (2007). "Screening for carotid artery stenosis: U.S. Preventive Services Task Force recommendation statement". Ann. Intern. Med. 147 (12): 854–9. doi:10.7326/0003-4819-147-12-200712180-00005. PMID 18087056.
- ↑ Halliday A, Mansfield A, Marro J, Peto C, Peto R, Potter J, Thomas D (2004). "Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial". Lancet 363 (9420): 1491–502. doi:10.1016/S0140-6736(04)16146-1. PMID 15135594.
- ↑ Chambers BR, Donnan GA (2005). Chambers, Brian R, ed. "Carotid endarterectomy for asymptomatic carotid stenosis". Cochrane Database Syst Rev (4): CD001923. doi:10.1002/14651858.CD001923.pub2. PMID 16235289.
- ↑ Spence JD (2006). "Nutrition and stroke prevention". Stroke; a Journal of Cerebral Circulation 37 (9): 2430–5. doi:10.1161/01.STR.0000236633.40160.ee. PMID 16873712.
- ↑ Zhou YH, Tang JY, Wu MJ, Lu J, Wei X, Qin YY, Wang C, Xu JF, He J (2011). Wright, James M, ed. "Effect of folic acid supplementation on cardiovascular outcomes: a systematic review and meta-analysis". PLoS ONE 6 (9): e25142. Bibcode:2011PLoSO...625142Z. doi:10.1371/journal.pone.0025142. PMC 3182189. PMID 21980387.
- ↑ Clarke R, Halsey J, Lewington S, Lonn E, Armitage J, Manson JE, Bønaa KH, Spence JD, Nygård O, Jamison R, Gaziano JM, Guarino P, Bennett D, Mir F, Peto R, Collins R (Oct 11, 2010). "Effects of lowering homocysteine levels with B vitamins on cardiovascular disease, cancer, and cause-specific mortality: Meta-analysis of 8 randomized trials involving 37 485 individuals". Archives of Internal Medicine 170 (18): 1622–31. doi:10.1001/archinternmed.2010.348. PMID 20937919.
- ↑ Bushnell C, McCullough LD, Awad IA, Chireau MV, Fedder WN, Furie KL, Howard VJ, Lichtman JH, Lisabeth LD, Piña IL, Reeves MJ, Rexrode KM, Saposnik G, Singh V, Towfighi A, Vaccarino V, Walters MR (2014). "Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association". Stroke; a Journal of Cerebral Circulation 45 (5): 1545–88. doi:10.1161/01.str.0000442009.06663.48. PMID 24503673.
- ↑ 106.0 106.1 Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA (May 1, 2014). "Guidelines for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association.". Stroke; a journal of cerebral circulation 45 (7): 2160–236. doi:10.1161/STR.0000000000000024. PMID 24788967.
- ↑ Hart RG, Pearce LA, Aguilar MI (2007). "Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation". Ann. Intern. Med. 146 (12): 857–67. doi:10.7326/0003-4819-146-12-200706190-00007. PMID 17577005.
- ↑ Paciaroni M, Agnelli G, Micheli S, Caso V (2007). "Efficacy and safety of anticoagulant treatment in acute cardioembolic stroke: a meta-analysis of randomized controlled trials". Stroke 38 (2): 423–30. doi:10.1161/01.STR.0000254600.92975.1f. PMID 17204681.ACP JC synopsis
- ↑ Armstrong MJ, Gronseth G, Anderson DC, Biller J, Cucchiara B, Dafer R, Goldstein LB, Schneck M, Messé SR (May 28, 2013). "Summary of evidence-based guideline: Periprocedural management of antithrombotic medications in patients with ischemic cerebrovascular disease: Report of the Guideline Development Subcommittee of the American Academy of Neurology". Neurology 80 (22): 2065–2069. doi:10.1212/WNL.0b013e318294b32d. PMC 3716407. PMID 23713086.
- ↑ Gomez CR: Time is Brain! J Stroke and Cerebrovasc Dis 3:1-2. 1993, additional Time
- ↑ Saver JL (2006). "Time is brain - quantified". Stroke 37 (1): 263–6. doi:10.1161/01.STR.0000196957.55928.ab. PMID 16339467.
- ↑ Bellolio MF, Gilmore RM, Stead LG (2011-09-07). Bellolio, M Fernanda, ed. "Insulin for glycaemic control in acute ischaemic stroke". Cochrane database of systematic reviews (Online) 9 (9): CD005346. doi:10.1002/14651858.CD005346.pub3. PMID 21901697.
