Salmonellosis
| Salmonellosis | |
|---|---|
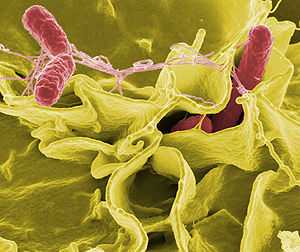 Electron micrograph showing Salmonella typhimurium (red) invading cultured human cells | |
| Classification and external resources | |
| ICD-10 | A02.0 |
| ICD-9 | 003.0 |
| MedlinePlus | 000294 |
Salmonellosis is an infection caused by Salmonella bacteria. Most people infected with Salmonella develop diarrhea, fever, vomiting, and abdominal cramps 12 to 72 hours after infection. In most cases, the illness lasts four to seven days, and most people recover without treatment.[1] In some cases, the diarrhea may be so severe that the patient becomes dangerously dehydrated and must be hospitalized.
Intravenous fluids may be used to treat dehydration. Medications may be used to provide symptomatic relief, such as fever reduction. In severe cases, the Salmonella infection may spread from the intestines to the blood stream, and then to other body sites; this is known as typhoid fever and is treated with antibiotics.
The elderly, infants, and those with impaired immune systems are more likely to develop severe illness. Some people afflicted with salmonellosis later experience reactive arthritis, which can have long-lasting, disabling effects. There are just two species of Salmonella, Salmonella bongori and Salmonella enterica. The latter is divided in 6 subspecies: enterica, salamae, arizonae, diazonae, houtenase and indica. These subspecies are further divided into numerous serovars. Because the serovars only differ in serotypes, and therefore in infection potential, the serovars are not italicised and are written with a capital letter as they still belong to the same subspecies.
The species Salmonella enterica subsp. enterica contains over 60% of the total number of serovars and 99% of the serovars that are capable of infecting cold and warm blooded animals as well as humans. Infections are usually contracted from sources such as:
- Poultry, pork, beef and fish (seafood), if the meat is prepared incorrectly or is infected with the bacteria after preparation[2]
- Infected eggs, egg products, and milk when not prepared, handled, or refrigerated properly[2]
- Tainted fruits and vegetables[2]
Reptiles such as red-eared slider turtles and green iguanas may carry Salmonella bongori (which inhabits cold-blooded animals) in their intestines which can cause intestinal infections. The most severe human Salmonella infection is caused by S. enterica subsp. enterica ser. Typhi which leads to typhoid fever; an infection that often proves fatal if not treated with the appropriate antibiotics. This serovar is restricted to humans and is usually contracted through direct contact with the fecal matter of an infected person. Typhoid fever is endemic in the developing world, where unsanitary conditions are more likely to prevail, and which can affect as many as 21.5 million people each year. Recorded cases of typhoid fever in the developed world are mostly related to recent travel in areas where Salmonella Typhi is endemic.
Signs and symptoms
Enteritis
After a short incubation period of a few hours to one day, the bacteria multiply in the intestinal lumen, causing an intestinal inflammation. Most people with salmonellosis develop diarrhea, fever, vomiting, and abdominal cramps 12 to 72 hours after infection.[3] Diarrhea is often mucopurulent (containing mucus or pus) and bloody. In most cases, the illness lasts four to seven days, and most people recover without treatment. In some cases, though, the diarrhea may be so severe that the patient becomes dangerously dehydrated and must be taken to a hospital. At the hospital, the patient may receive intravenous fluids to treat the dehydration, and may be given medications to provide symptomatic relief, such as fever reduction. In severe cases, the Salmonella infection may spread from the intestines to the blood stream, and then to other body sites, and can cause death, unless the person is treated promptly with antibiotics.
