Shoulder
| Shoulder | |
|---|---|
|
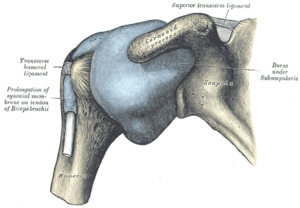
Diagram of the human shoulder joint | |
|
Capsule of shoulder-joint (distended). Anterior aspect. | |
| Details | |
| Latin | articulatio humeri |
| Identifiers | |
| Gray's | p.313 |
| MeSH | D012782 |
| Dorlands /Elsevier | 12161240 |
| Anatomical terminology | |
The human shoulder is made up of three bones: the clavicle (collarbone), the scapula (shoulder blade), and the humerus (upper arm bone) as well as associated muscles, ligaments and tendons. The articulations between the bones of the shoulder make up the shoulder joints. "Shoulder joint" typically refers to the glenohumeral joint, which is the major joint of the "shoulder," but can more broadly include the acromioclavicular joint. In human anatomy, the shoulder joint comprises the part of the body where the humerus attaches to the scapula, the head sitting in the glenoid cavity.[1] The shoulder is the group of structures in the region of the joint.[2]
There are two kinds of cartilage in the joint. The first type is the white cartilage on the ends of the bones (called articular cartilage) which allows the bones to glide and move on each other. When this type of cartilage starts to wear out (a process called arthritis), the joint becomes painful and stiff. The labrum is a second kind of cartilage in the shoulder which is distinctly different from the articular cartilage. This cartilage is more fibrous or rigid than the cartilage on the ends of the ball and socket. Also, this cartilage is also found only around the socket where it is attached.[3]
The shoulder must be mobile enough for the wide range actions of the arms and hands, but also stable enough to allow for actions such as lifting, pushing and pulling. The compromise between mobility and stability results in a large number of shoulder problems not faced by other joints such as the hip.
Structures
Bones
Bone is living tissue that makes up the body's skeleton providing shape and support. The bones that form the shoulder are the clavicle, humerus, and scapula, the latter providing the glenoid fossa, acromion and coracoid processes. These three bones create a ball-and-socket glenohumeral joint, that give the shoulder its wide range of motion in three different planes. In order for this joint to be operational, ligaments, muscles, and tendons must support the bone and maintain the relationship of one to another. Joints are formed by the ligamentous connection between two adjacent bones. Examples of both ligaments and joints are demonstrated by the glenohumeral, acromiclavicular, and sternoclavicular regions.
Joints
There are three joints of the shoulder: The glenohumeral, acromioclavicular, and the sternoclavicular joints.
Glenohumeral joint

The glenohumeral joint is the main joint of the shoulder and the generic term "shoulder joint" usually refers to it. It is a ball and socket joint that allows the arm to rotate in a circular fashion or to hinge out and up away from the body. It is formed by the articulation between the head of the humerus and the lateral scapula (specifically-the glenoid fossa of the scapula). The "ball" of the joint is the rounded, medial anterior surface of the humerus and the "socket" is formed by the glenoid fossa, the dish-shaped portion of the lateral scapula. The shallowness of the fossa and relatively loose connections between the shoulder and the rest of the body allows the arm to have tremendous mobility, at the expense of being much easier to dislocate than most other joints in the body. There is an approximately 4-to-1 disproportion in size between the large head of the humerus and the shallow glenoid cavity.
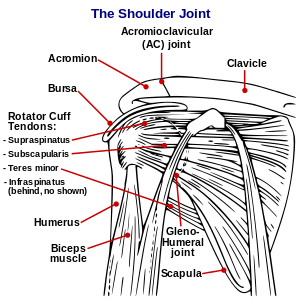
The capsule is a soft tissue envelope that encircles the glenohumeral joint and attaches to the scapula, humerus, and head of the biceps. It is lined by a thin, smooth synovial membrane. This capsule is strengthened by the coracohumeral ligament which attaches the coracoid process of the scapula to the greater tubercle of the humerus. There are also three other ligaments attaching the lesser tubercle of the humerus to lateral scapula and are collectively called the glenohumeral ligaments.
The transverse humeral ligament, which passes from the lesser tubercle to the greater tubercle of humerus, covers the intertubercular groove, in which the long head of biceps brachii travels.