- ↑ Bath, PM; Krishnan, K (28 October 2014). "Interventions for deliberately altering blood pressure in acute stroke.". The Cochrane database of systematic reviews 10: CD000039. doi:10.1002/14651858.CD000039.pub3. PMID 25353321.
- ↑ 114.0 114.1 Wardlaw, JM; Murray, V; Berge, E; del Zoppo, GJ (Jul 29, 2014). "Thrombolysis for acute ischaemic stroke.". The Cochrane database of systematic reviews 7: CD000213. doi:10.1002/14651858.CD000213.pub3. PMID 25072528.
- ↑ 115.0 115.1 Emberson, J; Lees, KR; Lyden, P; Blackwell, L; Albers, G; Bluhmki, E; Brott, T; Cohen, G; Davis, S; Donnan, G; Grotta, J; Howard, G; Kaste, M; Koga, M; von Kummer, R; Lansberg, M; Lindley, RI; Murray, G; Olivot, JM; Parsons, M; Tilley, B; Toni, D; Toyoda, K; Wahlgren, N; Wardlaw, J; Whiteley, W; Del Zoppo, GJ; Baigent, C; Sandercock, P; Hacke, W; for the Stroke Thrombolysis Trialists' Collaborative, Group (Aug 5, 2014). "Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials.". Lancet 384: 1929–1935. doi:10.1016/S0140-6736(14)60584-5. PMID 25106063.
- ↑ Wardlaw, JM; Murray, V; Berge, E; del Zoppo, GJ (Jul 29, 2014). "Thrombolysis for acute ischaemic stroke.". The Cochrane database of systematic reviews 7: CD000213. doi:10.1002/14651858.CD000213.pub3. PMID 25072528.
- ↑ 117.0 117.1 "Thrombolytics for acute stroke". Dynamed. Sep 15, 2014. Retrieved 4 October 2014.
at 3-4.5 hours after stroke onset t-PA increases risk of symptomatic intracranial hemorrhage but effect on functional outcomes is inconsistent
- ↑ "Thrombolysis in acute ischaemic stroke: time for a rethink?". BMJ 350 (h1075). Mar 17, 2015. doi:10.1136/bmj.h1075.
- ↑ "Canadian Association of Emergency Physicians Position Statement on Acute Ischemic Stroke" (PDF). caep.ca. 20155. Retrieved 7 April 2015. Check date values in:
|date=(help) - ↑ Wardlaw JM, Murray V, Berge E, del Zoppo G, Sandercock P, Lindley RL, Cohen G (May 23, 2012). "Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis". Lancet. Online first (9834): 2364–72. doi:10.1016/S0140-6736(12)60738-7. PMC 3386494. PMID 22632907.
- ↑ Whiteley WN, Slot KB, Fernandes P, Sandercock P, Wardlaw J (November 2012). "Risk factors for intracranial hemorrhage in acute ischemic stroke patients treated with recombinant tissue plasminogen activator: a systematic review and meta-analysis of 55 studies". Stroke; a journal of cerebral circulation 43 (11): 2904–9. doi:10.1161/STROKEAHA.112.665331. PMID 22996959.
- ↑ The National Institute Of Neurological Disorders And Stroke Rt-Pa Stroke Study Group, (1995). "Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group". New England Journal of Medicine 333 (24): 1581–7. doi:10.1056/NEJM199512143332401. PMID 7477192.
- ↑ Wardlaw JM, Murray V, Berge E, Del Zoppo GJ (2009-10-07). Wardlaw, Joanna M, ed. "Thrombolysis for acute ischaemic stroke". Cochrane database of systematic reviews (Online) (4): CD000213. doi:10.1002/14651858.CD000213.pub2. PMID 19821269.
- ↑ Dubinsky R, Lai SM (2006). "Mortality of stroke patients treated with thrombolysis: analysis of nationwide inpatient sample". Neurology 66 (11): 1742–1744. doi:10.1212/01.wnl.0000218306.35681.38. PMID 16769953.
- ↑ "Position Statement on the Use of Intravenous Thrombolytic Therapy in the Treatment of Stroke". American Academy of Emergency Medicine. Retrieved 2008-01-25.