In otherwise healthy adults, the symptoms can be mild. Normally, no sepsis occurs, but it can occur exceptionally as a complication in the immunocompromised. However, in people at risk such as infants, small children, the elderly, Salmonella infections can become very serious, leading to complications. In infants, dehydration can cause a state of severe toxicity. Extraintestinal localizations are possible, especially Salmonella meningitis in children, osteitis, etc. Children with sickle cell anemia who are infected with Salmonella may develop osteomyelitis. Treatment of osteomyelitis, in this case, will be to use fluoroquinolones (ciprofloxacin, levofloxacin, etc. and nalidixic acid).
Those whose only symptom is diarrhea usually completely recover, but it can be several months until their bowel habits are normal.[4] A small number of people afflicted with salmonellosis experience reactive arthritis, which can last months or years and can lead to chronic arthritis.[5][6] In sickle-cell anemia, osteomyelitis due to Salmonella infection is much more common than in the general population. Though Salmonella infection is frequently the cause of osteomyelitis in sickle-cell anemia patients, it is not the most common cause; the most common cause remains Staphylococcus infection.
Typhoid fever
Typhoid fever occurs when Salmonella bacteria enter the lymphatic system and cause a systemic form of salmonellosis. Endotoxins first act on the vascular and nervous apparatus, resulting in increased permeability and decreased tone of the vessels, upset thermal regulation, vomiting and diarrhea. In severe forms of the disease, enough liquid and electrolytes are lost to upset the water-salt metabolism, decrease the circulating blood volume and arterial pressure, and cause hypovolemic shock. Septic shock may also develop. Shock of mixed character (with signs of both hypovolemic and septic shock) are more common in severe salmonellosis. Oliguria and azotemia develop in severe cases as a result of renal involvement due to hypoxia and toxemia.[3]
Causes

- Contaminated food, often having no unusual look or smell;
- Poor kitchen hygiene, especially problematic in institutional kitchens and restaurants because this can lead to a significant outbreak;
- Excretions from either sick or infected but apparently clinically healthy people and animals (especially dangerous are caregivers and animals);
- Polluted surface water and standing water (such as in shower hoses or unused water dispensers);
- Unhygienically thawed fowl (the meltwater contains many bacteria);
- An association with reptiles (pet tortoises, snakes, iguanas,[7][8] and aquatic turtles) is well described.[9]
- Amphibians such as frogs may also carry the disease.
Salmonella bacteria can survive for some time without a host; thus, they are frequently found in polluted water, with contamination from the excrement of carrier animals being particularly important.
The European Food Safety Authority (EFSA) highly recommends that when handling raw turkey meat, consumers and people involved in the food supply chain should pay attention to personal and food hygiene.[10]
An estimated 142,000 Americans are infected each year with Salmonella Enteritidis from chicken eggs,[11] and about 30 die.[12] The shell of the egg may be contaminated with Salmonella by feces or environment, or its interior (yolk) may be contaminated by penetration of the bacteria through the porous shell or from a hen whose infected ovaries contaminate the egg during egg formation.[13][14]
Nevertheless, such interior egg yolk contamination is theoretically unlikely.[15][16][17][18] Even under natural conditions, the rate of infection was very small (0.6% in a study of naturally contaminated eggs[19] and 3.0% among artificially and heavily infected hens[20]).
Prevention
The FDA has published guidelines[21] to help reduce the chance of food-borne salmonellosis. Food must be cooked to 68–72°C (145–160°F), and liquids such as soups or gravies must be boiled. Freezing kills some Salmonella, but it is not sufficient to reliably reduce them below infectious levels. While Salmonella is usually heat-sensitive, it does acquire heat resistance in high-fat environments such as peanut butter.[22]
Vaccine
Salmonella antibodies were first found in Malawi children in research published in 2008. The Malawian researchers have identified an antibody that protects children against bacterial infections of the blood caused by Salmonella. A study at Queen Elizabeth Hospital in Blantyre found that children up to two years old develop antibodies that aid in killing the bacteria. This could lead to a possible Salmonella vaccine.[23]
A recent study has tested a vaccine on chickens which offered efficient protection against salmonellosis. [24]
Treatment
Electrolytes may be replenished with oral rehydration supplements (typically containing salts sodium chloride and potassium chloride). Appropriate antibiotics, such as ceftriaxone, are given to kill the bacteria. Azithromycin has been suggested to be better at treating typhoid in resistant populations than both fluoroquinolone drugs and ceftriaxone. Antibiotic resistance rates are increasing throughout the world, so health care providers should check current recommendations before choosing an antibiotic.
