Radiation hormesis
Radiation hormesis (also called radiation homeostasis) is the hypothesis that low doses of ionizing radiation (within the region of and just above natural background levels) are beneficial, stimulating the activation of repair mechanisms that protect against disease, that are not activated in absence of ionizing radiation. The reserve repair mechanisms are hypothesized to be sufficiently effective when stimulated as to not only cancel the detrimental effects of ionizing radiation but also inhibit disease not related to radiation exposure (see hormesis).[1][2][3][4] This counter-intuitive hypothesis has captured the attention of scientists and public alike in recent years.[5]
While the effects of high and acute doses of ionising radiation are easily observed and understood in humans (e.g. Japanese Atomic Bomb survivors), the effects of low-level radiation are very difficult to observe and highly controversial. This is because baseline cancer rate is already very high and the risk of developing cancer fluctuates 40% because of individual life style and environmental effects,[6][7] obscuring the subtle effects of low-level radiation. An acute dose of 100 mSv may increase cancer risk by ~0.8%.
Government and regulatory bodies disagree on the existence of radiation hormesis.
Quoting results from a literature database research, the Académie des Sciences — Académie nationale de Médecine (French Academy of Sciences — National Academy of Medicine) stated in their 2005 report concerning the effects of low-level radiation that many laboratory studies have observed radiation hormesis.[8][9] However, they cautioned that it is not yet known if radiation hormesis occurs outside the laboratory, or in humans.[10]
Reports by the United States National Research Council and the National Council on Radiation Protection and Measurements and the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) argue[11] that there is no evidence for hormesis in humans and in the case of the National Research Council, that hormesis is outright rejected as a possibility despite population and scientific evidence.[12] Therefore, estimating Linear no-threshold model (LNT) continues to be the model generally used by regulatory agencies for human radiation exposure.
Proposed mechanism and ongoing debate
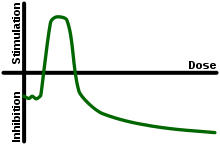
Radiation hormesis proposes that radiation exposure comparable to and just above the natural background level of radiation is not harmful but beneficial, while accepting that much higher levels of radiation are hazardous. Proponents of radiation hormesis typically claim that radio-protective responses in cells and the immune system not only counter the harmful effects of radiation but additionally act to inhibit spontaneous cancer not related to radiation exposure. Radiation hormesis stands in stark contrast to the more generally accepted linear no-threshold model (LNT), which states that the radiation dose-risk relationship is linear across all doses, so that small doses are still damaging, albeit less so than higher ones. Opinion pieces on chemical and radiobiological hormesis appeared in the journals Nature[1] and Science[3] in 2003.
Assessing the risk of radiation at low doses (<100 mSv) and low dose rates (<0.1 mSv.min−1) is highly problematic and controversial.[13][14] While epidemiological studies on populations of people exposed to an acute dose of high level radiation such as Japanese Atomic Bomb Survivors (hibakusha (被爆者)) have robustly upheld the LNT (mean dose ~210 mSv),[15] studies involving low doses and low dose rates have failed to detect any increased cancer rate.[14] This is because the baseline cancer rate is already very high (~42 of 100 people will be diagnosed in their lifetime) and it fluctuates ~40% because of lifestyle and environmental effects,[7][16] obscuring the subtle effects of low level radiation. Epidemiological studies maybe capable of detecting elevated cancer rates as low as 1.2 to 1.3 i.e. 20% to 30% increase. But for low doses (1–100 mSv) the predicted elevated risks are only 1.001 to 1.04 and excess cancer cases, if present, cannot be detected due to confounding factors, errors and biases.[16][17] New studies, however, have concluded that there is, in fact, a statistically significant indication of Radiation hormesis.[18]
In particular, variations in smoking prevalence or even accuracy in reporting smoking cause wide variation in excess cancer and measurement error bias. Thus, even a large study of many thousands of subjects with imperfect smoking prevalence information will fail to detect the effects of low level radiation than a smaller study that properly compensates for smoking prevalence.[19] Given the absence of direct epidemiological evidence, there is considerable debate as to whether the dose-response relationship <100 mSv is supralinear, linear (LNT), has a threshold or sub-linear i.e. a hormetic response.
While most major consensus reports and government bodies currently adhere to LNT,[20] the 2005 French Academy of Sciences-National Academy of Medicine's report concerning the effects of low-level radiation rejected LNT as a scientific model of carcinogenic risk at low doses.[10]
"Using LNT to estimate the carcinogenic effect at doses of less than 20 mSv is not justified in the light of current radiobiologic knowledge."