Sternoclavicular joint
The sternoclavicular occurs at the medial end of the clavicle with the manubrium or top most portion of the sternum. The clavicle is triangular and rounded and the manubrium is convex; the two bones articulate. The joint consists of a tight capsule and complete intra-articular disc which ensures stability of the joint. The costoclavicular ligament is the main limitation to movement, therefore, the main stabilizer of the joint. A fibrocartilaginous disc present at the joint increases the range of movement. Sternoclavicular dislocation is rare,[4] but may result from direct trauma to the clavicle or indirect forces applied to the shoulder.[5] Posterior dislocations deserve special attention, as they have the potential to be life-threatening because of the risk of damage to vital structures in the mediastinum.[6]
Muscles
Major muscles
The muscles that are responsible for movement in the shoulder attach to the scapula, humerus, and clavicle. The muscles that surround the shoulder form the shoulder cap and underarm.
| Name | Attachment | Function |
| serratus anterior | Originates on the surface of the upper eight ribs at the side of the chest and inserts along the entire anterior length of the medial border of the scapula. | It fixes the scapula into the thoracic wall and aids in rotation and abduction of the shoulders. |
| subclavius | Located inferior to the clavicle, originating on the first rib and inserting (penetrating) on the subclavian groove of the clavicle. | It depresses the lateral clavicle and also acts to stabilize the clavicle. |
| pectoralis minor | Arises from the third, fourth, and fifth ribs, near their cartilage and inserts into the medial border and upper surface of the coracoid process of the scapula. | This muscle aids in respiration, medially rotates the scapula, protracts the scapula, and also draws the scapula inferiorly. |
| sternocleidomastoid | Attaches to the sternum (sterno-), the clavicle (cleido-), and the mastoid process of the temporal bone of the skull. | Most of its actions flex and rotate the head. In regards to the shoulder, however, it also aids in respiration by elevating the sternoclavicular joint when the head is fixed. |
| levator scapulae | Arises from the transverse processes of the first four cervical vertebrae and inserts into the medial border of the scapula. | It is capable of rotating the scapula downward and elevating the scapula. |
| rhomboid major and rhomboid minor (work together) | They arise from the spinous processes of the thoracic vertebrae T1 to T5 as well as from the spinous processes of the seventh cervical. They insert on the medial border of the scapula, from about the level of the scapular spine to the scapula's inferior angle. | They are responsible for downward rotation of the scapula with the levator scapulae, as well as adduction of the scapula. |
| trapezius | Arises from the occipital bone, the ligamentum nuchae, the spinous process of the seventh cervical, and the spinous processes of all the thoracic vertebrae, and from the corresponding portion of the supraspinal ligament. It inserts on the lateral clavicle, the acromion process, and into the spine of the scapula. | Different portions of the fibers perform different actions on the scapula: depression, upward rotation, elevation, and adductions. |
| deltoid, anterior fibers | Arises from the anterior border and upper surface of the lateral third of the clavicle. | The anterior fibres are involved in shoulder abduction when the shoulder is externally rotated. The anterior deltoid is weak in strict transverse flexion but assists the pectoralis major during shoulder transverse flexion / shoulder flexion (elbow slightly inferior to shoulders). |
| deltoid, middle fibers | Arises from the lateral margin and upper surface of the acromion. | The middle fibres are involved in shoulder abduction when the shoulder is internally rotated, are involved in shoulder flexion when the shoulder is internally rotated, and are involved in shoulder transverse abduction (shoulder externally rotated) -- but are not utilized significantly during strict transverse extension (shoulder internally rotated). |
| deltoid, posterior fibers | Arises from the lower lip of the posterior border of the spine of the scapula, as far back as the triangular surface at its medial end. | The posterior fibres are strongly involved in transverse extension particularly since the latissimus dorsi muscle is very weak in strict transverse extension. The posterior deltoid is also the primary shoulder hyperextensor. |
Rotator Cuff
The muscles of the rotator cuff are supraspinatus, subscapularis, infraspinatus, and teres minor, all contributing to the stability of the shoulder. The cuff adheres to the glenohumeral capsule and attaches to the humeral head. The upper edge of the subscapularis tendon and anterior edge of the supraspinatus muscle, delineate a triangular space at the humeral head called the rotator interval.[7] The cuff plays two main roles:
- stabilizes the glenohumeral joint;
- rotates the humerus outward (external rotation).