Epidemiology
About 142,000 people in the United States are infected each year with Salmonella Enteritidis from chicken eggs, and about 30 die.[12]
In 2010, an analysis of death certificates in the United States identified a total of 1,316 Salmonella-related deaths from 1990 to 2006. These were predominantly among older adults and those who were immunocompromised.[25]
Before 2006
The U.S. Government reported as many as 20% of all chickens were contaminated with Salmonella in the late 1990s, and 16.3% were contaminated in 2005.[26] In the mid- to late 20th century, Salmonella enterica serovar Enteritidis was a common contaminant of eggs. This is much less common now with the advent of hygiene measures in egg production, and the vaccination of laying hens to prevent Salmonella colonization. Various Salmonella serovars (strains) also cause severe diseases in animals.
2006
In June 2006, the BBC reported the Cadbury chocolate manufacturer withdrew a number of products contaminated with Salmonella, which had resulted in up to 56 cases of salmonellosis.[27] The causes had been traced to a leaking pipe at a Cadbury plant in Herefordshire in January 2006, though the announcement was not made until June.
2007
In February 2007, the U.S. Food and Drug Administration (FDA) issued a warning to consumers not to eat certain jars of Peter Pan or Great Value peanut butter, due to risk of contamination with Salmonella Tennessee.
In March 2007, around 150 people were diagnosed with salmonellosis after eating tainted food at a governor's reception in Krasnoyarsk, Russia. Over 1,500 people attended the ball on March 1, and fell ill as a consequence of ingesting salmonella-tainted sandwiches.
About 150 people were sickened by salmonella-tainted chocolate cake produced by a major bakery chain in Singapore, in December 2007.
2008
From April 10, 2008 to July 8, 2008, the rare Saintpaul serotype of S. enteritidis caused at least 1017 cases of salmonellosis food poisoning in 41 states throughout the United States, the District of Columbia, and Canada. As of July 2008, the U.S. FDA suspected the contaminated food product was a common ingredient in fresh salsa, such as raw tomato, fresh jalapeño pepper, fresh serrano pepper, and fresh cilantro. It is the largest reported salmonellosis outbreak in the United States since 1985. New Mexico and Texas have been proportionally the hardest hit by far, with 49.7 and 16.1 reported cases per million, respectively. The greatest number of reported cases have occurred in Texas (384), New Mexico (98), Illinois (100), and Arizona (49).[28] At least 203 reported hospitalizations have been linked to the outbreak, it has caused at least one death, and it may have been a contributing factor in at least one additional death.[29] The CDC maintains "it is likely many more illnesses have occurred than those reported." If applying a previous CDC-estimated ratio of unreported salmonellosis cases to reported cases (38.6:1), an estimated 40,273 illnesses occurred from this outbreak.[30]
As of 18 July 2008, the FDA removed raw tomatoes and cilantro as potential carriers; however, fresh jalapeño and serrano peppers still remain.[31]
In December 2008 and January 2009, several Midwestern states, including Ohio (officially confirmed by state authorities), reported an outbreak of salmonellosis from Salmonella typhimurium that had sickened at least 50 people, due to contaminated dairy products such as cheeses.