- ↑ Lee M, Hong KS, Saver JL (May 2010). "Efficacy of intra-arterial fibrinolysis for acute ischemic stroke: meta-analysis of randomized controlled trials". Stroke 41 (5): 932–7. doi:10.1161/STROKEAHA.109.574335. PMID 20360549.
- ↑ Simard JM, Sahuquillo J, Sheth KN, Kahle KT, Walcott BP (April 2011). "Managing malignant cerebral infarction". Curr Treat Options Neurol 13 (2): 217–29. doi:10.1007/s11940-010-0110-9. PMC 3243953. PMID 21190097.
- ↑ "Organised inpatient (stroke unit) care for stroke". Cochrane Database of Systematic Reviews. Sep 11, 2013. doi:10.1002/14651858.CD000197.pub3.
- ↑ http://www.stroke.scot.nhs.uk/docs/UseOfAnkle-FootOrthosesFollowingStroke.pdf
- ↑ O'Sullivan 2007, pp. 471, 484, 737, 740
- ↑ Mackenzie C (April 2011). "Dysarthria in stroke: a narrative review of its description and the outcome of intervention". Int J Speech Lang Pathol 13 (2): 125–36. doi:10.3109/17549507.2011.524940. PMID 21480809.
- ↑ West C, Hesketh A, Vail A, Bowen A (2005). West, Carolyn, ed. "Interventions for apraxia of speech following stroke". Cochrane Database Syst Rev (4): CD004298. doi:10.1002/14651858.CD004298.pub2. PMID 16235357.
- ↑ Kelly H, Brady MC, Enderby P (2010). Brady, Marian C, ed. "Speech and language therapy for aphasia following stroke". Cochrane Database Syst Rev (5): CD000425. doi:10.1002/14651858.CD000425.pub2. PMID 20464716.
- ↑ 134.0 134.1 B. Lange, S. Flynn & A. Rizzo, B.; Flynn, S.; Rizzo, A. (2009). "Initial usability assessment of off-the-shelf video game consoles for clinical game-based motor rehabilitation". Physical Therapy Reviews 14 (5): 355–362. doi:10.1179/108331909X12488667117258.
- ↑ Fregni F, Pascual-Leone A (2007). "Technology Insight: noninvasive brain stimulation in neurology—perspectives on the therapeutic potential of rTMS and tDCS". Nature Clinical Practice Neurology 3 (7): 383–393. doi:10.1038/ncpneuro0530. PMID 17611487.
- ↑ Balasubramanian S, Klein J, Burdet E (2010). "Robot-assisted rehabilitation of hand function". Current Opinion in Neurology 23 (6): 661–70. doi:10.1097/WCO.0b013e32833e99a4. PMID 20852421.
- ↑ 137.0 137.1 137.2 Brazzelli M, Saunders DH, Greig CA, Mead GE (2011). "Physical fitness training for stroke patients". The Cochrane Database of Systematic Reviews (11): CD003316. doi:10.1002/14651858.CD003316.pub4. PMID 22071806.
- ↑ Institute for Quality and Efficiency in Health Care (IQWiG). "After a stroke: Does fitness training improve overall health and mobility?". Informed Health Online. Institute for Quality and Efficiency in Health Care (IQWiG). Retrieved 20 June 2013.
- ↑ 139.0 139.1 Coffey C. Edward, Cummings Jeffrey L, Starkstein Sergio, Robinson Robert (2000). Stroke - the American Psychiatric Press Textbook of Geriatric Neuropsychiatry (Second ed.). Washington DC: American Psychiatric Press. pp. 601–617.
- ↑ Stanford Hospital & Clinics. "Cardiovascular Diseases: Effects of Stroke". Retrieved 2005.
- ↑ editors, Tom A. Schweizer, R. Loch Macdonald, (2014). The behavioral consequences of stroke. New York, NY [u.a.]: Springer. pp. 119–133. ISBN 978-1-4614-7671-9.
- ↑ Mackenzie, Catherine (2011). "Dysarthria in stroke: A narrative review of its description and the outcome of intervention". International Journal of Speech-Language Pathology: 125–136.
- ↑ Ackley, Betty; Ladwig, Gail B.; Kelley, Helen (2010). Nursing diagnosis handbook: an evidence-based guide to planning care (9th ed.). Maryland Heights, MO.: Mosby.