The cuff centers the humeral head in the glenoid cavity and prevents upward migration of the humeral head caused by the pull of the deltoid muscle at the beginning of arm elevation. Furthermore, the infraspinatus and the teres minor, along with the anterior fibers of the deltoid muscle, are responsible for external rotation of the arm.[7]
The four tendons of these muscles converge to form the rotator cuff tendon. These tendinous insertions along with the articular capsule, the coracohumeral ligament, and the glenohumeral ligament complex, blend into a confluent sheet before insertion into the humeral tuberosities.[8] The insertion site of the rotator cuff tendon at the greater tuberosity is often referred to as the footprint. The infraspinatus and teres minor fuse near their musculotendinous junctions, while the supraspinatus and subscapularis tendons join as a sheath that surrounds the biceps tendon at the entrance of the bicipital groove.[8] The supraspinatus is most commonly involved in a rotator cuff tear.
The insertions sites of the supraspinatus and infraspinatus tendons have been further described as a five-layer structure[8] providing a glimpse into the various types of tears that can form given the different fiber characteristics of each layer.
Function
Movements
The muscles and joints of the shoulder allow it to move through a remarkable range of motion, making it one of the most mobile joints in the human body. The shoulder can abduct, adduct, rotate, be raised in front of and behind the torso and move through a full 360° in the sagittal plane. This tremendous range of motion also makes the shoulder extremely unstable, far more prone to dislocation and injury than other joints [9]
The following describes the terms used for different movements of the shoulder:[10]
| Name | Description | Muscles |
|---|---|---|
| Scapular retraction [11] (aka scapular adduction) | The scapula is moved posteriorly and medially along the back, moving the arm and shoulder joint posteriorly. Retracting both scapulae gives a sensation of "squeezing the shoulder blades together." | rhomboideus major, minor, and trapezius |
| Scapular protraction[11] (aka scapular abduction) | The opposite motion of scapular retraction. The scapula is moved anteriorly and laterally along the back, moving the arm and shoulder joint anteriorly. If both scapulae are protracted, the scapulae are separated and the pectoralis major muscles are squeezed together. | serratus anterior (prime mover), pectoralis minor and major |
| Scapular elevation [12] | The scapula is raised in a shrugging motion. | levator scapulae, the upper fibers of the trapezius |
| Scapular depression [12] | The scapula is lowered from elevation. The scapulae may be depressed so that the angle formed by the neck and shoulders is obtuse, giving the appearance of "slumped" shoulders. | pectoralis minor, lower fibers of the trapezius, subclavius, latissimus dorsi |
| Arm abduction [13] | Arm abduction occurs when the arms are held at the sides, parallel to the length of the torso, and are then raised in the plane of the torso. This movement may be broken down into two parts: True abduction of the arm, which takes the humerus from parallel to the spine to perpendicular; and upward rotation of the scapula, which raises the humerus above the shoulders until it points straight upwards. | True abduction: supraspinatus (first 15 degrees), deltoid; Upward rotation: trapezius, serratus anterior |
| Arm adduction [14] | Arm adduction is the opposite motion of arm abduction. It can be broken down into two parts: downward rotation of the scapula and true adduction of the arm. | Downward rotation: pectoralis minor, pectoralis major, subclavius, latissimus dorsi (same as scapular depression, with pec major replacing lower fibers of trapezius); True Adduction: same as downward rotation with addition of teres major and the lowest fibers of the deltoid |
| Arm flexion [15] | The humerus is rotated out of the plane of the torso so that it points forward (anteriorly). | pectoralis major, coracobrachialis, biceps brachii, anterior fibers of deltoid. |
| Arm extension [15] | The humerus is rotated out of the plane of the torso so that it points backwards (posteriorly) | latissimus dorsi and teres major, long head of triceps, posterior fibers of the deltoid |
| Medial rotation of the arm [16] | Medial rotation of the arm is most easily observed when the elbow is held at a 90-degree angle and the fingers are extended so they are parallel to the ground. Medial rotation occurs when the arm is rotated at the shoulder so that the fingers change from pointing straight forward to pointing across the body. | subscapularis, latissimus dorsi, teres major, pectoralis major, anterior fibers of deltoid |
| Lateral rotation of the arm[16] | The opposite of medial rotation of the arm. | infraspinatus and teres minor, posterior fibers of deltoid |
| Arm circumduction[17] | Movement of the shoulder in a circular motion so that if the elbow and fingers are fully extended the subject draws a circle in the air lateral to the body. In circumduction, the arm is not lifted above parallel to the ground so that "circle" that is drawn is flattened on top. | pectoralis major, subscapularis, coracobrachialis, biceps brachii, supraspinatus, deltoid, latissimus dorsi, teres major and minor, infraspinatus, long head of triceps |
Rotator cuff
The rotator cuff is an anatomical term given to the group of muscles and their tendons that act to stabilize the shoulder. It is composed of the tendons and muscles (supraspinatus, infraspinatus, teres minor and subscapularis) that hold the head of the humerus (ball) in the glenoid fossa (socket).