2009
On January 17, 2009, the FDA announced they had traced the source of an outbreak of Salmonella typhimurium to a plant in Blakely, Georgia, owned by Peanut Corporation of America (PCA), and urged people to postpone eating commercially prepared or manufactured peanut butter-containing products and institutionally served peanut butter.[32] Salmonella was reported to be found in 46 states in the United States in at least 3,862 peanut butter-based products, such as crackers, energy bars, and peanut butter cookies from at least 343 food companies. Dog treats were affected, as well. At least 691 people in more than 46 states became sick, and the Salmonella claimed at least 9 lives as of March 25.[33][34][35][36][37]
Peanut butter and peanut paste manufactured by PCA were distributed to hundreds of firms for use as an ingredient in thousands of different products, such as cookies, crackers, cereal, candy and ice cream, all of which were recalled. Some products were also sold directly to consumers in retail outlets, such as dollar stores.[32]
On March 14, 2009, expressing his own personal concern for the safety of his children who enjoy peanut butter, President Obama announced the establishment of the Food Safety Working Group, "an inter-agency effort to help overhaul the oversight system." [38] The announcement came days after the FDA, also responding, released its first "guidance" on dealing with Salmonella contamination.
2012
An outbreak of salmonellosis caused by a rarer subspecies, Salmonella bareilly, was reported in multiple states mostly in the East, having yet caused no deaths, but many episodes of sickness and some hospitalizations have been linked to the consumption of raw scraped ground tuna product.[39]
Since July 2012, an outbreak of salmonellosis occurred in Northern Europe caused by Salmonella thompson. The infections were linked to smoked salmon from the manufacterer Foppen, where the contamination had occurred. Most infections were reported in the Netherlands, over 1060 infections with this subspecies have been confirmed, as well as four mortalities.[40][41]
A case of widespread infection was detected mid-2012 in seven EU countries. Over 400 people had been infected with Salmonella enterica serovar Stanley (S. Stanley) that usually appears in the regions of Southeast Asia. After several DNA analyses seemed to point to a specific Belgian strain, the "Joint ECDC/E FSA Rapid Risk Assessment" report detected turkey production as the source of infection.[42]
History
Both salmonellosis and the Salmonella genus of microorganisms derive their names from a modern Latin coining after Daniel E. Salmon (1850–1914), an American veterinary surgeon. He had help from Theobald Smith, and together they found the bacterium in pigs.
Four-inch regulation
The "Four-inch regulation" or "Four-inch law" is a colloquial name for a regulation issued by the U.S. FDA in 1975, restricting the sale of turtles with a carapace length of less than four inches (10 cm).[43]
The regulation was introduced, according to the FDA, "because of the public health impact of turtle-associated salmonellosis." There had been reported cases of young children placing small turtles in their mouths, which led to the size-based restriction.
See also
References
- ↑ Salmonella, FoodSafety.gov
- ↑ 2.0 2.1 2.2 "FDA/CFSAN - Food Safety A to Z Reference Guide - Salmonella". FDA - Center for Food Safety and Applied Nutrition. 2008-07-03. Retrieved 2009-02-14.
- ↑ 3.0 3.1 Santos, Renato L.; Shuping Zhang; Renee M. Tsolis; Robert A. Kingsley; L. Gary Adams; Adreas J. Baumler (2001). "Animal models od Salmonella infections: enteritis versus typhoid fever". Microbes and Infection 3: 1335–1344. doi:10.1016/s1286-4579(01)01495-2.
- ↑ "What is Salmonellosis?". US Center of Disease Control and Prevention.
- ↑ Leirisalo-Repo, M; P Helenius; T Hannu; A Lehtinen; J Kreula; M Taavitsainen; S Koskimies (1997). "Long term prognosis of reactive salmonella arthritis". Annals of the Rheumatic Diseases 59 (9): 516–520.
- ↑ Dworkin MS, Shoemaker PC, Goldoft MJ, Kobayashi JM (2001). "Reactive arthritis and Reiter's syndrome following an outbreak of gastroenteritis caused by Salmonella enteritidis". Clin Infect Dis 33 (7): 1010–14. doi:10.1086/322644. PMID 11528573.
- ↑ "Reptile-Associated Salmonellosis—Selected States, 1998–2002". Centers for Disease Control and Prevention. 12 December 2003. Retrieved 9 October 2011.