They consider there to be several dose-effect relationships rather than only one, and that these relationships have many variables such as target tissue, radiation dose, dose rate and individual sensitivity factors. They request that further study is required on low doses (less than 100 mSv) and very low doses (less than 10 mSv) as well as the impact of tissue type and age. The Academy considers the LNT model is only useful for regulatory purposes as it simplifies the administrative task. Quoting results from literature research,[8][9] they furthermore claim that approximately 40% of laboratory studies on cell cultures and animals indicate some degree of chemical or radiobiological hormesis, and state:
"...its existence in the laboratory is beyond question and its mechanism of action appears well understood."
They go on to outline a growing body of research that illustrates that the human body is not a passive accumulator of radiation damage but it actively repairs the damage caused via a number of different processes, including:[10][14]
- Mechanisms that mitigate reactive oxygen species generated by ionizing radiation and oxidative stress.
- Apoptosis of radiation damaged cells that may undergo tumorigenesis is initiated at only few mSv.
- Cell death during meiosis of radiation damaged cells that were unsuccessfully repaired.
- The existence of a cellular signaling system that alerts neighboring cells of cellular damage.
- The activation of enzymatic DNA repair mechanisms around 10 mSv.
- Modern DNA microarray studies which show that numerous genes are activated at radiation doses well below the level that mutagenesis is detected.
- Radiation-induced tumorigenesis may have a threshold related to damage density, as revealed by experiments that employ blocking grids to thinly distribute radiation.
- A large increase in tumours in immunosuppressed individuals illustrates that the immune system efficiently destroys aberrant cells and nascent tumors.
Furthermore, increased sensitivity to radiation induced cancer in the inherited condition Ataxia-telangiectasia like disorder, illustrates the damaging effects of loss of the repair gene Mre11h resulting in the inability to fix DNA double-strand breaks.[21]
The BEIR-VII report argued that, "the presence of a true dose threshold demands totally error-free DNA damage response and repair." The specific damage they worry about is double strand breaks (DSBs) and they continue, "error-prone nonhomologous end joining (NHEJ) repair in postirradiation cellular response, argues strongly against a DNA repair-mediated low-dose threshold for cancer initiation".[22] Resent research observed that DSBs caused by CAT scans are repaired within 24-hours and DSBs maybe more efficiently repaired at low doses, suggesting the risk ionizing radiation at low doses may not by directly proportional to the dose.[23][24] However, it is not known if low dose ionizing radiation stimulates the repair of DSBs not caused by ionizing radiation i.e. a hormetic response.
Radon gas in homes is the largest source of radiation dose for most individuals and it is generally advised that the concentration be kept below 150 Bq/m³ (4 pCi/L).[25] A recent retrospective case-control study of lung cancer risk showed substantial cancer rate reduction between 50 and 123 Bq per cubic meter relative to a group at zero to 25 Bq per cubic meter.[26] This study is cited as evidence for hormesis, but a single study all by itself cannot be regarded as definitive. Other studies into the effects of domestic radon exposure have not reported a hormetic effect; including for example the respected "Iowa Radon Lung Cancer Study" of Field et al. (2000), which also used sophisticated radon exposure dosimetry.[27] In addition, Darby et al. (2005) argue that radon exposure is negatively correlated with the tendency to smoke and environmental studies need to accurately control for this; people living in urban areas where smoking rates are higher usually have lower levels of radon exposure due the increased prevalence of multi-story dwellings.[28] When doing so, they found a significant increase in lung cancer amongst smokers exposed to radon at doses as low as 100 to 199 Bq m−3 and warned that smoking greatly increases the risk posed by radon exposure i.e. reducing the prevalence of smoking would decrease deaths caused by radon.[28][29]
Furthermore, particle microbeam studies show that passage of even a single alpha particle (e.g. from radon and its progeny) through cell nuclei is highly mutagenic,[30] and that alpha radiation may have a higher mutagenic effect at low doses (even if a small fraction of cells are hit by alpha particles) than predicted by linear no-threshold model, a phenomenon attributed to bystander effect.[31] However, there is currently insufficient evidence at hand to suggest that the bystander effect promotes carcinogenesis in humans at low doses.[32]
Statements by leading nuclear bodies
Radiation hormesis has not been accepted by either the United States National Research Council,[33] or the National Council on Radiation Protection and Measurements.[34] In addition, the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) wrote in its most recent report:[35]
Until the [...] uncertainties on low-dose response are resolved, the Committee believes that an increase in the risk of tumour induction proportionate to the radiation dose is consistent with developing knowledge and that it remains, accordingly, the most scientifically defensible approximation of low-dose response. However, a strictly linear dose response should not be expected in all circumstances.