Two filmy sac-like structures called bursae permit smooth gliding between bone, muscle, and tendon. They cushion and protect the rotator cuff from the bony arch of the acromion.
Clinical significance
Shoulder problems including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well. Major injuries to the shoulder include rotator cuff tear and bone fractures of one or more of the bones of the shoulder.
Fracture
Shoulder fractures include:
Shoulder imaging
There are several ways to depict the structures of the shoulder, which consist of muscles, tendons, bones, cartilage and soft tissue. When deciding which medical imaging technique should be used, there are a couple of factors that need to be taken into account. Firstly, one has to consider the suspected clinical diagnosis. Together with the knowledge of the advantages and limitations of the various medical imaging techniques ( i.e. conventional radiography, ultrasound, computer tomography and magnetic resonance), one has to make an informed decision which technique would best suit the specific situation.
Hodler et al. recommend to start scanning with conventional x-rays taken from at least two planes, since this method gives a wide first impression and even has the chance of exposing any frequent shoulder pathologies, i.e. decompensated rotator cuff tears, tendinitis calcarea, dislocations, fractures, usures and/or osteophytes. Furthermore, x-rays are required for the planning of an optimal CT or MR image.[18]
Conventional x-rays and ultrasonography are the primary tools used to confirm a diagnosis of injuries sustained to the rotator cuff. For extended clinical questions, imaging through Magnetic Resonance with or without intraarticular contrast agent is indicated.
The conventional invasive arthrography is now-a-days being replaced by the non-invasive MRI and US and is used as an imaging reserve for patients who are contraindicated for MRI, for example pacemaker-carriers with an unclear and unsure ultrasonography.[19]
Conventional x-rays
a.-p.-projection 40° posterior oblique after Grashey

The body has to be rotated about 30 to 45 degrees towards the shoulder to be imaged, and the standing or sitting patient lets the arm hang.
This method allows the diagnostician to judge:[19]
- The joint gap and the vertical alignment towards the socket.
The humerus head should be aligned in the neutral position and external rotation in a way towards the socket, that a fictive continuous line can be seen. This line is called Bandi line, otherwise known as the Ménard-Shenton line. A discontinuous line alludes to a cranial decentralization of the humerus head.[20]
Transaxillary projection


The arm should be abducted 80 to 100 degrees at a precise defined scapular or frontal plane.
This method allows the diagnostician to judge:[19]
- The horizontal alignment of the humerus head in respect to the socket, and the lateral clavicle in respect to the acromion.
- Lesions of the anterior and posterior socket border or of the tuberculum minus.
- The eventual non-closure of the acromial apophysis.
- The coraco-humeral interval
Y-projection

The lateral contour of the shoulder should be positioned in front of the film in a way that the longitudinal axis of the scapula continues parallel to the path of the rays.
This method allows the diagnostician to judge:[19]
- The horizontal centralization of the humerus head and socket.
- The osseous margins of the coraco-acromial arch and hence the supraspinatus outlet canal.