- ↑ Mermin J, Hoar B, Angulo FJ (March 1997). "Iguanas and Salmonella marina infection in children: a reflection of the increasing incidence of reptile-associated salmonellosis in the United States". PubMed 99 (3): 399–402. doi:10.1542/peds.99.3.399. PMID 9041295.
- ↑ "Ongoing investigation into reptile associated salmonella infections". Health Protection Report 3 (14). 9 April 2009. Retrieved 12 April 2009.
- ↑ "Multi-country outbreak of Salmonella Stanley infections Update". EFSA journal (European Food Safety Authority). 21 September 2012. doi:10.2903/j.efsa.2012.2893.
- ↑ "Playing It Safe With Eggs". FDA Food Facts. 2013-02-28. Retrieved 2013-03-02.
The U.S. Food and Drug Administration (FDA) estimates that 142,000 illnesses each year are caused by consuming eggs contaminated with Salmonella.
- ↑ 12.0 12.1 Black, Jane; O'Keefe, Ed (2009-07-08). "Administration Urged to Boost Food Safety Efforts". Washington Post. Retrieved 2009-07-07.
Among them is a final rule, issued by the FDA, to reduce the contamination in eggs. About 142,000 Americans are infected each year with Salmonella enteritidis from eggs, the result of an infected hen passing along the bacterium. About 30 die.
- ↑ Gantois, Inne; Richard Ducatelle; Frank Pasmans; Freddy Haesebrouck; Richard Gast; Tom J. Humphrey; Filip Van Immerseel (July 2009). "Mechanisms of egg contamination by Salmonella Enteritidis". FEMS Microbiology Reviews 33 (4): 718–738. doi:10.1111/j.1574-6976.2008.00161.x. PMID 19207743.
Eggs can be contaminated on the outer shell surface and internally. Internal contamination can be the result of penetration through the eggshell or by direct contamination of egg contents before oviposition, originating from infection of the reproductive organs. Once inside the egg, the bacteria need to cope with antimicrobial factors in the albumen and vitelline membrane before migration to the yolk can occur
- ↑ Humphrey, T. J. (January 1994). "Contamination of egg shell and contents with Salmonella enteritidis: a review". International Journal of Food Microbiology 21 (1–2): 31–40. doi:10.1016/0168-1605(94)90197-X. PMID 8155476. Retrieved 2010-08-19.
Salmonella enteritidis can contaminate the contents of clean, intact shell eggs as a result of infections of the reproductive tissue of laying hens. The principal site of infection appears to be the upper oviduct. In egg contents, the most important contamination sites are the outside of the vitelline membrane or the albumen surrounding it. In fresh eggs, only a few salmonellae are present. As albumen is an iron-restricted environment, growth only occurs with storage-related changes to vitelline membrane permeability, which allows salmonellas to invade yolk contents.
- ↑ Stokes, J.L.; W.W. Osborne, H.G. Bayne (September 1956). "Penetration and Growth of Salmonella in Shell Eggs". Journal of Food Science 21 (5): 510–518. doi:10.1111/j.1365-2621.1956.tb16950.x.
Normally, the oviduct of the hen is sterile and therefore the shell and internal contents of the egg are also free of microorganisms (10,16). In some instances, however, the ovaries and oviduct may be infected with Salmonella and these may be deposited inside the egg (12). More frequently, however, the egg becomes contaminated after it is laid.
- ↑ Okamura, Masashi; Yuka Kamijima; Tadashi Miyamoto; Hiroyuki Tani; Kazumi Sasai; Eiichiroh Baba (2001). "Differences Among Six Salmonella Serovars in Abilities to Colonize Reproductive Organs and to Contaminate Egges in Laying Hens". Avian Diseases 45 (1): 61–69. doi:10.2307/1593012. JSTOR 1593012. PMID 11332500.
when hens were artificially infected to test for transmission rate to yolks: "Mature laying hens were inoculated intravenously with 106 colony-forming units of Salmonella Enteritidis, Salmonella Typhimurium, Salmonella Infantis, Salmonella Hadar, Salmonella Heidelberg, or Salmonella Montevideo to cause the systemic infection. Salmonella Enteritidis was recovered from three yolks of the laid eggs (7.0%), suggesting egg contamination from the transovarian transmission of S. enteritidis."