This is a reference to the fact that very low doses of radiation have only marginal impacts on individual health outcomes. It is therefore difficult to detect the 'signal' of decreased or increased morbidity and mortality due to low-level radiation exposure in the 'noise' of other effects. The notion of radiation hormesis has been rejected by the National Research Council's (part of the National Academy of Sciences) 16-year-long study on the Biological Effects of Ionizing Radiation. "The scientific research base shows that there is no threshold of exposure below which low levels of ionizing radiation can be demonstrated to be harmless or beneficial. The health risks – particularly the development of solid cancers in organs – rise proportionally with exposure" says Richard R. Monson, associate dean for professional education and professor of epidemiology, Harvard School of Public Health, Boston.[36][37]
The possibility that low doses of radiation may have beneficial effects (a phenomenon often referred to as “hormesis”) has been the subject of considerable debate. Evidence for hormetic effects was reviewed, with emphasis on material published since the 1990 BEIR V study on the health effects of exposure to low levels of ionizing radiation. Although examples of apparent stimulatory or protective effects can be found in cellular and animal biology, the preponderance of available experimental information does not support the contention that low levels of ionizing radiation have a beneficial effect. The mechanism of any such possible effect remains obscure. At this time, the assumption that any stimulatory hormetic effects from low doses of ionizing radiation will have a significant health benefit to humans that exceeds potential detrimental effects from radiation exposure at the same dose is unwarranted.—[37]
Studies of low level radiation
Very high natural background gamma radiation cancer rates at Kerala, India
Kerala's monazite sand (containing a third of the world's economically recoverable reserves of radioactive thorium) emits about 8 micro Sieverts per hour of gamma radiation, 80 times the dose rate equivalent in London, but a decade long study of 69,985 residents published in Health Physics in 2009: "showed no excess cancer risk from exposure to terrestrial gamma radiation. The excess relative risk of cancer excluding leukemia was estimated to be -0.13 Gy_1 (95% CI: -0.58, 0.46)", indicating no statistically significant positive or negative relationship between background radiation levels and cancer risk in this sample.[38]
Cultures
Studies in cell cultures can be useful for finding mechanisms for biological processes, but they also can be criticized for not effectively capturing the whole of the living organism.
A study by E.I. Azzam suggested that pre-exposure to radiation causes cells to turn on protection mechanisms.[39] A different study by de Toledo and collaborators, has shown that irradiation with gamma rays increases the concentration of glutathione, an antioxidant found in cells.[40]
In 2011, an in vitro study led by S.V. Costes showed in time-lapse images a strongly non-linear response of certain cellular repair mechanisms called radiation-induced foci (RIF). The study found that low doses of radiation prompted higher rates of RIF formation than high doses, and that after low-dose exposure RIF continued to form after the radiation had ended. Measured rates of RIF formation were 15 RIF/Gy at 2 Gy, and 64 RIF/Gy at .1 Gy.[24] These results suggest that low dose levels of ionizing radiation may not increase cancer risk directly proportional to dose and thus contradict the linear-no-threshold standard model.[41] Mina Bissell, a world-renowned breast cancer researcher and collaborator in this study stated “Our data show that at lower doses of ionizing radiation, DNA repair mechanisms work much better than at higher doses. This non-linear DNA damage response casts doubt on the general assumption that any amount of ionizing radiation is harmful and additive.”[41]
Animals
A study by Otsuka and collaborators find hormesis in animals.[42] Miyachi conducted a study on mice and found that a 200 mGy X-ray dose protects mice against both further X-ray exposure and ozone gas.[43] In another rodent study, Sakai and collaborators found that (1 mGy/hr) gamma irradiation prevents the development of cancer (induced by chemical means, injection of methylcholanthrene).[44]
In a 2006 paper,[45] a dose of 1 Gy was delivered to the cells (at constant rate from a radioactive source) over a series of lengths of time. These were between 8.77 and 87.7 hours, the abstract states for a dose delivered over 35 hours or more (low dose rate) no transformation of the cells occurred. Also for the 1 Gy dose delivered over 8.77 to 18.3 hours that the biological effect (neoplastic transformation) was about "1.5 times less than that measured at high dose rate in previous studies with a similar quality of [X-ray] radiation." Likewise it has been reported that fractionation of gamma irradiation reduces the likelihood of a neoplastic transformation.[46] Pre-exposure to fast neutrons and gamma rays from Cs-137 is reported to increase the ability of a second dose to induce a neoplastic transformation.[47]
Caution must be used in interpreting these results, as it noted in the BEIR VII report, these pre-doses can also increase cancer risk:
In chronic low-dose experiments with dogs (75 mGy/d for the duration of life), vital hematopoietic progenitors showed increased radioresistance along with renewed proliferative capacity (Seed and Kaspar 1992). Under the same conditions, a subset of animals showed an increased repair capacity as judged by the unscheduled DNA synthesis assay (Seed and Meyers 1993). Although one might interpret these observations as an adaptive effect at the cellular level, the exposed animal population experienced a high incidence of myeloid leukemia and related myeloproliferative disorders. The authors concluded that “the acquisition of radioresistance and associated repair functions under the strong selective and mutagenic pressure of chronic radiation is tied temporally and causally to leukemogenic transformation by the radiation exposure” (Seed and Kaspar 1992).