- ↑ 144.0 144.1 Senelick Richard C., Rossi, Peter W., Dougherty, Karla (1994). Living with Stroke: A Guide for Families. Contemporary Books, Chicago. ISBN 0-8092-2607-3. OCLC 40856888 42835161.
- ↑ 145.0 145.1 Villarosa, Linda; Singleton, Lafayette; Johnson, Kirk A. (1993). The Black health library guide to stroke. New York: Henry Holt and Co. ISBN 0-8050-2289-9. OCLC 26929500.
- ↑ Hamilton RH, Chrysikou EG, Coslett B (July 2011). "Mechanisms of aphasia recovery after stroke and the role of noninvasive brain stimulation". Brain Lang 118 (1–2): 40–50. doi:10.1016/j.bandl.2011.02.005. PMC 3109088. PMID 21459427.
- ↑ Leys D, Hénon H, Mackowiak-Cordoliani MA, Pasquier F (November 2005). "Poststroke dementia". Lancet Neurol 4 (11): 752–9. doi:10.1016/S1474-4422(05)70221-0. PMID 16239182.
- ↑ Coulthard E, Singh-Curry V, Husain M (December 2006). "Treatment of attention deficits in neurological disorders". Current Opinion in Neurology 19 (6): 613–8. doi:10.1097/01.wco.0000247605.57567.9a. PMID 17102702.
- ↑ Lim C, Alexander MP (December 2009). "Stroke and episodic memory disorders". Neuropsychologia 47 (14): 3045–58. doi:10.1016/j.neuropsychologia.2009.08.002. PMID 19666037.
- ↑ Murray ED, Buttner N, Price BH (2012). "Depression and Psychosis in Neurological Practice". In Bradley WG, Daroff RB, Fenichel GM, Jankovic J. Bradley's neurology in clinical practice. 1 (6th ed.). Philadelphia, PA: Elsevier/Saunders. pp. 100–1. ISBN 1-4377-0434-4.
- ↑ Reith J, Jørgensen HS, Nakayama H, Raaschou HO, Olsen TS (August 1997). "Seizures in acute stroke: predictors and prognostic significance. The Copenhagen Stroke Study". Stroke 28 (8): 1585–9. doi:10.1161/01.STR.28.8.1585. PMID 9259753.
- ↑ Burn J, Dennis M, Bamford J, Sandercock P, Wade D, Warlow C (December 1997). "Epileptic seizures after a first stroke: the Oxfordshire Community Stroke Project". BMJ 315 (7122): 1582–7. doi:10.1136/bmj.315.7122.1582. PMC 2127973. PMID 9437276.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved November 11, 2009.
- ↑ "The top 10 causes of death". WHO.
- ↑ Towfighi A, Saver JL (August 2011). "Stroke declines from third to fourth leading cause of death in the United States: historical perspective and challenges ahead". Stroke 42 (8): 2351–5. doi:10.1161/STROKEAHA.111.621904. PMID 21778445.
- ↑ Ellekjaer H, Holmen J, Indredavik B, Terent A (November 1, 1997). "Epidemiology of Stroke in Innherred, Norway, 1994 to 1996 : Incidence and 30-Day Case-Fatality Rate". Stroke 28 (11): 2180–2184. doi:10.1161/01.STR.28.11.2180. PMID 9368561. Retrieved 2008-01-22.
- ↑ Bongers TN, de Maat MP, van Goor ML, Bhagwanbali V, van Vliet HH, Gómez García EB, Dippel DW, Leebeek FW (2006). "High von Willebrand factor levels increase the risk of first ischemic stroke: influence of ADAMTS13, inflammation, and genetic variability". Stroke 37 (11): 2672–7. doi:10.1161/01.STR.0000244767.39962.f7. PMID 16990571.
- ↑ Ashrafian H (2010). "Familial stroke 2700 years ago". Stroke 41 (4): e187. doi:10.1161/STROKEAHA.109.573170. PMID 20185778.
- ↑ 159.0 159.1 Thompson JE (August 1, 1996). "The evolution of surgery for the treatment and prevention of stroke. The Willis Lecture". Stroke 27 (8): 1427–34. doi:10.1161/01.STR.27.8.1427. PMID 8711815.
- ↑ Kopito, Jeff (September 2001). "A Stroke in Time". MERGINET.com 6 (9).