- The shape of the acromion
This Y-projection can be traced back to Wijnblath’s 1933 published cavitas-en-face projection.[21]
It must be pointed out that this projection has a low tolerance for errors and accordingly needs proper execution.[19]
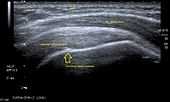
Ultrasound
There are several solid advantages of ultrasound. It is relatively cheap, does not emit any radiation, is accessible, is capable of visualizing tissue function in real time and allows to the performing of provocative maneuvers in order to replicate the patient’s pain.[22] Those apparent benefits have helped ultrasound become a common initial choice for assessing tendons and soft tissues. Limitations include, for example, the high degree of operator dependence and the inability to define pathologies in bones. One also has to have an extensive anatomical knowledge of the examined region and keep an open mind to normal variations and artifacts created during the scan.[23]
Although musculoskeletal ultrasound training, like medical training in general, is a lifelong process, Kissin et al. suggest that rheumatologists who taught themselves how to manipulate ultrasound can use it just as well as international musculo-skeletal ultrasound experts to diagnose common rheumatic conditions.[24]
After the introduction of high-frequency transducers in the mid-eighties, ultrasound has become a conventional tool for taking accurate and precise images of the shoulder to support diagnosis.[25][26][27][28][29]
Adequate for the examination are high-resolution, high-frequency transducers with a transmission frequency of 5, 7.5 and 10 MHz. To improve the focus on structures close to the skin an additional „water start-up length“ is advisable. During the examination the patient is asked to be seated, the affected arm is then adducted and the elbow is bent to 90 degrees. Slow and cautious passive lateral and/or medial rotations have the effect of being able to visualize different sections of the shoulder. In order to also demonstrate those parts which are hidden under the acromion in the neutral position, a maximum medial rotation with hyperextension behind the back is required.[30]
To avoid the different tendon echogenicities caused by different instrument settings, Middleton compared the tendon’s echogenicity with that of the deltoid muscle, which is still lege artis.[31][32]
Usually the echogenicity compared to the deltoid muscle is homogeneous intensified without dorsal echo extinction. Variability with reduced or intensified[33] echo has also been found in healthy tendons. Bilateral comparison is very helpful when distinguishing and setting boundaries between physiological variants and a possible pathological finding. Degenerative changes at the rotator cuff often are found on both sides of the body.[34] Consequently unilateral differences rather point to a pathological source and bilateral changes rather to a physiological variation.[32]
In addition, a dynamic examination can help to differentiate between an ultrasound artifact and a real pathology.[35]
To accurately evaluate the echogenicity of an ultrasound, one has to take into account the physical laws of reflection, absorption and dispersion. It is at all times important to acknowledge that the structures in the joint of the shoulder are not aligned in the transversal, coronal or sagittal plane, and that therefore during imaging of the shoulder the transducer head has to be hold perpendicularly or parallel to the structures of interest. Otherwise the appearing echogenicity may not be evaluated.[36]
Orientation-aid for the longitudinal plane:
As an aid to orientation, it is advisable to begin the examination with the delineation of the acromion, as it is easy to palpate and it has an identifiable echo extinction. To adjust the longitudinal plane image the way it is known in the x-rays and the physical examination, the acromion has to be visible at the image border.[36]
Orientation-aid for the transversal plane:
Again it is advantageous to start above the acromion and then move the transducer to the humerus. The acromion echo extinction disappears and the wheel-like figure with almost concentric projection of the deltoid muscle, supraspinatus muscle tendon and humeral head-outline turns up as soon as the transducer is directed perpendicularly and parallel to the acromion edge. Using the anterior transversal plane one can depict the intraarticular part of the long head of the biceps brachii muscle. Additionally one can use the posterior transversal plane to depict the intersection of the infraspinatus muscle tendon and the posterior edge of the fossa.[36]
| usual longitudinal front vision | usual longitudinal back vision | usual transversal side vision | |
|---|---|---|---|
| supraspinatus tendon | acromion of the left shoulder in the left half of the image and vice versa. (In order to explore the entire tendon the examiner must move the transducer from ventral to dorsal perpendicular at the acromion axis. Either through a maximal medial rotation or an according position of the transducer it is possible to see the supra- infraspinatus tendon intersection.) | ventral right shoulder in the right half of the image and vice versa. | |
| infraspinatus tendon | scapula spine of the right shoulder in the left half of the image and vice versa. |
 Longitudinal ultra sonography of the supraspinatus tendon |
 Transversal ultra sonography of the supraspinatus tendon |
MRI
Orthopedics established early the MRI as the tool of choice for joint- and soft tissue-imaging, because its non-invasiveness, the lack of radiation exposure, multi planar slicing possibilities and the high soft tissue contrast.[37]
The MR Imaging should provide joint details to the treating orthopedist, to help him diagnose and decide the next appropriate therapeutic step.
