Pleural effusion
| Pleural effusion | |
|---|---|
_CRUK_054.svg.png) Diagram of fluid buildup in the pleura | |
| Classification and external resources | |
| ICD-10 | J90-J91 |
| ICD-9 | 511.9 |
| MedlinePlus | 000086 |
| MeSH | D010996 |
Pleural effusion is excess fluid that accumulates in the pleural cavity, the fluid-filled space that surrounds the lungs. This excess can impair breathing by limiting the expansion of the lungs. Various kinds of pleural effusion, depending on the nature of the fluid and what caused its entry into the pleural space, are hydrothorax (serous fluid), hemothorax (blood), urinothorax (urine), chylothorax (chyle), or pyothorax (pus). Pneumothorax is the accumulation of air in the pleural space.
Types
Five types of fluids can accumulate in the pleural space:
- Serous fluid (hydrothorax)
- Blood (hemothorax)
- Chyle (chylothorax)
- Pus (pyothorax or empyema)
- Urine (urinothorax)
- John m.
Causes
Transudative
The most common causes of transudative pleural effusions in the United States are right ventricular failure, and cirrhosis (causing hepatic hydrothorax). Nephrotic syndrome leading to increased loss of albumin and resultant hypoalbuminemia and thus reducing colloid osmotic pressure is another less common cause. Pulmonary embolisms were once thought to be associated with transudative effusions but have been recently shown to be exudative[1] The mechanism for the exudative pleural effusion is probably related to increased permeability of the capillaries in the lung, which results from the release of cytokines or inflammatory mediators (e.g. vascular endothelial growth factor) from the platelet-rich thrombi. The excessive interstitial lung fluid traverses the visceral pleura and accumulates into the pleural space.
Conditions associated with transudative pleural effusions:[2]
- Congestive Heart Failure (CHF)
- Liver cirrhosis
- Hypoproteinemia
- Nephrotic syndrome
- Acute atelectasis
- Myxedema
- Peritoneal dialysis
- Meigs syndrome
- Obstructive uropathy
- End-stage kidney disease
Exudative
Once identified as exudative, additional evaluation is needed to determine the cause of the excess fluid, and pleural fluid amylase, glucose, pH and cell counts are obtained.
- Pleural fluid amylase is elevated in cases of esophageal rupture, pancreatic pleural effusion, or cancer.
- Glucose is decreased with cancer, bacterial infections, or rheumatoid pleuritis.
- Pleural fluid pH is low in empyema (<7.2) and may be low in cancer.
- If cancer is suspected, the pleural fluid is sent for cytology. If cytology is negative, and cancer is still suspected, either a thoracoscopy, or needle biopsy[3] of the pleura may be performed.
- The fluid is also sent for Gram staining and culture, and, if suspicious for tuberculosis, examination for TB markers (adenosine deaminase > 45 IU/L, interferon gamma > 140 pg/mL, or positive polymerase chain reaction (PCR) for tuberculous DNA).
The most common causes of exudative pleural effusions are bacterial pneumonia, cancer (with lung cancer, breast cancer, and lymphoma causing approximately 75% of all malignant pleural effusions), viral infection, and pulmonary embolism.
Conditions associated with exudative pleural effusions:[2]
- Malignancy
- Infection
- Trauma
- Pulmonary infarction
- Pulmonary embolism
- Autoimmune disorders
- Pancreatitis
- Ruptured esophagus ( or Boerhaave's syndrome)
- Rheumatoid Pleurisy
- Drug-induced Lupus
- Tuberculosis
Other/ungrouped
Other causes of pleural effusion include tuberculosis (though pleural fluid smears are rarely positive for AFB, this is the most common cause of pleural effusion in some developing countries), autoimmune disease such as systemic lupus erythematosus, bleeding (often due to chest trauma), chylothorax (most commonly caused by trauma), and accidental infusion of fluids.
Less common causes include esophageal rupture or pancreatic disease, intra-abdominal abscess, rheumatoid arthritis, asbestos pleural effusion, Mesothelioma, Meigs syndrome (ascites and pleural effusion due to a benign ovarian tumor), and ovarian hyperstimulation syndrome.
Pleural effusions may also occur through medical/surgical interventions, including the use of medications (pleural fluid is usually eosinophilic), coronary artery bypass surgery, abdominal surgery, endoscopic variceal sclerotherapy, radiation therapy, liver or lung transplantation, and intra- or extravascular insertion of central lines.
Pathophysiology
Pleural fluid is secreted by parietal layer of the pleura and reabsorbed by the lymphatics in the most dependent parts of the parietal pleura, primarily the diaphragmatic and mediastinal regions.
