Pectus excavatum
| Pectus Excavatum | |
|---|---|
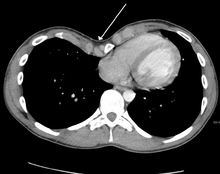
 An example of a severe case. | |
| Classification and external resources | |
| ICD-10 | Q67.6 |
| ICD-9 | 754.81 |
| OMIM | 169300 |
| DiseasesDB | 29401 |
| MedlinePlus | 003320 |
| eMedicine | ped/2558 |
| MeSH | D005660 |
Pectus excavatum (a Latin term meaning hollowed chest)[1] is the most common congenital deformity of the anterior wall of the chest, in which several ribs and the sternum grow abnormally. This produces a caved-in or sunken appearance of the chest.[2] It can either be present at birth or not develop until puberty.
Pectus excavatum is sometimes considered to be cosmetic; however, depending on the severity, it can impair cardiac and respiratory function and cause pain in the chest and back.[3] People with the condition may experience negative psychosocial effects, and avoid activities that expose the chest.[4]
Pectus excavatum is sometimes referred to as cobbler's chest, sunken chest, the crevasse, or funnel chest.[5][6]
Signs and symptoms
The hallmark of the condition is a sunken appearance of the sternum. The heart can be displaced and/or rotated. Mitral valve prolapse may also be present. Base lung capacity is decreased.[7]
Causes
Researchers are currently unsure as to the actual cause of pectus excavatum but hypothesize genetic defect.[3] Approximately 37% of individuals with pectus excavatum have a first degree family member with the condition.[2] Physiologically, increased pressure in utero, rickets and increased traction on the sternum due to abnormalities of the diaphragm have been postulated as specific mechanisms.[2] Pectus excavatum is also a relatively common symptom of Marfan syndrome[8] and sometimes is found in other connective tissue disorders such as Ehlers-Danlos Syndrome.[9] Many children with spinal muscular atrophy develop pectus excavatum due to the diaphragmatic breathing that is common with the disease. Pectus excavatum also occurs in about 1% of persons diagnosed with Celiac disease for unknown reasons.
Pathophysiology
Because the heart is located behind the sternum, and because individuals with pectus excavatum have been shown to have visible deformities of the heart (seen both on radiological imaging and after autopsies), it has been hypothesized that there is impairment of function of the cardiovascular system in individuals with pectus excavatum. While some studies have demonstrated decreased cardiovascular function in pectus excavatum, there has been no consensus reached based on newer physiological tests (such as echocardiography) of the presence or degree of impairment in cardiovascular function in people with pectus excavatum. Similarly, there is no consensus on the degree of functional improvement after corrective surgery.[2]
Diagnosis
Pectus excavatum is initially suspected from visual examination of the anterior chest. Auscultation of the chest can reveal displaced heart beat and valve prolapse. There can be a heart murmur occurring during systole caused by proximity between the sternum and the pulmonary artery.[10] Lung sounds are usually clear yet diminished due to decreased base lung capacity.[7]
Many scales have been developed to determine the degree of deformity in the chest wall. Most of these are variants on the distance between the sternum and the spine. One such index is the Backer ratio which grades severity of deformity based on the ratio between the diameter of the vertebral body nearest to xiphosternal junction and the distance between the xiphosternal junction and the nearest vertebral body.[11] More recently the Haller index has been used based on CT scan measurements. An index over 3.25 is often defined as severe.[12] The Haller index is the ratio between the horizontal distance of the inside of the ribcage and the shortest distance between the vertebrae and sternum.[13]

Chest x-rays are also useful in the diagnosis. The chest x-ray in pectus excavatum can show an opacity in the right lung area that can be mistaken for an infiltrate (such as that seen with pneumonia).[14] Some studies also suggest that the Haller index can be calculated based on chest x-ray as opposed to CT scanning in individuals who have no limitation in their function.[15]
Pectus excavatum is differentiated from other disorders by a series of elimination of signs and symptoms. Pectus carinatum is excluded by the simple observation of a collapsing of the sternum rather than a protrusion. Kyphoscoliosis is excluded by diagnostic imaging of the spine, where in pectus excavatum the spine usually appears normal in structure.