To examine the shoulder, the patient is lying and the concerned arm is in lateral rotation. For signal detection it is recommended to use a surface-coil. To find pathologies of the rotator cuff in the basic diagnostic investigation, T2-weighted sequences with fat-suppression or STIR sequences have proven value. In general, the examination should occur in the following three main planes: axial, oblique coronal and sagittal.[38]
Most morphological changes and injuries are sustained to the supraspinatus tendon. Traumatic rotator cuff changes are often located antero-superior, meanwhile degenerative changes more likely are supero-posterior.[39]
Tendons are predominantly composed of dense collagen fiber bundles. Because of their extreme short T2-relaxation time they appear typically signal-weak, respectively, dark. Degenerative changes, inflammations and also partial and complete tears cause loss of the original tendon structure. Fatty deposits, mucous degeneration and hemorrhages lead to an increased intratendinal T1-image. Edema formations, inflammatory changes and ruptures increase the signals in a T2-weighted image.[38]
Magic angle artifact

Erickson et al. noticed and described a typical artifact and gave the phenomenon the name „magic angle“. The „magic angle“ describes a changed T2-relaxation time depending on the spatial orientation of the tissue to the main magnetic field. If parts of the tendon are located at the area of the magic angle at 55 degrees to the main magnetic field, their T2-relaxation time gets influenced and the signal heavily intensified. Unluckily these artifacts occupy similar areas where clinical relevant pathologies are found. To avoid a wrong diagnosis it is recommended to exclude this phenomenon in a case of doubt through a heavy T2-weighted sequence or an additional fat-suppression at a proton weighted sequence.[40]
MRA
While using MRI, true lesions at the rotator interval region between the parts of the supraspinatus and subscapularis are all but impossible to distinguish from normal synovium and capsule.[41]
In 1999, Weishaupt D. et al. reached through two readers a significant better visibility of pully lesions at the rotator interval and the expected location of the reflection pulley of the long biceps and subscapularis tendon on parasagittal (reader1/reader2 sensitivity: 86%/100%; specificity: 90%/70%) and axial (reader1/reader2 sensitivity: 86%/93%; specificity: 90%/80%) MRA images.[42]
When examining the rotator cuff, the MRA has a couple of advantages compared to the native MRI. Through a fat suppressed T2-weighted spin echo, MRA can reproduce an extreme high fat-water-contrast, which helps to detect water-deposits with better damage diagnosis in structurally changed collagen fiber bundles.[43]
In other animals
Tetrapod forelimbs are characterised by a high degree of mobility in the shoulder-thorax connection. Lacking a solid skeletal connection between the shoulder girdle and the vertebral column, the forelimb's attachment to the trunk is instead mainly controlled by serratus lateralis and levator scapulae. Depending on locomotor style, a bone connects the shoulder girdle to the trunk in some animals; the coracoid bone in reptiles and birds, and the clavicle in primates and bats; but cursorial mammals lack this bone. In primates, the shoulder shows characteristics that differ from other mammals, including a well developed clavicle, a dorsally shifted scapula with prominent acromion and spine, and a humerus featuring a straight shaft and a spherical head. [44]
Additional images
-
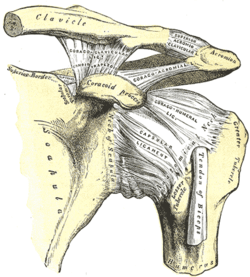
The left shoulder and acromioclavicular joints, and the proper ligaments of the scapula
-

Instrumented shoulder endoprosthesis, with a 9-channel telemetry transmitter to measure six load components in vivo
See also
- This article uses anatomical terminology; for an overview, see anatomical terminology.
- Shoulder girdle (Pectoral girdle)
- Glenohumeral joint (Shoulder joint)
- Acromioclavicular joint
- Sternoclavicular joint
- Chip on shoulder
References
- ↑ ‹The template EMedicineDictionary is being considered for deletion.› Shoulder+joint at eMedicine Dictionary
- ↑ ‹The template EMedicineDictionary is being considered for deletion.› Shoulder at eMedicine Dictionary
- ↑ "labrum tear Johns Hopkins Orthopaedic Surgery". www.hopkinsortho.org. Retrieved 2010-05-16.