However, 75 mGy/d cannot be accurately described as low dose rate radiation - it is over 27 Sieverts per year. The same study on dogs showed no increase in cancer nor reduction in life expectancy for dogs irradiated at 3 mGy/day.[48]
Humans
Effects of sunlight exposure
In an Australian study which analyzed the association between solar UV exposure and DNA damage, the results indicated that although the frequency of cells with chromosome breakage increased with increasing sun exposure, the misrepair of DNA strand breaks decreased as sun exposure was heightened.[49]
Effects of cobalt-60 exposure
The health of the inhabitants of radioactive apartment buildings in Taiwan has received prominent attention in popular treatments of radiation hormesis. In 1982, more than 20,000 tons of steel was accidentally contaminated with cobalt-60, much of this radioactive steel was used to build apartments and exposed thousands of Taiwanese to gamma radiation levels of up to >1000 times background (ave. 47.7 mSv, max. 2360 mSv excess cumulative dose); it was not until 1992 that the radioactive contamination was discovered. A medical study published in 2004 claimed the cancer mortality rates in the exposed population were much lower than expected.[50] However, this initial study failed to control for age, comparing a much younger exposed population (mean age 17.2 years at initial exposure) with the much older general population of Taiwan (mean age approx. 34 years in 2004), a serious flaw.[51][52] Older people have much higher cancer rates even in the absence of excess radiation exposure. However, Chen et al. did find a lower cancer incidence with time, still the opposite of what would be expected, even with a younger population.
A subsequent study by Hwang et al. (2006) found the incidence of "all cancers" in the irradiated population was 40% lower than expected (95 vs. 160.3 cases expected), except for leukaemia in men (6 vs. 1.8 cases expected) and thyroid cancer in women (6 vs. 2.8 cases expected), an increase only detected amongst those exposed before the age of 30. Hwang et al. proposed that the lower rate of "all cancers" might due to the exposed populations higher socioeconomic status and thus overall healthier lifestyle, but this was difficult to prove. Additionally, they cautioned that leukaemia was the first cancer type found to be elevated amongst the survivors of the Hiroshima and Nagasaki bombings, so it may be decades before any increase in more common cancer types are seen.[51]
Besides the excess risks of leukaemia and thyroid cancer, a later publication notes various DNA anomalies and other health effects among the exposed population:[53]
There have been several reports concerning the radiation effects on the exposed population, including cytogenetic analysis that showed increased micronucleus frequencies in peripheral lymphocytes in the exposed population, increases in acentromeric and single or multiple centromeric cytogenetic damages, and higher frequencies of chromosomal translocations, rings and dicentrics. Other analyses have shown persistent depression of peripheral leucocytes and neutrophils, increased eosinophils, altered distributions of lymphocyte subpopulations, increased frequencies of lens opacities, delays in physical development among exposed children, increased risk of thyroid abnormalities, and late consequences in hematopoietic adaptation in children.
Effects of no radiation
Given the uncertain effects of low-level and very-low-level radiation, there is a pressing need for quality research in this area. An expert panel convened at the 2006 Ultra-Low-Level Radiation Effects Summit at Carlsbad, New Mexico, proposed the construction of an Ultra-Low-Level Radiation laboratory.[54] The laboratory, if built, will investigate the effects of almost no radiation on laboratory animals and cell cultures, and it will compare these groups to control groups exposed to natural radiation levels. Precautions would be made, for example, to remove potassium-40 from the food of laboratory animals. The expert panel believes that the Ultra-Low-Level Radiation laboratory is the only experiment that can explore with authority and confidence the effects of low-level radiation; that it can confirm or discard the various radiobiological effects proposed at low radiation levels e.g. LNT, threshold and radiation hormesis.[55]
The first preliminary results of the effects of almost no-radiation on cell cultures was reported by two research groups in 2011 and 2012; researchers in the US studied cell cultures protected from radiation in a steel chamber 650 meters underground at the Waste Isolation Pilot Plant in Carlsbad, New Mexico[56] and researchers in Europe reported the effects of almost no-radiation on mouse cells (pKZ1 transgenic chromosomal inversion assay).[57]
See also
- Background radiation
- Dose fractionation
- Hormesis
- Linear no-threshold model
- Petkau effect
- Radioresistance
- Ramsar, Mazandaran
References
- ↑ 1.0 1.1 Calabrese, Edward J; Baldwin, Linda A (2003). "Toxicology rethinks its central belief". Nature 421 (6924): 691–2. Bibcode:2003Natur.421..691C. doi:10.1038/421691a. PMID 12610596.