Treatment
Treatment for pectus excavatum can involve either invasive or non-invasive techniques or a combination of both. Before an operation proceeds several tests are usually to be performed. These include, but are not limited to, a CT scan, pulmonary function tests, and cardiology exams (such as auscultation and ECGs).[3] After a CT scan is taken the Haller index is measured. The patient's Haller is calculated by obtaining the ratio of the transverse diameter (the horizontal distance of the inside of the ribcage) and the anteroposterior diameter (the shortest distance between the vertebrae and sternum).[16] A Haller Index of greater than 3.25 is generally considered severe, while normal chest has an index of 2.5.[13][17][18] The cardiopulmonary tests are used to determine the lung capacity and to check for heart murmurs.
Vacuum bell
A relatively new alternative to surgery is the vacuum bell. It consists of a bowl shaped device which fits over the caved-in area; the air is then removed by the use of a hand pump.[19] The vacuum created by this lifts the sternum upwards, lessening the severity of the deformity.[20] Once the defect visually disappears, two additional years of use of the vacuum bell is required to make what may be a permanent correction.[21][22]
Orthopedics
Mild cases have also reportedly been treated with corset-like orthopedic support vests and exercise.[23][24]
Surgery
Surgical correction has been shown to repair any functional symptoms that may occur in the condition, such as respiratory problems or heart murmurs, provided that permanent damage has not already arisen from an extremely severe case.[3] One of the most popular technique for repair of pectus excavatum today is the minimally invasive operation, also known as MIRPE or Nuss technique.[25]
Ravitch technique
The Ravitch technique is an invasive surgery that was introduced in 1949,[26] and developed in the 1950s to treat the condition. This procedure involves creating an incision along the chest through which the cartilage is removed and the sternum detached. A small bar is then inserted underneath the sternum to hold it up in the desired position. The bar is left implanted until the cartilage grows back, typically about 6 months. The bar is subsequently removed in a simple out-patient procedure. The Ravitch technique is not widely practiced because it is so invasive. It is often used in older patients, where the sternum has calcified, when the deformity is asymmetrical, or when the less invasive Nuss procedure has proven unsuccessful.[27]
Nuss procedure


Dr. Donald Nuss, based at Children's Hospital of The King's Daughters in Norfolk, Virginia, developed in 1987[28] a technique that is minimally invasive.[29][30] The Nuss procedure involves slipping in one or more concave steel bars into the chest, underneath the sternum. The bar is flipped to a convex position so as to push outward on the sternum, correcting the deformity. The bar usually stays in the body for about two years, although many surgeons are now moving toward leaving them in for up to five years. When the bones have solidified into place, the bar is removed through outpatient surgery.
Taulinoplastia
Taulinoplastia utilizes a set of implants placed on the outer surface of the rib cage similar to the Nuss procedure. This procedure claims to accomplish the same benefits of the Nuss procedure with minimal blood loss, a shorter recovery period, no risk to internal organs, shorter surgical intervention, small incisions, and does not require intensive treatment or post operational tubes.[31]
Robicsek Technique
Dr. Francis Robicsek, based at Carolinas HealthCare System in Charlotte, NC developed the Robicsek procedure in 1965. Each time the procedure is performed, it is individually tailored based on the extent and location of the deformity in the patient. The operation begins with an incision, no more than 4-6 centimeters, to the sternum. The pectoralis major muscles are then detached from the sternum. Using the upper limit of the sternal depression as a guide, the deformed cartilages are removed one-by-one, using sharp and blunt dissection. The lower tip of the sternum is then grabbed with a towel-clip and, using blunt dissection, is freed of tissue connections with the pericardium and the pleura. The sternum is then forcefully bent forward into a corrected position.
To keep the sternum elevated, a piece of mesh is placed under the mobilized sternum and sutured under moderate tension bilaterally to the stumps of the ribs. After appropriate hemostasis, the pectoralis muscles are united in front of the sternum and the wound is closed without additional drainage. Any pressure-dressing should be avoided. [32] There has been controversy as to the best surgical approach for correction of pectus excavatum. It is important for the surgeon to select the appropriate operative approach based on each individual patient's characteristics.[33]
Cosmetic and light treatments
The cosmetic appearance of pectus excavatum can be treated with a dermal filler called Bio-Alcamid.[34] However, this does nothing to alleviate the actual deformity and will not prevent any physiological symptoms caused by the condition.