- ↑ Gast, RK; D.R. Jones, K.E. Anderson, R. Guraya, J. Guard, P.S. Holt (August 2010). "In vitro penetration of Salmonella Enteritidis through yolk membranes of eggs from 6 genetically distinct commercial lines of laying hens". Poultry Science 89 (8): 1732–1736. doi:10.3382/ps.2009-00440. PMID 20634530. Retrieved 2010-08-20.
In this study, egg yolks were infected at the surface of the yolk (vitelline membrane) to determine the percentage of yolk contamination (a measure used to determine egg contamination resistance, with numbers lower than 95% indicating increasing resistance): Overall, the frequency of penetration of Salmonella Enteritidis into the yolk contents of eggs from individual lines of hens ranged from 30 to 58% and the mean concentration of Salmonella Enteritidis in yolk contents after incubation ranged from 0.8 to 2.0 log10 cfu/mL.
- ↑ Jaeger, Gerald (Jul–Aug 2009). "Contamination of eggs of laying hens with S. Enteritidis". Veterinary Survey (Tierärztliche Umschau) 64 (7–8): 344–348. Retrieved 2010-08-20.
The migration of the bacterium into the nutritionally rich yolk is constrained by the lysozyme loaded vitelline membrane, and would need warm enough storage conditions within days and weeks. The high concentration on of antibodies of the yolk does not inhibit the Salmonella multiplication. Only seldom does transovarian contamination of the developing eggs with S. Enteritidis make this bacterium occur in laid eggs, because of the bactericidal efficacy of the antimicrobial peptides
- ↑ Humphrey, T.J.; A. Whitehead, A. H. L. Gawler, A. Henley and B. Rowe (1991). "Numbers of Salmonella enteritidis in the contents of naturally contaminated hens' eggs". Epidemiology and Infection 106 (3): 489–496. doi:10.1017/S0950268800067546. PMC 2271858. PMID 2050203. Retrieved 2010-08-19.
Over 5700 hens eggs from 15 flocks naturally infected with Salmonella enteritidis were examined individually for the presence of the organism in either egg contents or on shells. Thirty-two eggs (0·6%) were positive in the contents. In the majority, levels of contamination were low.
- ↑ Gast, Richard; Rupa Guraya; Jean Guard; Peter Holt; Randle Moore (March 2007). "Colonization of specific regions of the reproductive tract and deposition at different locations inside eggs laid by hens infected with Salmonella Enteritidis or Salmonella Heidelberg". Journal of Avian Diseases 51 (1): 40–44. doi:10.1637/0005-2086(2007)051[0040:cosrot]2.0.co;2. PMID 17461265. Retrieved 2010-08-20.
when hens are artificially infected with unrealistically large doses (according to the author): In the present study, groups of laying hens were experimentally infected with large oral doses of Salmonella Heidelberg, Salmonella Enteritidis phage type 13a, or Salmonella Enteritidis phage type 14b. For all of these isolates, the overall frequency of ovarian colonization (34.0%) was significantly higher than the frequency of recovery from either the upper (22.9%) or lower (18.1%) regions of the oviduct. No significant differences were observed between the frequencies of Salmonella isolation from egg yolk and albumen (4.0% and 3.3%, respectively).
- ↑ "Salmonella Questions and Answers". USDA Food Safety and Inspection Service. 2006-09-20. Retrieved 2009-01-21.
- ↑ "FDA issues peanut safety guidelines for foodmakers". Reuters. 2009-03-10.