- ↑ Feinendegen, L E (2005). "Evidence for beneficial low level radiation effects and radiation hormesis". British Journal of Radiology 78 (925): 3–7. doi:10.1259/bjr/63353075. PMID 15673519.
- ↑ 3.0 3.1 Kaiser, J. (2003). "HORMESIS: Sipping from a Poisoned Chalice". Science 302 (5644): 376–9. doi:10.1126/science.302.5644.376. PMID 14563981.
- ↑ Wolff, Sheldon (1998). "The Adaptive Response in Radiobiology: Evolving Insights and Implications". Environmental Health Perspectives 106: 277–83. doi:10.2307/3433927. JSTOR 3433927. PMC 1533272. PMID 9539019.
- ↑ Allison, Wade (2009). Radiation and Reason: The Impact of Science on a Culture of Fear. York, England: York Publishing Services. p. 2. ISBN 0-9562756-1-3.
- ↑ "WHO Cancer Fact sheet N°297". Retrieved 2011-04-29.
- ↑ 7.0 7.1 Parkin, D M; Boyd, L; Walker, L C (2011). "16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010". British Journal of Cancer 105 (Suppl 2): S77–81. doi:10.1038/bjc.2011.489. PMC 3252065. PMID 22158327.
- ↑ 8.0 8.1 Calabrese, Edward J (2004). "Hormesis: From marginalization to mainstream". Toxicology and Applied Pharmacology 197 (2): 125–36. doi:10.1016/j.taap.2004.02.007. PMID 15163548.
- ↑ 9.0 9.1 Duport, P. (2003). "A database of cancer induction by low-dose radiation in mammals: Overview and initial observations". International Journal of Low Radiation 1: 120–31. doi:10.1504/IJLR.2003.003488.
- ↑ 10.0 10.1 10.2 Aurengo (2005-03-30). "Dose-effect relationships and estimation of the carcinogenic effects of low doses of ionizing radiation". Académie des Sciences & Académie nationale de Médecine. CiteSeerX: 10
.1 ..1 .126 .1681 - ↑ UNSCEAR 2000 REPORT Vol. II: Sources and Effects of Ionizing Radiation: Annex G: Biological effects at low radiation doses.
- ↑ http://books.nap.edu/catalog/11340.html Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2
- ↑ Mullenders, Leon; Atkinson, Mike; Paretzke, Herwig; Sabatier, Laure; Bouffler, Simon (2009). "Assessing cancer risks of low-dose radiation". Nature Reviews Cancer 9 (8): 596–604. doi:10.1038/nrc2677. PMID 19629073.
- ↑ 14.0 14.1 14.2 Tubiana, M.; Feinendegen, L. E.; Yang, C.; Kaminski, J. M. (2009). "The Linear No-Threshold Relationship is Inconsistent with Radiation Biologic and Experimental Data1". Radiology 251 (1): 13–22. doi:10.1148/radiol.2511080671. PMC 2663584. PMID 19332842.
- ↑ Samartzis, Dino; Nishi, N; Hayashi, M; Cologne, J; Cullings, HM; Kodama, K; Miles, EF; Funamoto, S et al. (2011). "Exposure to Ionizing Radiation and Development of Bone Sarcoma: New Insights Based on Atomic-Bomb Survivors of Hiroshima and Nagasaki". The Journal of Bone & Joint Surgery (American) 93 (11): 1008–15. doi:10.2106/JBJS.J.00256. PMID 21984980.
- ↑ 16.0 16.1 Boice Jr, John D (2012). "Radiation epidemiology: A perspective on Fukushima". Journal of Radiological Protection 32 (1): N33–40. doi:10.1088/0952-4746/32/1/N33. PMID 22395193.
- ↑ Boice, John D. (2010). "INVITED EDITORIAL Uncertainties in studies of low statistical power Uncertainties in studies of low statistical power". Journal of Radiological Protection 30 (2): 115–20. Bibcode:2010JRP....30..115B. doi:10.1088/0952-4746/30/2/E02. PMID 20548136.