- ↑ R. Barnhart, ed. The Barnhart Concise Dictionary of Etymology (1995)
- ↑ Schiller F (April 1970). "Concepts of stroke before and after Virchow". Med Hist 14 (2): 115–31. doi:10.1017/S0025727300015325. PMC 1034034. PMID 4914683.
- ↑ Stanley Finger; François Boller; Kenneth L. Tyler (2010). Handbook of Clinical Neurology. North-Holland Publishing Company. p. 401. ISBN 978-0-444-52009-8. Retrieved 1 October 2013.
- ↑ John W. Scadding (December 2011). Clinical Neurology. CRC Press. p. 488. ISBN 978-0-340-99070-4. Retrieved 1 October 2013.
- ↑ Joseph I. Sirven; Barbara L. Malamut (2008). Clinical Neurology of the Older Adult. Lippincott Williams & Wilkins. p. 243. ISBN 978-0-7817-6947-1. Retrieved 1 October 2013.
- ↑ David Myland Kaufman; Mark J Milstein (5 December 2012). Kaufman's Clinical Neurology for Psychiatrists. Elsevier Health Sciences. p. 892. ISBN 978-1-4557-4004-8. Retrieved 1 October 2013.
- ↑ 167.0 167.1 Mosby's Medical Dictionary, 8th edition. Elsevier. 2009.
- ↑ "What is a Stroke/Brain Attack?" (PDF). National Stroke Association. Retrieved 27 February 2014.
- ↑ Segen's Medical Dictionary. Farlex, Inc. 2010.
- ↑ Derdeyn CP, Chimowitz MI; Chimowitz (August 2007). "Angioplasty and Stenting for Atherosclerotic Intracranial Stenosis: Rationale for a Randomized Clinical Trial". Neuroimaging Clin. N. Am. 17 (3): 355–63, viii–ix. doi:10.1016/j.nic.2007.05.001. PMC 2040119. PMID 17826637.
- ↑ Tenser MS, Amar AP, Mack WJ; Amar; Mack (December 2011). "Mechanical thrombectomy for acute ischemic stroke using the MERCI retriever and penumbra aspiration systems". World neurosurgery 76 (6 Suppl): S16–23. doi:10.1016/j.wneu.2011.07.003. PMID 22182267.
- ↑ Ortega-Lopez Y, Llanos-Mendez A (2010). "[Mechanical thrombectomy with MERCI device. Ischaemic stroke]". Andalusian Agency for Health Technology Assessment.
- ↑ Lees KR, Zivin JA, Ashwood T, Davalos A, Davis SM, Diener HC, Grotta J, Lyden P, Shuaib A, Hårdemark HG, Wasiewski WW; Zivin; Ashwood; Davalos; Davis; Diener; Grotta; Lyden; Shuaib; Hårdemark; Wasiewski; Stroke-Acute Ischemic NXY Treatment (SAINT I) Trial Investigators (February 2006). "NXY-059 for acute ischemic stroke". The New England Journal of Medicine 354 (6): 588–600. doi:10.1056/NEJMoa052980. PMID 16467546.
- ↑ Koziol JA, Feng AC; Feng (October 2006). "On the analysis and interpretation of outcome measures in stroke clinical trials: lessons from the SAINT I study of NXY-059 for acute ischemic stroke". Stroke; a journal of cerebral circulation 37 (10): 2644–7. doi:10.1161/01.STR.0000241106.81293.2b. PMID 16946150.
- ↑ Bennett, MH; Weibel, S; Wasiak, J; Schnabel, A; French, C; Kranke, P (12 November 2014). "Hyperbaric oxygen therapy for acute ischaemic stroke.". The Cochrane database of systematic reviews 11: CD004954. doi:10.1002/14651858.CD004954.pub3. PMID 25387992.
Further reading
- J. P. Mohr, Dennis Choi, James Grotta, Philip Wolf (2004). Stroke: Pathophysiology, Diagnosis, and Management. New York: Churchill Livingstone. ISBN 0-443-06600-0. OCLC 50477349 52990861.
- Charles P. Warlow, Jan van Gijn, Martin S. Dennis, Joanna M. Wardlaw, John M. Bamford, Graeme J. Hankey, Peter A. G. Sandercock, Gabriel Rinkel, Peter Langhorne, Cathie Sudlow, Peter Rothwell (2008). Stroke: Practical Management (3rd ed.). Wiley-Blackwell. ISBN 1-4051-2766-X.
External links
| Wikimedia Commons has media related to Stroke. |
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||