Diagnosis
Pleural effusion is usually diagnosed on the basis of medical history and physical exam, and confirmed by chest x-ray. Once accumulated fluid is more than 300 ml, there are usually detectable clinical signs in the patient, such as decreased movement of the chest on the affected side, stony dullness to percussion over the fluid, diminished breath sounds on the affected side, decreased vocal resonance and fremitus (though this is an inconsistent and unreliable sign), and pleural friction rub. Above the effusion, where the lung is compressed, there may be bronchial breathing and egophony. A large effusion there may cause tracheal deviation away from the effusion. A systematic review (2009) published as part of the Rational Clinical Examination Series in the Journal of the American Medical Association (JAMA) showed that dullness to conventional percussion was most accurate for diagnosing pleural effusion (summary positive likelihood ratio, 8.7; 95% confidence interval, 2.2–33.8), while the absence of reduced tactile vocal fremitus made pleural effusion less likely (negative likelihood ratio, 0.21; 95% confidence interval, 0.12–0.37).[4]
Imaging
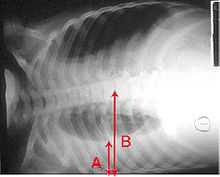
A pleural effusion will show up as an area of whiteness on a standard posteroanterior X-ray.[5] Normally the space between the two layers of the lung, the visceral pleura and the parietal pleura, cannot be seen. A pleural effusion infiltrates the space between these layers. Because the pleural effusion has a density similar to body fluid or water, it can be seen on radiographs. Since the effusion has greater density than the rest of the lung, it will gravitate towards the lower portions of the pleural cavity. The pleural effusion behaves according to basic fluid dynamics, conforming to the shape of the lung and chest cavity. If the pleural cavity contains both air and fluid, then the fluid will have a "fluid level" that is horizontal instead of conforming to the lung space.[6] Chest radiographs acquired in the lateral decubitus position (with the patient lying on his side) are more sensitive and can pick up as little as 50 ml of fluid. At least 300 ml of fluid must be present before upright chest films can pick up signs of pleural effusion (e.g., blunted costophrenic angles).
-

Massive left-sided pleural effusion (whiteness) in a patient presenting with lung cancer.
-

CT scan of chest showing left sided pleural effusion. Effusion fluid often settles at the lowest space due to gravity; here at the back as the patient is lying under scanner.
-
The lung expanding within an area of pleural effusion as seen by ultrasound
-

Micrograph of a pleural fluid cytopathology specimen showing malignant mesothelioma, one cause of a pleural effusion.
Thoracentesis
Once a pleural effusion is diagnosed, the cause must be determined. Pleural fluid is drawn out of the pleural space in a process called thoracentesis, and it should be done in almost all patients who have pleural fluid that is ≥ 10 mm in thickness on CT, ultrasonography, or lateral decubitus x-ray and that is new or of uncertain etiology. In general, the only patients who do not require thoracentesis are those who have heart failure with symmetric pleural effusions and no chest pain or fever; in these patients, diuresis can be tried, and thoracentesis avoided unless effusions persist for ≥ 3 days.[7] In thoracentesis, a needle is inserted through the back of the chest wall in the sixth, seventh, or eighth intercostal space on the midaxillary line, into the pleural space. The fluid may then be evaluated for the following:
- Chemical composition including protein, lactate dehydrogenase (LDH), albumin, amylase, pH, and glucose
- Gram stain and culture to identify possible bacterial infections
- Cell count and differential
- Cytopathology to identify cancer cells, but may also identify some infective organisms
- Other tests as suggested by the clinical situation – lipids, fungal culture, viral culture, specific immunoglobulins
Light's criteria
| Transudate vs. exudate | ||
|---|---|---|
| Transudate | Exudate | |
| Main causes | Increased hydrostatic pressure, Decreased colloid osmotic pressure |
Inflammation-Increased Vascular Permeability |
| Appearance | Clear[8] | Cloudy[8] |
| Specific gravity | < 1.012 | > 1.020 |
| Protein content | < 2.5 g/dL | > 2.9 g/dL[9] |
| fluid protein/ serum protein | < 0.5 | > 0.5[10] |
| Difference of albumin content with blood albumin | > 1.2 g/dL | < 1.2 g/dL[11] |
| fluid LDH upper limit for serum | < 0.6 or < 2⁄3 | > 0.6[9] or > 2⁄3[10] |
| Cholesterol content | < 45 mg/dL | > 45 mg/dL[9] |
Definitions of the terms "transudate" and "exudate" are the source of much confusion. Briefly, transudate is produced through pressure filtration without capillary injury while exudate is "inflammatory fluid" leaking between cells.