- ↑ MacLennan CA, Gondwe EN, Msefula CL et al. (April 2008). "The neglected role of antibody in protection against bacteremia caused by nontyphoidal strains of Salmonella in African children". J. Clin. Invest. 118 (4): 1553–62. doi:10.1172/JCI33998. PMC 2268878. PMID 18357343.
- ↑ Nandre, Rahul M.; Lee, John Hwa (Jan 2014). "Construction of a recombinant-attenuated Salmonella Enteritidis strain secreting Escherichia coli heat-labile enterotoxin B subunit protein and its immunogenicity and protection efficacy against salmonellosis in chickens.". Vaccine 32 (2): 425–431. doi:10.1016/j.vaccine.2013.10.054. PMID 24176491.
- ↑ Cummings, PL; Sorvillo F; Kuo T (November 2010). "Salmonellosis-related mortality in the United States, 1990–2006". Foodborne pathogens and disease 7 (11): 1393–9. doi:10.1089/fpd.2010.0588. PMID 20617938.
- ↑ Burros, Marian (March 8, 2006). "More Salmonella Is Reported in Chickens". The New York Times. Retrieved 2007-05-13.
- ↑ Tran, Mark (2006-07-21). "Cadbury named over salmonella outbreak". London: Guardian Unlimited. Retrieved 2007-09-09.
- ↑ "Cases infected with the outbreak strain of Salmonella Saintpaul, United States, by state". For some states, such as California, the CDC has recently revised the tally of identified illness downward.
- ↑ August 8, 2008: Investigation of Outbreak of Infections Caused by Salmonella Saintpaul | Salmonella CDC
- ↑ Voetsch et al. (2004-04-15). "FoodNet Estimate of the Burden of Illness Caused by Nontyphoidal Salmonella Infections in the United States". Clinical Infectious Diseases, 2004; 38:S3.
- ↑ Elizabeth Landau (2008-07-18). "FDA lifts warning on tomatoes". CNN.
- ↑ 32.0 32.1 Recall of Products Containing Peanut Butter: Salmonella Typhimurium, U.S. Food and Drug Administration.
- ↑ Recall of Peanut-Containing Products: Salmonella Typhimurium (Current Update), U.S. Food and Drug Administration
- ↑ Investigation Update: Outbreak of Salmonella Typhimurium Infections, 2008–2009, Centers for Disease Control and Prevention
- ↑ "More peanut products recalled, U.S. probe continues". Reuters. 2009-01-19.
- ↑ MSNBC: http://www.msnbc.msn.com/id/28749159
- ↑ "Peanut Plant Had History of Health Lapses". The New York Times. 2009-01-27. Retrieved 2010-05-23.
- ↑ Weise, Elizabeth (March 2009). "Salmonella outbreaks lead to food-safety changes". USA Today.
- ↑ "Multistate Outbreak of Salmonella Bareilly Infections Associated with a Raw Scraped Ground Tuna Product"
- ↑ Veelgestelde vragen Salmonella Thompson 15 oktober 2012, Rijksinstituut voor Volksgezondheid en Milieu [Frequently asked questions Salmonella Thompson 15 October 2012, Netherlands Institute for Public Health and the Environment].
- ↑ "Salmonella besmetting neemt verder af, 2 november 2012, Rijksinstituut voor Volksgezondheid en Milieu" [Salmonella infections continue to decline 2 November 2012, Netherlands Institute for Public Healthand the Environment].
- ↑ Multi-country outbreak of Salmonella Stanley infections Update EFSA Journal 2012;10(9):2893 [16 pp.]. Retrieved 04/23/2013
- ↑ "Human Health Hazards Associated with Turtles". U.S. Food and Drug Administration. Archived from the original on 2007-06-09. Retrieved 2007-06-29.
External links
| Wikimedia Commons has media related to Salmonella. |
- CDC website, Division of Bacterial and Mycotic Diseases, Disease Listing: Salmonellosis
- CFIA Website: Salmonellae
- Protective salmonella antibodies found in Malawi children, Sub-Saharan Africa gateway, Science and Development Network,