- ↑ Chen, W.; Luan, Y.; Shieh, M.; Chen, S.; Kung, H.; Soong, K.; Yeh, Y.; Chou, T. et al. (2007). "Effects of Cobalt-60 Exposure on Health of Taiwan Residents Suggest New Approach Needed in Radiation Protection". Dose-Response 5 (1): 63–75. doi:10.2203/dose-response.06-105.Chen. PMC 2477708. PMID 18648557.
- ↑ Lubin, Jay H.; Samet, Jonathan M.; Weinberg, Clarice (1990). "Design Issues in Epidemiologic Studies of Indoor Exposure to Rn and Risk of Lung Cancer". Health Physics 59 (6): 807–17. doi:10.1097/00004032-199012000-00004. PMID 2228608.
- ↑ Hall, Eric J. (1998). "From Chimney Sweeps to Astronauts". Health Physics 75 (4): 357–66. doi:10.1097/00004032-199810000-00001. PMID 9753358.
- ↑ Stewart, G; Maser, RS; Stankovic, T; Bressan, DA; Kaplan, MI; Jaspers, NG; Raams, A; Byrd, PJ et al. (1999). "The DNA Double-Strand Break Repair Gene hMRE11 is Mutated in Individuals with an Ataxia-Telangiectasia-like Disorder". Cell 99 (6): 577–87. doi:10.1016/S0092-8674(00)81547-0. PMID 10612394.
- ↑ BEIR VII, page 245
- ↑ Löbrich, Markus; Rief, Nicole; Kühne, Martin; Heckmann, Martina; Fleckenstein, Jochen; Rübe, Christian; Uder, Michael (2005). "In vivo formation and repair of DNA double-strand breaks after computed tomography examinations". Proceedings of the National Academy of Sciences 102 (25): 8984–9. Bibcode:2005PNAS..102.8984L. doi:10.1073/pnas.0501895102. PMC 1150277. PMID 15956203.
- ↑ 24.0 24.1 Neumaier, T.; Swenson, J.; Pham, C.; Polyzos, A.; Lo, A. T.; Yang, P.; Dyball, J.; Asaithamby, A. et al. (2012). "Evidence for formation of DNA repair centers and dose-response nonlinearity in human cells". Proceedings of the National Academy of Sciences 109 (2): 443–8. Bibcode:2012PNAS..109..443N. doi:10.1073/pnas.1117849108. PMC 3258602. PMID 22184222.
- ↑ "Surgeon General Releases National Health Advisory On Radon". US HHS Office of the Surgeon General. January 12, 2005. Retrieved 28 November 2008.
- ↑ Thompson, Richard E.; Nelson, Donald F.; Popkin, Joel H.; Popkin, Zenaida (2008). "Case-Control Study of Lung Cancer Risk from Residential Radon Exposure in Worcester County, Massachusetts". Health Physics 94 (3): 228–41. doi:10.1097/01.HP.0000288561.53790.5f. PMID 18301096.
- ↑ Field, R. W.; Steck, D. J.; Smith, B. J.; Brus, C. P.; Fisher, E. L.; Neuberger, J. S.; Platz, C. E.; Robinson, R. A. et al. (2000). "Residential Radon Gas Exposure and Lung Cancer: The Iowa Radon Lung Cancer Study". American Journal of Epidemiology 151 (11): 1091–102. doi:10.1093/oxfordjournals.aje.a010153. PMID 10873134.
- ↑ 28.0 28.1 Darby, S; Hill, D; Auvinen, A; Barros-Dios, JM; Baysson, H; Bochicchio, F; Deo, H; Falk, R et al. (2005). "Radon in homes and risk of lung cancer: Collaborative analysis of individual data from 13 European case-control studies". BMJ 330 (7485): 223. doi:10.1136/bmj.38308.477650.63. PMC 546066. PMID 15613366.
- ↑ Méndez, David; Alshanqeety, Omar; Warner, Kenneth E.; Lantz, Paula M.; Courant, Paul N. (2011). "The Impact of Declining Smoking on Radon-Related Lung Cancer in the United States". American Journal of Public Health 101 (2): 310–4. doi:10.2105/AJPH.2009.189225. PMC 3020207. PMID 21228294.
- ↑ Hei, Tom K.; Wu, Li-Jun; Liu, Su-Xian; Vannais, Diane; Waldren, Charles A.; Randers-Pehrson, Gerhard (1997). "Mutagenic Effects of a Single and an Exact Number of α Particles in Mammalian Cells". Proceedings of the National Academy of Sciences of the United States of America 94 (8): 3765–70. Bibcode:1997PNAS...94.3765H. doi:10.1073/pnas.94.8.3765. PMC 20515. PMID 9108052.