Transudative pleural effusions are defined as effusions that are caused by systemic factors that alter the pleural equilibrium, or Starling forces. The components of the Starling forces–hydrostatic pressure, permeability, and oncotic pressure (effective pressure due to the composition of the pleural fluid and blood)–are altered in many diseases, e.g., left ventricular failure, kidney failure, liver failure, and cirrhosis. Exudative pleural effusions, by contrast, are caused by alterations in local factors that influence the formation and absorption of pleural fluid (e.g., bacterial pneumonia, cancer, pulmonary embolism, and viral infection).[13]
An accurate diagnosis of the cause of the effusion, transudate versus exudate, relies on a comparison of the chemistries in the pleural fluid to those in the blood, using Light's criteria. According to Light's criteria (Light, et al. 1972), a pleural effusion is likely exudative if at least one of the following exists:[14]
- The ratio of pleural fluid protein to serum protein is greater than 0.5
- The ratio of pleural fluid LDH and serum LDH is greater than 0.6
- Pleural fluid LDH is greater than 0.6 [9] or 2⁄3[14] times the normal upper limit for serum. Different laboratories have different values for the upper limit of serum LDH, but examples include 200[15] and 300[15] IU/l.[16]
The sensitivity and specificity of Light's criteria for detection of exudates have been measured in many studies and are usually reported to be around 98% and 80%, respectively.[17][18] This means that although Light's criteria are relatively accurate, twenty percent of patients that are identified by Light's criteria as having exudative pleural effusions actually have transudative pleural effusions. Therefore, if a patient identified by Light's criteria as having an exudative pleural effusion appears clinically to have a condition that usually produces transudative effusions, additional testing is needed. In such cases albumin levels in blood and pleural fluid are measured. If the difference between the albumin level in the blood and the pleural fluid is greater than 1.2 g/dL (12 g/L), this suggests that the patient has a transudative pleural effusion.[11] However, pleural fluid testing is not perfect, and the final decision about whether a fluid is a transudate or an exudate is based not on chemical analysis of the fluid, but on accurate diagnosis of the disease that produces the fluid.
The traditional definitions of transudate as a pleural effusion due to systemic factors and an exudate as a pleural effusion due to local factors have been used since 1940 or earlier (Light et al., 1972). Previous to Light's landmark study, which was based on work by Chandrasekhar, investigators unsuccessfully attempted to use other criteria, such as specific gravity, pH, and protein content of the fluid, to differentiate between transudates and exudates. Light's criteria are highly statistically sensitive for exudates (although not very statistically specific). More recent studies have examined other characteristics of pleural fluid that may help to determine whether the process producing the effusion is local (exudate) or systemic (transudate). The chart to the right, illustrates some of the results of these more recent studies. However, it should be borne in mind that Light's criteria are still the most widely used criteria.
The Rational Clinical Examination Series review found that bilateral effusions, symmetric and asymmetric, are the most common distribution in heart failure (60% of effusions in heart failure will be bilateral). When there is asymmetry in heart failure-associated pleural effusions (either unilateral or one side larger than the other), the right side is usually more involved than the left.[4]
Treatment
Treatment depends on the underlying cause of the pleural effusion.
Therapeutic aspiration may be sufficient; larger effusions may require insertion of an intercostal drain (either pigtail or surgical). When managing these chest tubes, it is important to make sure the chest tubes do not become occluded or clogged. A clogged chest tube in the setting of continued production of fluid will result in residual fluid left behind when the chest tube is removed. This fluid can lead to complications such as hypoxia due to lung collapse from the fluid, or fibrothorax, later, when the space scars down. Repeated effusions may require chemical (talc, bleomycin, tetracycline/doxycycline), or surgical pleurodesis, in which the two pleural surfaces are scarred to each other so that no fluid can accumulate between them. This is a surgical procedure that involves inserting a chest tube, then either mechanically abrading the pleura or inserting the chemicals to induce a scar. This requires the chest tube to stay in until the fluid drainage stops. This can take days to weeks and can require prolonged hospitalizations. If the chest tube becomes clogged, fluid will be left behind and the pleurodesis will fail.
Pleurodesis fails in as many as 30% of cases. An alternative is to place a PleurX Pleural Catheter or Aspira Drainage Catheter. This is a 15Fr chest tube with a one-way valve. Each day the patient or care givers connect it to a simple vacuum tube and remove from 600 cc to 1000 cc of fluid. This can be repeated daily. When not in use, the tube is capped. This allows patients to be outside the hospital. For patients with malignant pleural effusions, it allows them to continue chemotherapy, if indicated. Generally, the tube is in for about 30 days and then it is removed when the space undergoes a spontaneous pleurodesis.