There are also prosthetic implants available to fill the depressed area. Solid silicone implants have been successfully used for many years with acceptable results in some cases.[35][36] More recently a porex implant has been used which is a similar material used to replace skull in brain surgery and severe head injuries.[37]
Magnetic mini-mover procedure
The magnetic mini-mover procedure (3MP) is a technique used to correct pectus excavatum by using two magnets to realign the sternum with the rest of the chest and ribcage.[38] One magnet is inserted 1 cm into the patient's body on the lower end of the sternum, the other is placed externally onto a custom fitted brace. These two magnets generate around 0.04 tesla (T) in order to slowly move the sternum outwards over a number of years. The maximum magnetic field that can be applied to the body safely is around 4 T, making this technique safe from a magnetic viewpoint.[38] The 3MP technique's main advantages are that it is more cost-effective than major surgical approaches such as the Nuss procedure and it is considerably less painful postoperatively.
Its effectiveness is limited to younger children in early- to mid-puberty because older patients have less compliant (flexible) chest walls.[39] One potential adverse interaction with other medical devices is possible inactivation of artificial pacemakers if present.
Laser Thermoplasty
Research has been conducted into the potential for utilizing laser thermoplasty to directly reshape the malformed costal cartilages thought to result in chest wall deformities. Ex vivo studies have been conducted with success but have not yet been translated to human studies.[40]
Epidemiology
Pectus excavatum occurs in an estimated 1 in 150-1000 births, with male predominance (male-to-female ratio of 3:1). Occurrences of the condition in family members have been reported in 35% to 45% of cases.[7][41]
Other animals
Pectus excavatum is also known to occur in animals, e.g. the Munchkin breed of cat.[42] Some procedures used to treat the condition in animals have not been used in human treatments, such as the use of a cast with sutures wrapped around the sternum and the use of internal and external splints.[43][44] These techniques are generally used in immature animals with flexible cartilage.[45]
First depiction by Leonardo da Vinci
Recently a surgeon at Imperial College London (Dr Hutan Ashrafian) has studied the anatomical images of Leonardo da Vinci from The Royal Collection to identify the first ever depiction of pectus excavatum by the famous artist.[46]
See also
References
- ↑ chief lexicographer: Douglas M. Anderson (2003). "Pectus Excavatum". Dorland's Medicla Dictionary (28 ed.). Philadelphia, Penns.: Saunders. ISBN 0-7216-0146-4.
- ↑ 2.0 2.1 2.2 2.3 Shamberger RC (1996). "Congenital chest wall deformities". Current Problems in Surgery 33 (6): 469–542. doi:10.1016/S0011-3840(96)80005-0. PMID 8641129.
- ↑ 3.0 3.1 3.2 3.3 Crump HW (1992). "Pectus excavatum". Am Fam Physician 46 (1): 173–9. PMID 1621629. Archived from the original on 2007-01-24.
- ↑ "Pectus excavatum". MedLine Plus Medical Encyclopedia. U.S. National Library of Medicine and the National Institutes of Health. 2007-11-12.
- ↑ "Pectus Excavatum".
- ↑ Spence, Roy A. J.; Patrick J. Morrison (2005). Genetics for Surgeons. Remedica Publishing. ISBN 1-901346-69-2.
- ↑ 7.0 7.1 7.2 "eMedicine — Pectus Excavatum". Andre Hebra.
- ↑ "eMedicine — Marfan Syndrome". Harold Chen.
- ↑ Creswick HA1, Stacey MW, Kelly RE Jr, Gustin T, Nuss D, Harvey H, Goretsky MJ, Vasser E, Welch JC, Mitchell K, Proud VK (October 2006). "Family study of the inheritance of pectus excavatum". Journal of Pediatric Surgery 41 (10): 1699–703. doi:10.1016/j.jpedsurg.2006.05.071. PMID 17011272.
- ↑ Guller B, Hable K (1974). "Cardiac findings in pectus excavatum in children: review and differential diagnosis". Chest 66 (2): 165–71. doi:10.1378/chest.66.2.165. PMID 4850886.
- ↑ BACKER OG, BRUNNER S, LARSEN V (1961). "The surgical treatment of funnel chest. Initial and follow-up results". Acta chirurgica Scandinavica 121: 253–61. PMID 13685690.