- ↑ Cadogan, Mike (February 2010). "Sternoclavicular Joint Dislocations". Life in the Fast Lane. Retrieved June 2011.
- ↑ Arend CF. Ultrasound of the Shoulder. Master Medical Books, 2013. Free section on sternoclavicular joint dislocation available at ShoulderUS.com
- ↑ Jougon JB, Lepront DJ, Dromer CE. Posterior dislocation of the sternoclavicular joint. Ann Thorac Surg 1996; 61:711-13.
- ↑ 7.0 7.1 Favard L, Bacle G, Berhouet J (December 2007). "Rotator cuff repair". Joint Bone Spine 74 (6): 551–7. doi:10.1016/j.jbspin.2007.08.003. PMID 17993287.
- ↑ 8.0 8.1 8.2 Matava, M. J., Purcell, D. B., & Rudzki, J. R. (2005). Partial-Thickness Rotator Cuff Tears. Am J Sports Med 33: 1405. doi:10.1177/0363546505280213
- ↑ Scientific Keys Volume I, The Key Muscles of Hatha Yoga, Ray Long MD FRCSC, Third Edition, pg. 174
- ↑ "Movements of the Upper Limb — Introduction". University of Michigan Medical School. 2002. Retrieved December 2010.
- ↑ 11.0 11.1 "Scapular Protraction and Retraction". University of Michigan Medical School. 2002. Retrieved December 2010.
- ↑ 12.0 12.1 "Scapular Elevation and Depression". University of Michigan Medical School. 2002. Retrieved December 2010.
- ↑ "Arm Abduction". University of Michigan Medical School. 2002. Retrieved December 2010.
- ↑ "Arm Adduction". University of Michigan Medical School. 2002. Retrieved December 2010.
- ↑ 15.0 15.1 "Arm Flexion and Extension". University of Michigan Medical School. 2002. Retrieved December 2010.
- ↑ 16.0 16.1 "Arm Medial and Lateral Rotation". University of Michigan Medical School. 2002. Retrieved December 2010.
- ↑ "Arm Circumduction". University of Michigan Medical School. 2002. Retrieved December 2010.
- ↑ Hodler J et al.. Gelenkdiagnostik mit bildgebenden Verfahren. Stuttgart [etc.]. G. Thieme. 1992. ISBN 3-13-780501-5
- ↑ 19.0 19.1 19.2 19.3 19.4 Hedtmann A et al.. Imaging in evaluating rotator cuff tears. Orthopade. 2007 Sep;36(9):796-809. - (http://www.springerlink.com/content/26l346817932h383/)
- ↑ Bandi W (1981) Die Läsion der Rotatorenmanschette. Helv Chir Acta 48:537-549
- ↑ Wijnbladh H (1933) Zur Röntgendiagnose von Schulterluxationen. Chirurg 5:702
- ↑ Arend CF. Ultrasound of the Shoulder. Porto Alegre: Master Medical Books; 2013. Free access to sample chapter on ultrasound technique to evaluate rotator cuff disorders at ShoulderUS.com.
- ↑ Broadhurst NA. Musculoskeletal ultrasound - used to best advantage. Aust Fam Physician. 2007 Jun;36(6):430-2. - free article(http://www.racgp.org.au/afp/200706/200706broadhurst.pdf)
- ↑ Kissin et al.. Self-directed learning of basic musculo-skeletal ultrasound among rheumatologists in the United States. Arthritis Care Res (Hoboken). 2010 Feb;62(2):155-60 - (http://www3.interscience.wiley.com/journal/123236784/abstract)
- ↑ Allen GM, Wilson DJ, Eur J Ultrasound. 2001 Oct;14(1):3-9. Review - (http://linkinghub.elsevier.com/retrieve/pii/S0929826601001409)
- ↑ Middleton WD, Edelstein G, et al. Sonographic detection of rotator cuff tears. Ajr American Journal of Roentgenology. 1985a;144(2):349–53. free article(http://www.ajronline.org/cgi/reprint/144/2/349)
- ↑ Middleton WD, Reinus WR, et al. Ultrasonographic evaluation of the rotator cuff and biceps tendon. Journal of Bone and Joint Surgery American Volume. 1986;68(3):440–50.