- ↑ Zhou, Hongning; Randers-Pehrson, Gerhard; Waldren, Charles A.; Vannais, Diane; Hall, Eric J.; Hei, Tom K. (2000). "Induction of a bystander mutagenic effect of alpha particles in mammalian cells". Proceedings of the National Academy of Sciences 97 (5): 2099–104. Bibcode:2000PNAS...97.2099Z. doi:10.1073/pnas.030420797. PMC 15760. PMID 10681418.
- ↑ Blyth, Benjamin J.; Sykes, Pamela J. (2011). "Radiation-Induced Bystander Effects: What Are They, and How Relevant Are They to Human Radiation Exposures?". Radiation Research 176 (2): 139–57. doi:10.1667/RR2548.1. PMID 21631286.
- ↑ http://books.nap.edu/catalog/11340.html Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2
- ↑ NCRP Report No. 136 — Evaluation of the Linear-Nonthreshold Dose-Response Model for Ionizing Radiation
- ↑ UNSCEAR 2000 REPORT Vol. II: Sources and Effects of Ionizing Radiation: Annex G: Biological effects at low radiation doses. page 160, paragraph 541.
- ↑ Vines, Vanee; Petty, Megan (2005-06-29). "Low Levels of Ionizing Radiation May Cause Harm". National Academy of Sciences. Retrieved 2010-01-27.
- ↑ 37.0 37.1 37.2 Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. National Academies Press. 2006. ISBN 978-0-309-09156-5. Retrieved 2010-01-27.
- ↑ Nair, Raghu Ram K.; Rajan, Balakrishnan; Akiba, Suminori; Jayalekshmi, P; Nair, M Krishnan; Gangadharan, P; Koga, Taeko; Morishima, Hiroshige et al. (2009). "Background Radiation and Cancer Incidence in Kerala, India—Karanagappally Cohort Study". Health Physics 96 (1): 55–66. doi:10.1097/01.HP.0000327646.54923.11. PMID 19066487.
- ↑ Azzam, E.I.; Raaphorst, G. P.; Mitchel, R. E. J. (1994). "Radiation-Induced Adaptive Response for Protection against Micronucleus Formation and Neoplastic Transformation in C3H 10T1/2 Mouse Embryo Cells". Radiation Research (Radiation Research, Vol. 138, No. 1) 138 (1): S28–S31. doi:10.2307/3578755. JSTOR 3578755. PMID 8146320.
- ↑ De Toledo, Sonia M.; Asaad, Nesrin; Venkatachalam, Perumal; Li, Ling; Howell, Roger W.; Spitz, Douglas R.; Azzam, Edouard I. (2006). "Adaptive Responses to Low-Dose/Low-Dose-Rate γ Rays in Normal Human Fibroblasts: The Role of Growth Architecture and Oxidative Metabolism". Radiation Research 166 (6): 849–57. doi:10.1667/RR0640.1. PMID 17149977.
- ↑ 41.0 41.1 http://www.healthcanal.com/public-health-safety/24865-New-Take-Impacts-Low-Dose-Radiation.html[]
- ↑ Otsuka, Kensuke; Koana, Takao; Tauchi, Hiroshi; Sakai, Kazuo (2006). "Activation of Antioxidative Enzymes Induced by Low-Dose-Rate Whole‐Body γ Irradiation: Adaptive Response in Terms of Initial DNA Damage". Radiation Research 166 (3): 474–8. doi:10.1667/RR0561.1. PMID 16953665.
- ↑ Miyachi, Y (2000). "Acute mild hypothermia caused by a low dose of X-irradiation induces a protective effect against mid-lethal doses of X-rays, and a low level concentration of ozone may act as a radiomimetic". The British Journal of Radiology 73 (867): 298–304. PMID 10817047.
- ↑ Sakai, Kazuo; Iwasaki, Toshiyasu; Hoshi, Yuko; Nomura, Takaharu; Oda, Takeshi; Fujita, Kazuko; Yamada, Takeshi; Tanooka, Hiroshi (2002). "Suppressive effect of long-term low-dose rate gamma-irradiation on chemical carcinogenesis in mice". International Congress Series 1236: 487. doi:10.1016/S0531-5131(01)00861-5.
- ↑ Elmore, E.; Lao, X-Y.; Kapadia, R.; Redpath, J. L. (2006). "The Effect of Dose Rate on Radiation-Induced Neoplastic TransformationIn Vitroby Low Doses of Low-LET Radiation". Radiation Research 166 (6): 832–8. doi:10.1667/RR0682.1. PMID 17149982.
- ↑ Hill, C.K.; Han, A.; Buonaguro, F.; Elkind, M.M. (1984). "Multifractionation of 60Co gamma-rays reduces neoplastic transformation in vitro". Carcinogenesis 5 (2): 193–7. doi:10.1093/carcin/5.2.193. PMID 6697436.