- ↑ Jeannette Diana-Zerpa; Nancy Thacz Browne; Laura M. Flanigan; Carmel A. McComiskey; Pam Pieper (2006). Nursing Care of the Pediatric Surgical Patient (Browne, Nursing Care of the Pediatric Surgical Patient). Sudbury, Mass: Jones & Bartlett Publishers. p. 253. ISBN 0-7637-4052-7.
- ↑ 13.0 13.1 Haller JA, Kramer SS, Lietman SA (1987). "Use of CT scans in selection of patients for pectus excavatum surgery: a preliminary report". Journal of Pediatric Surgery 22 (10): 904–6. doi:10.1016/S0022-3468(87)80585-7. PMID 3681619.
- ↑ Hoeffel JC, Winants D, Marcon F, Worms AM (1990). "Radioopacity of the right paracardiac lung field due to pectus excavatum (funnel chest)". Rontgenblatter 43 (7): 298–300. PMID 2392647.
- ↑ Mueller C, Saint-Vil D, Bouchard S (2008). "Chest x-ray as a primary modality for preoperative imaging of pectus excavatum". Journal of Pediatric Surgery 43 (1): 71–3. doi:10.1016/j.jpedsurg.2007.09.023. PMID 18206458.
- ↑ "How the Haller is measured. Departament of Cardiology and Pulmonology of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo – Thoracic Surgery Sector" (PDF).
- ↑ "The Nuss procedure for pectus excavatum correction | AORN Journal". Barbara Swoveland, Clare Medrick, Marilyn Kirsh, Kevin G. Thompson, Nussm Donald. 2001.
- ↑ "Pectus Excavatum overview" (PDF). CIGNA.
- ↑ chkd, Children's Hospital of the King's Daughters
- ↑ Haecker, FM; Mayr J (April 2006). "The vacuum bell for treatment of pectus excavatum: an alternative to surgical correction?". European Journal of Cardiothoracic Surgery 29 (4): 557–561. doi:10.1016/j.ejcts.2006.01.025. PMID 16473516.
- ↑ Non-surgical sunken chest treatment device may eliminate surgery, Mass Device, November 2012
- ↑ Raver-Lampman (November 2012), First patients in US receive non-surgical device of sunken chest syndrome, AAAS
- ↑ "LaceIT PE Brace". Advanced Orthotic Designs, Inc.
- ↑ "Orthopectus". Dr. Sydney A. Haje, Ortopedista.
- ↑ Hebra A (2009). "Minimally invasive repair of pectus excavatum". Semin Thorac Cardiovasc Surg 21 (1): 76–84. doi:10.1053/j.semtcvs.2009.04.005. PMID 19632566.
- ↑ Ravitch MM (April 1949). "The Operative Treatment of Pectus Excavatum". Ann Surg 129 (4): 429–44. doi:10.1097/00000658-194904000-00002. PMC 1514034. PMID 17859324.
- ↑ Theresa D. Luu MD (November 2009). "Surgery for Recurrent Pectus Deformities". The Annals of Thoracic Surgery 88 (5): 1627–1631. doi:10.1016/j.athoracsur.2009.06.008. PMID 19853122.
- ↑ Dr. Donald Nuss, Pioneer of the Nuss Procedure
- ↑ Nuss D, Kelly RE Jr, Croitoru DP, Katz ME (April 1998). "A 10-year review of a minimally invasive technique for the correction of pectus excavatum". J Pediatr Surg 33 (4): 545–52. doi:10.1016/S0022-3468(98)90314-1. PMID 9574749.
- ↑ Pilegaard, HK; Licht PB (February 2008). "Early results following the Nuss operation for pectus excavatum--a single-institution experience of 383 patients". Interactive Cardiovascular and Thoracic Surgery (Oxford University Press) 7 (1): 54–57. doi:10.1510/icvts.2007.160937. PMID 17951271. Retrieved 2008-04-18.
- ↑ http://www.venturamedicaltechnologies.com/en/productes/per-que-pectus-up.php
- ↑ Robiscek, Francis. "Marlex Mesh Support For The Correction Of Very Severe And Recurrent Pectus Excavatum" 26 (1). pp. 80–83.