- ↑ Crass JR, Craig EV, et al. Ultrasonography of rotator cuff tears: a review of 500 diagnostic studies. Jcu J Clin Ultrasound. 1988;16(5):313–27.
- ↑ Mack LA, Gannon MK, et al. Sonographic evaluation of the rotator cuff. Accuracy in patients without prior surgery. Clinical Orthopaedics and Related Research. 1988a;234:21–7.
- ↑ Thelen M. et al.. Radiologische Diagnostik der Verletzungen von Knochen und Gelenken. Stuttgart [etc.]. Georg Thieme. 1993. ISBN 3-13-778701-7
- ↑ Middleton WD. et al.. Ultrasonography of the rotator cuff: technique and normal anatomy. J Ultrasound Med.. 1984 Dec;3(12):549-51
- ↑ 32.0 32.1 Middleton WD, Reinus WR, Melson GL, Totty WG, Murphy WA (March 1986). "Pitfalls of rotator cuff sonography". AJR. American Journal of Roentgenology 146 (3): 555–60. doi:10.2214/ajr.146.3.555. PMID 3511639.
- ↑ crass 1984 @Katthagen BD. et al.. Schultersonographie. Stuttgart. ISBN 3-13-719401-6
- ↑ Arend CF (November 2013). "Top ten pitfalls to avoid when performing musculoskeletal sonography: what you should know before entering the examination room". European Journal of Radiology 82 (11): 1933–9. doi:10.1016/j.ejrad.2013.01.022. PMID 23478008.
- ↑ Hedtmann A. et al.. Atlas und Lehrbuch der Schultersonographie. Stuttgart. 1988@ Hodler J et al.. Gelenkdiagnostik mit bildgebenden Verfahren. Stuttgart [etc.]. G. Thieme. 1992. ISBN 3-13-780501-5
- ↑ 36.0 36.1 36.2 Katthagen BD. et al.. Schultersonographie. Stuttgart. ISBN 3-13-719401-6
- ↑ Trattnig S. et al.. High-field and ultrahigh-field magnetic resonance imaging: new possibilities for imaging joints. Z Rheumatol. 2006 Dec;65(8):681-7 - (http://www.springerlink.com/content/54r55191m43327j5/)
- ↑ 38.0 38.1 Romaneehsen B. et al.. MR imaging of tendon diseases. Exemplified using the examples of rotator cuff, epicondylitis and achillodynia. Orthopade. 2005 Jun;34(6):543-9 - (http://www.springerlink.com/content/r60654q134376711/)
- ↑ Nové-Josserand L, Gerber C, Walch G (1997) Lesions of the antero-superior rotator cuff. Lippincott-Raven, Philadelphia
- ↑ Erickson SJ, Cox IH, Hyde JS, Car re ra GF, Strandt JA, Estkowski LD (1991) Effect of tendon orientation on MR imaging signal intensity: a manifestation of the „magic angle" phenomenon. Radiology 181:389–393
- ↑ Seeger LL, Lubowitz J, Thomas BJ (1993) Case report 815: Tear of the rotator interval. Skeletal Radiol 22(8): 615–617
- ↑ Weishaupt D, Zanetti M, Tanner A et al. (1999) Lesions of the reflection pulley of the long biceps tendon. MR arthrographic findings. Invest Radiol 34: 463–469 @Hedtmann A. et al.. Imaging in evaluating rotator cuff tears. Orthopade. 2007 Sep;36(9):796-809 - (http://www.springerlink.com/content/26l346817932h383/)
- ↑ Palmer WE, Brown JH, Rosenthal DI (1993) Rotator cuff: evaluation with fat-suppressed MR arthrography. Radiology 188:683–687
- ↑ Preuschoft, Holger; Hohn, Bianca; Scherf, Heike; Schmidt, Manuela; Krause, Cornelia; Witzel, Ulrich (April 2010). "Functional Analysis of the Primate Shoulder". Int J Primatol. 31 (2): 301–320. doi:10.1007/s10764-010-9399-1. PMC 215885. PMID 2860095.
External links
| Wikimedia Commons has media related to Shoulders. |
| Look up shoulder in Wiktionary, the free dictionary. |
- Video of the shoulder carriage in motion
- NIH (article includes text from this source)
- University of Michigan Medical School module on movements of the shoulder, arm, forearm, and hand
| ||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||