See also
References
- ↑ Porcel JM, Light RW (2008). "Pleural effusions due to pulmonary embolism.". Current Opinion in Pulmonary Medicine 14 (4): 337–42. doi:10.1097/MCP.0b013e3282fcea3c. PMID 18520269.
- ↑ 2.0 2.1 Galagan et al. Color Atlas of Body Fluids. CAP Press, Northfield, 2006
- ↑ de Menezes Lyra R (July 1997). "A modified outer cannula can help thoracentesis after pleural biopsy" (PDF). Chest 112 (1): 296. doi:10.1378/chest.112.1.296. PMID 9228404.
- ↑ 4.0 4.1 Wong CL, Holroyd-Leduc J, Straus SE (Jan 2009). "Does this patient have a pleural effusion?". JAMA 301 (3): 309–17. doi:10.1001/jama.2008.937. PMID 19155458.
- ↑ Corne et al. (2002). Chest X-Ray Made Easy. Churchill Livingstone. ISBN 0-443-07008-3.
- ↑ Squire, Lucy Frank; Novelline, Robert A. (2004). Squire's fundamentals of radiology. Cambridge: Harvard University Press. pp. 132–3. ISBN 0-674-01279-8.
- ↑ Light, Richard W. "Pleural Effusion". Merck Manual for Health Care Professionals. Merck Sharp & Dohme Corp. Retrieved 21 August 2013.
- ↑ 8.0 8.1 The University of Utah • Spencer S. Eccles Health Sciences Library > WebPath images > "Inflammation".
- ↑ 9.0 9.1 9.2 9.3 Heffner J, Brown L, Barbieri C (1997). "Diagnostic value of tests that discriminate between exudative and transudative pleural effusions. Primary Study Investigators". Chest 111 (4): 970–80. doi:10.1378/chest.111.4.970. PMID 9106577.
- ↑ 10.0 10.1 Light R, Macgregor M, Luchsinger P, Ball W (1972). "Pleural effusions: the diagnostic separation of transudates and exudates". Ann Intern Med 77 (4): 507–13. doi:10.7326/0003-4819-77-4-507. PMID 4642731.
- ↑ 11.0 11.1 Roth BJ, O'Meara TF, Gragun WH (1990). "The serum-effusion albumin gradient in the evaluation of pleural effusions". Chest 98 (3): 546–9. doi:10.1378/chest.98.3.546. PMID 2152757.
- ↑ de Menezes Lyra R (1997). "A modified outer cannula can help thoracentesis after pleural biopsy.". Chest 112 (1): 296. doi:10.1378/chest.112.1.296. PMID 9228404.
- ↑ Light, Richard W. "Ch. 257: Disorders of the Pleura and Mediastinum". In Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrison's Principles of Internal Medicine (17th ed.).
- ↑ 14.0 14.1 Light RW, Macgregor MI, Luchsinger PC, Ball WC (1972). "Pleural effusions: the diagnostic separation of transudates and exudates". Ann Intern Med 77 (4): 507–13. doi:10.7326/0003-4819-77-4-507. PMID 4642731.
- ↑ 15.0 15.1 Joseph J, Badrinath P, Basran GS, Sahn SA (November 2001). "Is the pleural fluid transudate or exudate? A revisit of the diagnostic criteria". Thorax 56 (11): 867–70. doi:10.1136/thorax.56.11.867. PMC 1745948. PMID 11641512.
- ↑ Joseph J, Badrinath P, Basran GS, Sahn SA (2002). "Is albumin gradient or fluid to serum albumin ratio better than the pleural fluid lactate dehydroginase in the diagnostic of separation of pleural effusion?". BMC Pulmonary Medicine 2: 1. doi:10.1186/1471-2466-2-1. PMC 101409. PMID 11914151.
- ↑ Romero S, Martinez A, Hernandez L, Fernandez C, Espasa A, Candela A, Martin C (2000). "Light's criteria revisited: consistency and comparison with new proposed alternative criteria for separating pleural transudates from exudates.". Respiration; international review of thoracic diseases 67 (1): 18–23. doi:10.1159/000029457. PMID 10705257.
- ↑ Porcel JM, Peña JM, Vicente de Vera C, Esquerda A (Feb 18, 2006). "[Reappraisal of the standard method (Light's criteria) for identifying pleural exudates].". Medicina clinica 126 (6): 211–3. doi:10.1157/13084870. PMID 16510093.
External links
- Pleural Effusion - Definition, Causes, Diagnosis and Treatment.
- MedlinePlus Encyclopedia Pleural Effusion
- Pleural Effusion Images from MedPix
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