- ↑ Cao, J.; Wells, R.L.; Elkind, M.M. (1992). "Enhanced Sensitivity to Neoplastic Transformation by137Cs γ-rays of Cells in the G2-/M-phase Age Interval". International Journal of Radiation Biology 62 (2): 191–9. doi:10.1080/09553009214552011. PMID 1355513.
- ↑ http://www.nuclearsafety.gc.ca/eng/pdfs/Presentations/Guest-Speakers/2013/20130625-Cuttler-CNSC-Fukushima-and-beneficial-effects-low-radiation.pdf
- ↑ Nair-Shalliker, V.; Fenech, M.; Forder, P. M.; Clements, M. S.; Armstrong, B. K. (2012). "Sunlight and vitamin D affect DNA damage, cell division and cell death in human lymphocytes: A cross-sectional study in South Australia". Mutagenesis 27 (5): 609–14. doi:10.1093/mutage/ges026. PMID 22547344.
- ↑ Chen, W.L.; Luan, Y.C.; Shieh, M.C.; Chen, S.T.; Kung, H.T.; Soong, K.L.; Yeh, Y.C.; Chou, T.S.; Mong, S.H. (2004). "Is Chronic Radiation an Effective Prophylaxis Against Cancer?". Journal of the American Physicians and Surgeons 9 (1): 6–10.
- ↑ 51.0 51.1 Hwang, S. -L.; Guo, H. -R.; Hsieh, W. -A.; Hwang, J. -S.; Lee, S. -D.; Tang, J. -L.; Chen, C. -C.; Chang, T. -C. et al. (2006). "Cancer risks in a population with prolonged low dose-rate γ-radiation exposure in radiocontaminated buildings, 1983 – 2002". International Journal of Radiation Biology 82 (12): 849–58. doi:10.1080/09553000601085980. PMID 17178625.
- ↑ Chen, C. Y.; Y. J. Chen (2011). The Social Migration Effect Toward Population Aging-The Application of Perston’s Rate of Change of a Population’s Mean Age Improvement Model in Taiwan. The 23rd Conference of the European Network for Housing Research. Retrieved 2012-05-09.
- ↑ Hwang, Su-Lun; Hwang, Jing-Shiang; Yang, Yi-Ta; Hsieh, Wanhua A.; Chang, Tien-Chun; Guo, How-Ran; Tsai, Mong-Hsun; Tang, Jih-Luh et al. (2008). "Estimates of Relative Risks for Cancers in a Population after Prolonged Low-Dose-Rate Radiation Exposure: A Follow-up Assessment from 1983 to 2005". Radiation Research 170 (2): 143–8. doi:10.1667/RR0732.1. PMID 18666807.
- ↑ "Ultra-Low-Level Radiation Effects Summit." January 2006. ORION International Technologies, Inc. (ORION) and sponsored by the U.S. Department of Energy’s Waste Isolation Pilot Plant (WIPP) 03 Apr. 2008.
- ↑ http://www.orionint.com/ullre/report-2006.pdf[]
- ↑ Smith, Geoffrey Battle; Grof, Yair; Navarrette, Adrianne; Guilmette, Raymond A. (2011). "Exploring Biological Effects of Low Level Radiation from the Other Side of Background". Health Physics 100 (3): 263–5. doi:10.1097/HP.0b013e318208cd44. PMID 21595063.
- ↑ Capece, D.; Fratini, E. (2012). "The use of pKZ1 mouse chromosomal inversion assay to study biological effects of environmental background radiation". The European Physical Journal Plus 127 (4): 37. Bibcode:2012EPJP..127...37C. doi:10.1140/epjp/i2012-12037-7.
External links
- International Dose-Response Society. University of Massachusetts center for research on hormesis. Many papers on radiation hormesis.
- Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2
- Radiation Hormesis Overview by T. D. Luckey, who wrote a book on the subject (Luckey, T. D. (1991). Radiation Hormesis. Boca Raton, FL: CRC Press. ISBN 0-8493-6159-1)
- Brenner, David J.; Doll, Richard; Goodhead, Dudley T.; Hall, Eric J.; Land, Charles E.; Little, John B.; Lubin, Jay H.; Preston, Dale L. et al. (2003). "Cancer risks attributable to low doses of ionizing radiation: Assessing what we really know". Proceedings of the National Academy of Sciences 100 (24): 13761–6. Bibcode:2003PNAS..10013761B. doi:10.1073/pnas.2235592100. JSTOR 3148861. PMC 283495. PMID 14610281.
| ||||||||||||||||||||||||||||