- ↑ Robicsek, Hebra (2009). "To Nuss or not to Nuss? Two opposing views" 21 (1). pp. 85–88. doi:10.1053/j.semtcvs.2009.03.007. PMID 19632567.
- ↑ Lahiri, A; Waters R (February 2007). "Experience with Bio-Alcamid, a new soft tissue endoprosthesis". Journal of Plastic, Reconstructive & Aesthetic Surgery 60 (6): 663–667. doi:10.1016/j.bjps.2006.07.010. PMID 17485056.
- ↑ Saour S, Shaaban H, McPhail J, McArthur P (September 2007). "Customised silicone prostheses for the reconstruction of chest wall defects: technique of manufacture and final outcome". J Plast Reconstr Aesthet Surg 61 (10): 1205–9. doi:10.1016/j.bjps.2007.07.019. PMID 18178533. Retrieved 2008-08-21.
- ↑ Wechselberger G, Ohlbauer M, Haslinger J, Schoeller T, Bauer T, Piza-Katzer H (November 2001). "Silicone implant correction of pectus excavatum". Ann Plast Surg 47 (5): 489–93. doi:10.1097/00000637-200111000-00003. PMID 11716258. Retrieved 2008-08-21.
- ↑ Grappolini S, Fanzio PM, D'Addetta PG, Todde A, Infante M (January 2008). "Aesthetic treatment of pectus excavatum: a new endoscopic technique using a porous polyethylene implant". Aesthetic Plast Surg 32 (1): 105–10. doi:10.1007/s00266-007-9025-6. PMID 17851713.
- ↑ 38.0 38.1 Harrison, MR; Estefan-Ventura D et al. (January 2007). "Magnetic Mini-Mover Procedure for pectus excavatum: I. Development, design, and simulations for feasibility and safety" (PDF). Journal of Pediatric Surgery 42 (1): 81–85. doi:10.1016/j.jpedsurg.2006.09.042. PMID 17208545. Retrieved 2008-04-23.
- ↑ Harrison, MR; Michael R. Harrison; Kelly D. Gonzales; Barbara J. Bratton; Darrell Christensen; Patrick F. Curran; Richard Fechter; Shinjiro Hirose (January 2012). "Magnetic mini-mover procedure for pectus excavatum III: safety and efficacy in a Food and Drug Administration-sponsored clinical trial". Journal of Pediatric Surgery 47 (1): 154–9. doi:10.1016/j.jpedsurg.2011.10.039. PMID 22244409. Retrieved 2014-08-20.
- ↑ Sviridov, A. P.; Zakharkina, O. L., Ignatieva, N. Yu., Vorobieva, N. N., Bagratashvili, N. V., Plyakin, V. A., Kulik, I. O., Sarukhanyan, O. O., Minaev, V. P., Lunin, V. V. and Bagratashvili, V. N. (February 2014). "Ex vivo laser thermoplasty of whole costal cartilages.". Lasers Surg. Med. 46: 302–309. doi:10.1002/lsm.22233.
- ↑ "Pectus Excavatum: Frequently Asked Questions: Surgery: UI Health Topics". Harold M. Burkhart and Joan Ricks-McGillin.
- ↑ "Genetic Anomalies of Cats".
- ↑ Fossum, TW; Boudrieau RJ; Hobson HP; Rudy RL (1989). "Surgical correction of pectus excavatum, using external splintage in two dogs and a cat". Journal of the American Veterinary Medical Association 195 (1): 91–7. PMID 2759902.
- ↑ Risselada M, de Rooster H, Liuti T, Polis I, van Bree H (2006). "Use of internal splinting to realign a noncompliant sternum in a cat with pectus excavatum". Journal of the American Veterinary Medical Association 228 (7): 1047–52. doi:10.2460/javma.228.7.1047. PMID 16579783.
- ↑ McAnulty JF, Harvey CE (1989). "Repair of pectus excavatum by percutaneous suturing and temporary external coaptation in a kitten". Journal of the American Veterinary Medical Association 194 (8): 1065–7. PMID 2651373.
- ↑ Ashrafian, Hutan. (2013). "Leonardo da Vinci and the first portrayal of pectus excavatum". Thorax. doi:10.1136/thoraxjnl-2013-203224.
External links
| Wikimedia Commons has media related to Pectus excavatum. |
| Look up pectus in Wiktionary, the free dictionary. |
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||